Many people experience a popping or cracking sound in their lower back when they stand up after sitting or lying down. For some, it happens daily without discomfort; for others, it’s accompanied by stiffness, pain, or concern about long-term damage. While occasional joint noise is typically harmless, understanding the underlying causes—and recognizing warning signs—can help prevent more serious spinal problems.
This article explores the science behind joint cavitation, common reasons for lower back cracking, risk factors, and clear guidelines on when this symptom warrants medical attention. Whether you're an office worker, athlete, or someone managing chronic back discomfort, this guide offers practical insights grounded in biomechanics and clinical expertise.
The Science Behind Joint Cracking
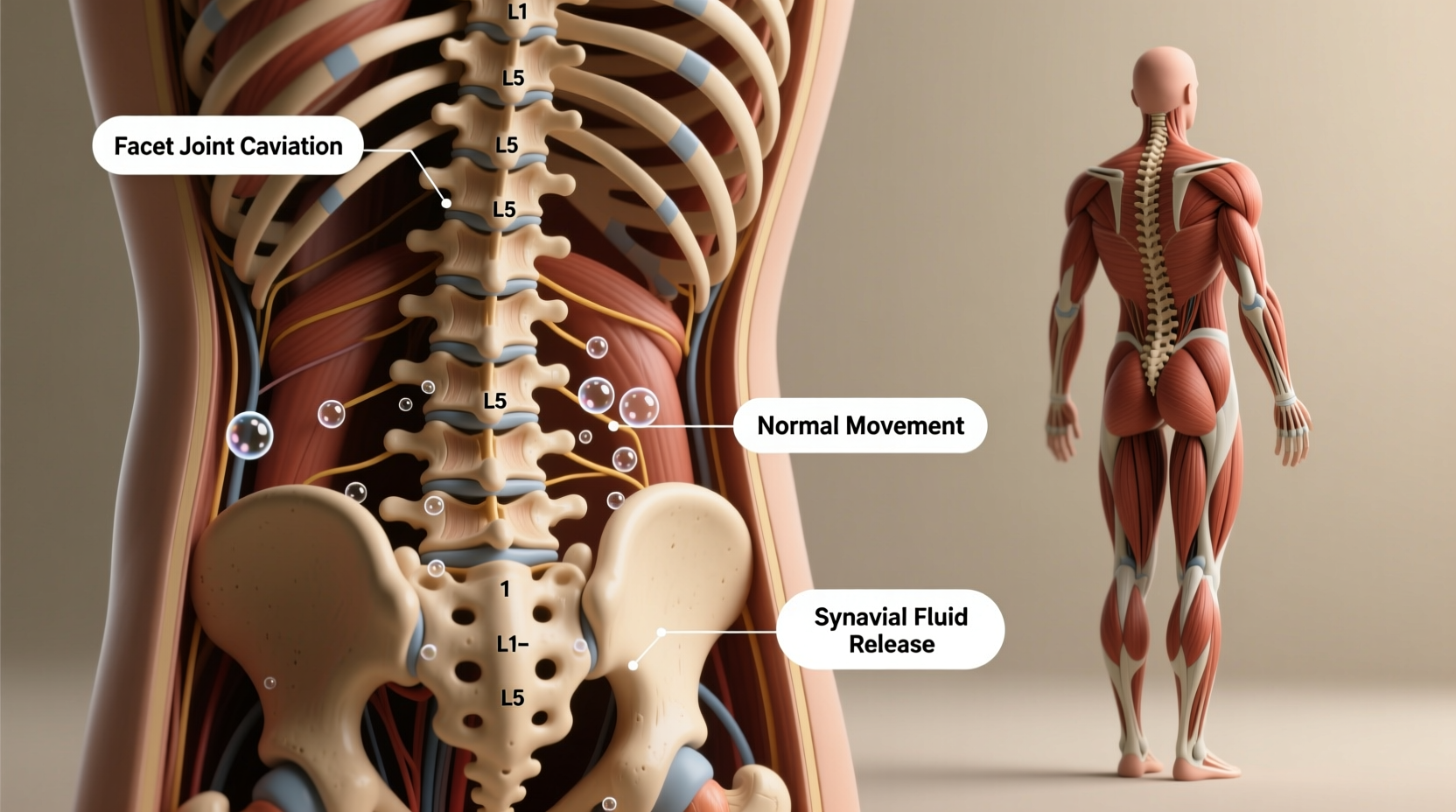
The sound of a \"crack\" in your lower back isn’t bones grinding together—it’s usually the result of a process called *cavitation*. When pressure changes rapidly within a synovial joint (such as those in the spine), dissolved gases like nitrogen, oxygen, and carbon dioxide form tiny bubbles in the synovial fluid. These bubbles collapse quickly, producing the familiar pop or snap.
