Liver pain is not always straightforward. Unlike a sprained ankle or a headache, discomfort from the liver can be subtle, diffuse, or mistaken for digestive issues. The liver itself doesn’t have pain receptors, but the capsule surrounding it—the Glisson’s capsule—does. When this membrane stretches due to inflammation, swelling, or enlargement, it triggers discomfort typically felt in the upper right abdomen. Recognizing the signs early and understanding when to act can make a critical difference in long-term health outcomes.
Understanding Liver Pain: Location and Sensation
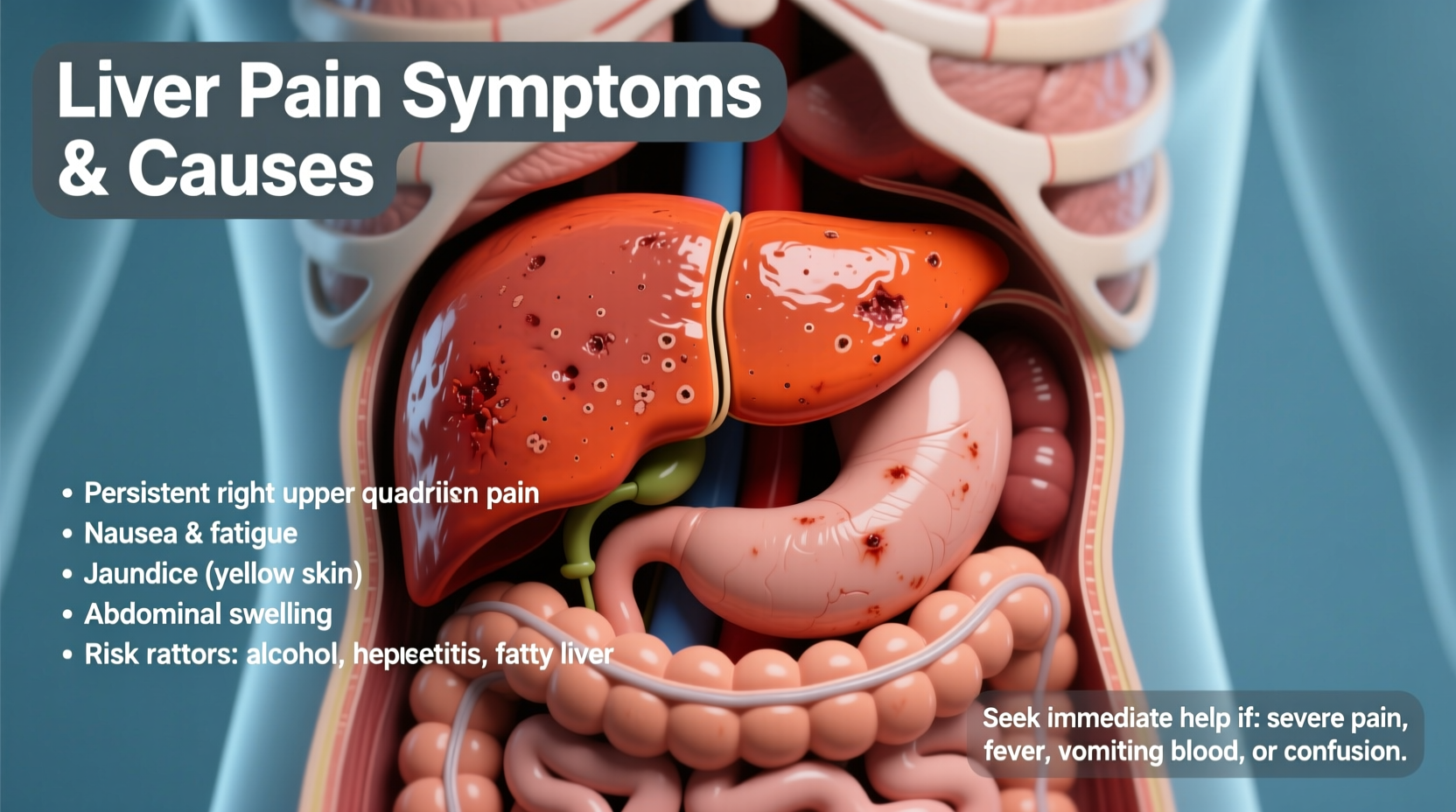
Liver-related discomfort is usually felt in the upper right quadrant of the abdomen, just below the rib cage. It may present as a dull ache, a feeling of fullness, or a sharp, localized pain—especially if there’s rapid organ enlargement or associated complications like gallstones.
