That familiar clicking or popping sound when you chew, yawn, or speak can be unsettling. For many, it’s a minor annoyance that comes and goes. But for others, it may signal an underlying issue affecting the temporomandibular joint (TMJ), the hinge connecting your jawbone to your skull. While occasional jaw popping is common and often harmless, persistent or painful symptoms warrant attention. Understanding the causes, risks, and treatment options empowers you to make informed decisions about your oral and overall health.
Understanding the Jaw Joint: The TMJ Explained
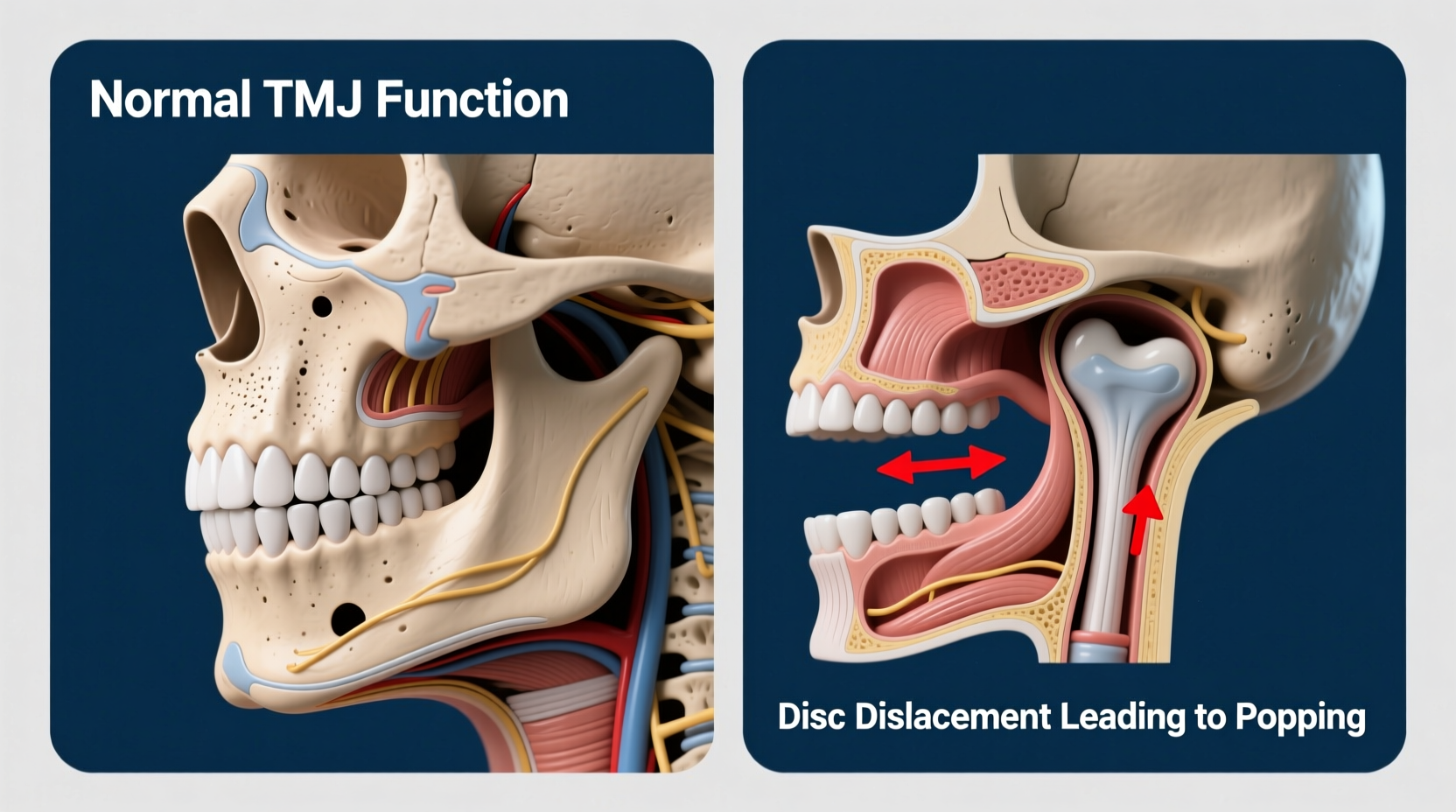
The temporomandibular joint is one of the most complex joints in the human body. It allows your jaw to move up and down, side to side, and forward and back—essential motions for chewing, speaking, and swallowing. Each TMJ consists of a rounded mandibular condyle that fits into the temporal bone’s articular fossa, cushioned by a small disc of cartilage that acts as a shock absorber during movement.