Spinal facet joints, located at the back of each vertebra, are particularly prone to this phenomenon. When you transition from sitting to standing, subtle shifts in posture can create just enough movement to trigger gas release in these small joints.
“The audible pop during joint movement is almost always benign if it occurs without pain. It’s similar to cracking your knuckles—mechanical, not pathological.” — Dr. Alan Kim, Board-Certified Spine Physiatrist
Cavitation alone doesn't cause harm. In fact, studies show no link between habitual joint cracking and arthritis. However, repeated forceful manipulation or cracking associated with pain may indicate other structural or functional issues.
Common Causes of Lower Back Cracking When Standing
Not all joint noises are created equal. The context in which your back cracks matters significantly. Here are the most frequent explanations:
- Postural Shifts: After prolonged sitting, spinal joints compress slightly. Standing restores natural curvature, causing minor realignment and possible gas release.
- Muscle Tightness: Tight hip flexors or hamstrings pull on the pelvis, altering lumbar alignment. This tension can increase stress on facet joints, making them more likely to pop during motion.
- Reduced Joint Lubrication: With age or inactivity, synovial fluid production may decrease, increasing friction and the likelihood of audible joint movement.
- Minor Misalignments (Subluxations): Chiropractors often describe slight vertebral shifts that resolve with movement. These can produce a satisfying pop but aren’t necessarily harmful.
- Scar Tissue or Adhesions: Previous injuries or inflammation can lead to fibrous tissue buildup around joints, creating resistance that releases audibly upon movement.
When Cracking May Signal a Problem
While isolated, pain-free cracking is normal, certain patterns suggest underlying pathology. Pay close attention to frequency, accompanying symptoms, and functional limitations.
Red flags include:
- Pain during or immediately after the crack
- Swelling or warmth around the area
- Loss of mobility or range of motion
- Numbness, tingling, or radiating pain into the legs
- Instability or feeling like your back might \"give out\"
- Cracking that becomes louder, more frequent, or localized to one spot
Repetitive cracking due to hypermobility syndromes (like Ehlers-Danlos) can also contribute to early degenerative changes. In such cases, the joints move beyond their normal range, stressing ligaments and accelerating wear.
Conditions Linked to Symptomatic Back Cracking
| Condition | Description | Symptoms Beyond Cracking |
|---|---|---|
| Facet Joint Osteoarthritis | Wear-and-tear of spinal facet joints leading to cartilage loss | Stiffness, localized tenderness, worse pain with extension |
| Herniated Disc | Disc material pressing on nerves due to rupture or bulge | Leg pain (sciatica), numbness, muscle weakness |
| Spondylolisthesis | One vertebra slips forward over another | Lower back pain, tight hamstrings, possible nerve compression |
| Sacroiliac Joint Dysfunction | Abnormal motion in the SI joint connecting spine to pelvis | Pain in buttock or groin, worsened by climbing stairs |
| Ankylosing Spondylitis | Inflammatory arthritis affecting the spine and sacroiliac joints | Chronic morning stiffness lasting >30 minutes, fatigue, systemic inflammation |
Mini Case Study: Office Worker with Recurring Back Pops
Mark, a 38-year-old software developer, began noticing loud cracking in his lower back every time he stood from his desk chair. Initially, it didn’t hurt—but after several months, he started experiencing dull aching and occasional sharp twinges. He also felt increasingly stiff in the mornings.
After visiting a physical therapist, Mark learned that poor ergonomics—his chair lacked lumbar support, and his monitor was too low—had led to chronic slouching. This altered his spinal alignment, placing extra strain on his L4-L5 facet joints. Over time, this increased mechanical stress caused repetitive micro-movements and joint irritation.