Because the liver plays a central role in digestion, detoxification, protein synthesis, and metabolism, any disruption can manifest through a range of systemic symptoms. These often appear before overt pain develops, making early recognition essential.
Common Symptoms Associated with Liver Dysfunction
Pain alone isn’t enough to diagnose liver trouble. More telling are combinations of symptoms that suggest impaired liver function. Key indicators include:
- Fatigue and unexplained weakness
- Nausea or loss of appetite
- Jaundice (yellowing of skin or eyes)
- Dark urine and pale stools
- Abdominal swelling (ascites)
- Easy bruising or bleeding
- Itchy skin without rash
- Spider angiomas (small, spider-like blood vessels visible under the skin)
These symptoms arise because the liver struggles to process bilirubin, produce clotting factors, metabolize fats, or filter toxins effectively. As damage progresses, symptoms intensify and may become irreversible.
“Many patients don’t realize they have liver disease until it’s advanced. That’s why symptom awareness and routine blood work are so important.” — Dr. Lena Torres, Hepatologist at Cleveland Clinic
Major Causes of Liver Pain and Damage
Liver pain is rarely caused by a single factor. Instead, it results from conditions that inflame, scar, or obstruct the liver. Below are the most common culprits:
| Condition | Description | Key Risk Factors |
|---|---|---|
| Fatty Liver Disease (NAFLD/NASH) | Buildup of fat in liver cells leading to inflammation; most common cause in Western countries. | Obesity, insulin resistance, high cholesterol, sedentary lifestyle |
| Alcoholic Liver Disease | Chronic alcohol use damages liver tissue, progressing from fatty liver to cirrhosis. | Heavy drinking (more than 2 drinks/day for men, 1 for women) |
| Viral Hepatitis (A, B, C) | Infections causing acute or chronic liver inflammation. | Contaminated food/water (A), blood exposure/sex (B, C), IV drug use |
| Cirrhosis | Scarring of the liver from long-term damage; reduces function and increases pressure in veins. | Untreated hepatitis, alcohol abuse, fatty liver progression |
| Liver Abscess or Tumor | Less common but serious—can be benign or cancerous growths pressing on the capsule. | Chronic infection, genetic predisposition, toxin exposure |
| Gallbladder Disease | Often confused with liver pain; gallstones can block bile ducts shared with the liver. | High-fat diet, rapid weight loss, female gender, age over 40 |
Each condition affects the liver differently, but all share the potential to stretch the liver capsule and trigger pain. For example, someone with undiagnosed non-alcoholic steatohepatitis (NASH) might experience mild, intermittent discomfort after meals while showing no other obvious signs—until significant fibrosis develops.
When to Seek Medical Help: Red Flags and Timelines
Not every case of abdominal discomfort requires emergency care, but certain symptoms demand prompt evaluation. Delaying diagnosis in liver conditions can lead to permanent damage or life-threatening complications such as liver failure or portal hypertension.
Immediate Warning Signs (Seek Help Within 24–48 Hours)
- Yellowing of skin or eyes (jaundice)
- Sudden, severe upper right abdominal pain
- Swollen, tense abdomen with difficulty breathing
- Confusion, drowsiness, or slurred speech (signs of hepatic encephalopathy)
- Vomiting blood or passing black, tarry stools
If you notice any of these, contact your healthcare provider immediately or go to the nearest emergency department. These indicate advanced liver dysfunction or complications requiring urgent intervention.