When this disc becomes displaced, inflamed, or worn, or when the surrounding muscles and ligaments are strained, the joint may not glide smoothly. This dysfunction can lead to audible sounds like popping, clicking, or grinding—collectively known as crepitus. These noises occur when the disc snaps back into place or when bone rubs against bone due to reduced cushioning.
“Over 10 million Americans experience some form of TMJ disorder, and jaw popping is often the first symptom patients report.” — Dr. Alan Kim, Oral and Maxillofacial Specialist
Common Causes of Jaw Popping During Chewing
Jaw popping isn’t always a sign of serious trouble. In fact, many people experience it without pain or long-term consequences. However, several factors can contribute to the condition:
- Misaligned bite (malocclusion): When teeth don’t meet evenly, uneven pressure on the jaw joint can lead to strain and popping.
- TMJ disorders (TMD): A broad category of conditions affecting jaw function, including disc displacement, arthritis, or muscle tension.
- Bruxism (teeth grinding or clenching): Often occurs at night and places excessive force on the TMJ, leading to inflammation and joint instability.
- Arthritis: Osteoarthritis or rheumatoid arthritis can degrade the joint cartilage, causing friction and noise.
- Injury or trauma: A blow to the jaw or whiplash can dislocate the joint or damage the disc.
- Stress-related tension: Emotional stress leads to tightened facial and jaw muscles, increasing pressure on the TMJ.
- Excessive gum chewing or wide yawning: Repetitive or extreme jaw movements can temporarily irritate the joint.
When Should You Be Concerned?
Not all jaw popping requires medical intervention. If the sound is infrequent, painless, and doesn’t limit your jaw movement, it may simply be a mechanical quirk with no clinical significance. However, certain red flags indicate it’s time to consult a dentist or specialist:
- Pain in the jaw, face, neck, or ears during chewing or speaking
- Difficulty opening or closing your mouth fully
- Jaw locking—either open or closed position
- Frequent headaches or migraines, especially upon waking
- Swelling on the side of the face near the joint
- Symptoms that worsen over time or interfere with daily life
Left untreated, chronic TMD can lead to degenerative changes in the joint, chronic pain, and even permanent mobility issues. Early assessment improves outcomes significantly.
Do’s and Don’ts for Managing Jaw Popping
| Do’s | Don’ts |
|---|---|
| Eat soft foods to reduce joint strain | Avoid hard, crunchy, or chewy foods (e.g., nuts, bagels, taffy) |
| Apply warm compresses to relax muscles | Don’t rest your chin on your hand or bite nails |
| Practice gentle jaw stretches (if recommended) | Don’t yawn widely or chew gum excessively |
| Manage stress through meditation or breathing exercises | Don’t ignore persistent pain or limited motion |
| Use a prescribed night guard if you grind your teeth | Don’t self-diagnose or delay professional evaluation |
Diagnosis and Treatment Options
If symptoms persist, a dentist or TMJ specialist will perform a comprehensive evaluation. This may include:
- Physical examination of jaw movement and tenderness
- Dental impressions to assess bite alignment
- Imaging tests such as X-rays, CT scans, or MRI to visualize the joint structure
Based on findings, treatment plans are tailored to the individual. Most cases respond well to conservative, non-invasive approaches.
Step-by-Step Guide to Initial Relief
- Modify your diet: Switch to soft foods like soups, yogurt, mashed potatoes, and smoothies for 5–7 days to minimize joint stress.