With guided postural correction, ergonomic adjustments, and targeted core strengthening exercises, Mark reduced both the cracking frequency and discomfort within six weeks. His case highlights how seemingly minor habits can compound into noticeable musculoskeletal effects.
Step-by-Step Guide to Assessing and Managing Back Cracking
If you're concerned about your back cracking, follow this structured approach to determine whether self-care is sufficient or professional evaluation is needed.
- Monitor Symptoms Daily: Keep a simple log noting when cracking occurs, intensity of sound, presence of pain, and any triggers (e.g., standing, twisting).
- Evaluate Pain Pattern: Is the pain sharp, dull, burning? Does it radiate? Use a scale from 1–10 to track severity.
- Perform Basic Mobility Tests: Try touching your toes, rotating your torso, and bending sideways. Note any asymmetry or restriction.
- Improve Daily Habits: Adjust workstation setup, avoid prolonged sitting, incorporate walking breaks, and practice neutral spine posture.
- Try Conservative Care: Apply heat for stiffness, ice for acute pain, and perform gentle mobility drills like cat-cow stretches or pelvic tilts.
- Seek Professional Help If: Pain persists beyond two weeks, worsens, or interferes with sleep or activity.
Checklist: When to See a Doctor
Use this checklist to decide if your symptoms require medical evaluation:
- ✅ Cracking is consistently painful
- ✅ You feel instability or \"catching\" in your back
- ✅ Numbness, tingling, or weakness develops in one or both legs
- ✅ Bowel or bladder control changes occur (urgent red flag)
- ✅ Pain wakes you at night or fails to improve with rest
- ✅ History of trauma, osteoporosis, or inflammatory disease
- ✅ Symptoms persist longer than 2–3 weeks despite self-care
Fulfilling even one of these criteria warrants consultation with a healthcare provider such as a primary care physician, orthopedic specialist, or physical therapist.
FAQ: Common Questions About Lower Back Cracking
Is it bad to crack my back every day?
Daily cracking without pain is generally not harmful. However, deliberately forcing your back to crack using twisting motions or excessive pressure can strain muscles and ligaments over time. Letting your body move naturally through full-range activities like yoga or swimming is safer than aggressive manipulation.
Can dehydration cause more joint noise?
Yes. Synovial fluid relies on adequate hydration to maintain viscosity and cushion joints. Chronic dehydration may reduce lubrication efficiency, potentially increasing audible joint movements. Drinking sufficient water supports overall joint health.
Should I go to a chiropractor for back cracking?
If your cracking is painless, routine chiropractic care isn't necessary. However, if you have discomfort, restricted motion, or recurring misalignment sensations, a licensed chiropractor or physical therapist can assess joint function and provide appropriate treatment. Always choose providers who use evidence-based methods and avoid those pushing unnecessary long-term plans.
Prevention Strategies for Long-Term Spinal Health
Maintaining a resilient lower back involves consistent lifestyle choices. Consider these foundational practices:
- Core Strengthening: A strong transverse abdominis and multifidus muscles stabilize the spine and reduce abnormal joint loading.
- Flexibility Work: Regular stretching of hip flexors, hamstrings, and glutes prevents compensatory strain on the lumbar region.
- Proper Lifting Mechanics: Bend at the hips and knees, keep objects close to your body, and engage your core when lifting.
- Weight Management: Excess body weight increases mechanical stress on spinal structures, especially in the lower back.
- Active Recovery: Incorporate low-impact activities like walking, swimming, or cycling to promote circulation and joint nutrition.
“Spinal health isn’t about avoiding movement—it’s about moving well. Controlled, varied motion nourishes discs and keeps joints supple.” — Dr. Lena Torres, Physical Therapist & Spine Specialist
Conclusion: Listen to Your Body, Act with Confidence
Occasional lower back cracking when standing is a normal part of human biomechanics. It reflects the dynamic nature of your spine responding to gravity and posture changes. But your body communicates through more than just sound—pain, stiffness, and functional changes are signals worth interpreting.
By understanding what’s typical versus concerning, you empower yourself to take timely action. Small adjustments in posture, movement habits, and self-awareness can preserve spinal health for decades. And when uncertainty arises, don’t hesitate to consult a qualified professional. Early intervention often prevents minor issues from becoming chronic conditions.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?