Non-Urgent But Concerning Symptoms (Schedule Appointment Within 1 Week)
- Mild, recurring discomfort under the right ribs
- Unexplained fatigue lasting more than two weeks
- Loss of appetite with weight loss
- Itchy skin without allergy explanation
- Consistently elevated liver enzymes on blood tests
Even if symptoms seem minor, chronic low-grade liver stress can progress silently. A primary care physician can order liver function tests (ALT, AST, ALP, bilirubin), imaging (ultrasound, FibroScan), or refer you to a gastroenterologist or hepatologist.
Mini Case Study: Recognizing Silent Progression
Mark, a 47-year-old office worker, began noticing he felt bloated and slightly tender on his right side after dinner. He assumed it was acid reflux and took antacids. Over six months, the discomfort became more frequent. He also felt unusually tired and noticed his whites of his eyes looked yellowish.
After encouragement from his wife, he visited his doctor. Blood work revealed elevated ALT and AST levels. An ultrasound showed moderate fatty infiltration and mild liver enlargement. Further testing confirmed non-alcoholic steatohepatitis (NASH).
With dietary changes, weight loss, and regular monitoring, Mark reversed early-stage liver damage. His story underscores how easily liver issues can be overlooked—and how timely action can prevent serious outcomes.
Action Plan: What to Do If You Suspect Liver Trouble
If you’re experiencing possible liver-related symptoms, follow this step-by-step guide:
- Track your symptoms: Note location, duration, triggers (e.g., food, alcohol), and associated signs like fatigue or nausea.
- Review your habits: Assess alcohol intake, medication use (including supplements), diet, and exercise patterns.
- Request lab tests: Ask your doctor for a comprehensive metabolic panel focusing on liver enzymes and bilirubin.
- Get imaging if needed: Ultrasound is often first-line; FibroScan assesses liver stiffness (fibrosis).
- Consult a specialist: A hepatologist or gastroenterologist can provide targeted evaluation and management.
- Implement lifestyle changes: Reduce alcohol, adopt a Mediterranean-style diet, increase physical activity, and avoid liver-toxic substances.
Checklist: Protect Your Liver Daily
- ✅ Limit alcohol to moderate levels (or abstain if advised)
- ✅ Avoid unnecessary medications and herbal supplements (some are hepatotoxic)
- ✅ Eat whole grains, vegetables, lean proteins, and healthy fats
- ✅ Maintain a healthy weight and manage blood sugar
- ✅ Practice safe sex and avoid sharing needles to prevent hepatitis B/C
- ✅ Get vaccinated for hepatitis A and B if not already immune
- ✅ Use protective gear when handling chemicals or solvents
Frequently Asked Questions
Can liver pain come and go?
Yes. Early-stage liver disease may cause intermittent discomfort, especially after eating fatty foods or drinking alcohol. However, episodic pain doesn’t mean the condition is harmless—ongoing damage can still occur.
Is liver pain worse at night?
Some people report increased discomfort when lying down, particularly on the back. This may be due to internal pressure or heightened awareness at rest. Elevating the torso slightly may help temporarily, but addressing the root cause is essential.
Can stress cause liver pain?
Stress doesn't directly damage the liver, but chronic stress can worsen unhealthy behaviors like poor diet, alcohol use, or medication noncompliance, which indirectly affect liver health. Stress also influences inflammation pathways in the body.
Conclusion: Listen to Your Body—Your Liver Can’t Wait
Liver pain is not normal. While the organ may tolerate years of abuse silently, once symptoms appear, they signal that something is wrong. Whether it's fatty liver, alcohol-related damage, or an infection, early detection dramatically improves outcomes. You don’t need dramatic symptoms to take action—tracking subtle changes, advocating for testing, and adjusting lifestyle choices now can preserve liver function for decades.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?