- Apply heat: Use a warm, moist towel on the affected side for 10–15 minutes, 2–3 times daily to ease muscle tension.
- Practice jaw rest: Keep your teeth slightly apart, not touching, except when eating or swallowing. This reduces clenching.
- Manage stress: Engage in relaxation techniques like deep breathing, yoga, or mindfulness meditation to lower muscle tension.
- Try over-the-counter pain relief: NSAIDs like ibuprofen can reduce inflammation and discomfort (consult your doctor first).
- Schedule a dental check-up: Even if symptoms improve, a professional assessment ensures there’s no underlying structural issue.
For more advanced cases, additional interventions may be recommended:
- Occlusal splints or night guards: Custom-fitted devices worn at night to prevent grinding and reposition the jaw.
- Physical therapy: Targeted exercises to strengthen jaw muscles and improve range of motion.
- Dental correction: Orthodontics or restorative work to correct bite imbalances.
- Injections: Corticosteroids or Botox may be used in severe cases to reduce inflammation or relax overactive muscles.
- Surgery: Reserved for rare, debilitating cases where conservative treatments fail and structural damage is evident.
“Most TMJ issues resolve within weeks with simple lifestyle adjustments. Surgery is needed in less than 5% of diagnosed cases.” — Dr. Lena Torres, Orofacial Pain Specialist
Real-Life Example: Sarah’s Journey with Jaw Popping
Sarah, a 34-year-old graphic designer, began noticing a loud pop in her right jaw every time she chewed on that side. At first, it didn’t hurt, so she ignored it. Over three months, the popping became painful, especially in the mornings. She also started experiencing dull headaches behind her eyes.
After reading about TMJ online, she realized she had been clenching her jaw unconsciously during work hours and grinding her teeth at night. Her dentist confirmed moderate TMD and fitted her with a custom night guard. She also adopted stress-reduction practices and switched to a softer diet.
Within six weeks, the popping decreased significantly, and the pain disappeared. “I had no idea how much tension I was holding in my jaw,” Sarah said. “Now I do daily stretches and keep my shoulders relaxed. My jaw hasn’t popped in over two months.”
Frequently Asked Questions
Is jaw popping dangerous?
Occasional, painless popping is usually not dangerous and may result from normal joint mechanics. However, if accompanied by pain, limited movement, or worsening symptoms, it could indicate TMJ dysfunction and should be evaluated.
Can poor posture affect my jaw?
Yes. Forward head posture, often seen in people who spend long hours at computers, alters neck and jaw alignment. This increases strain on the TMJ and can contribute to popping and discomfort. Maintaining ergonomic posture supports jaw health.
Will jaw popping go away on its own?
In many cases, yes—especially if triggered by temporary factors like stress, minor injury, or overuse. However, if the cause is structural (like disc displacement) or habitual (like bruxism), it may persist without intervention.
Prevention Checklist: Protect Your Jaw Long-Term
Preventing recurrence starts with consistent habits. Use this checklist to maintain optimal jaw function:
- ✅ Avoid chewing gum and hard foods regularly
- ✅ Practice stress management techniques daily
- ✅ Maintain good posture, especially while working
- ✅ Visit your dentist annually for TMJ screening
- ✅ Wear a night guard if you grind your teeth
- ✅ Stay hydrated—dehydration can increase muscle tension
- ✅ Perform gentle jaw stretches if approved by a professional
Final Thoughts: Listen to Your Body
Your jaw is designed for thousands of movements each day. When it starts sending signals—like popping, pain, or stiffness—it’s worth paying attention. While many cases of jaw popping are benign and self-limiting, dismissing persistent symptoms can lead to avoidable complications. Simple changes in diet, posture, and stress levels often make a dramatic difference. But when in doubt, professional guidance is invaluable.
Don’t wait for pain to escalate. Whether it’s a routine dental visit or a referral to a TMJ specialist, taking proactive steps today can preserve your comfort and function for years to come.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?