It’s a familiar sensation: stepping outside into the crisp winter air and almost immediately feeling a drip at the tip of your nose. You reach for a tissue, wondering why your body reacts so strongly to cold temperatures. This phenomenon—known medically as cold-induced rhinorrhea—is surprisingly common, yet often misunderstood. While many assume it's just a quirk of winter, persistent or worsening symptoms may point to something more, such as underlying allergies. Understanding the science behind this reaction and recognizing when it could be more than just cold air can help you manage discomfort and maintain better respiratory health.
The Science Behind a Runny Nose in Cold Weather
When cold, dry air enters your nasal passages, your body responds with a series of physiological changes designed to protect your lungs. The primary goal is to warm and humidify the air before it reaches your sensitive lower airways. To do this, your nasal membranes increase mucus production. Blood vessels in the nose dilate (a process called vasodilation), boosting blood flow and stimulating glands that secrete fluid. This excess mucus is what leads to the familiar \"runny nose\" in chilly conditions.
This reaction is entirely normal and serves a protective function. In fact, it’s a sign that your nasal system is doing its job. However, not everyone experiences it to the same degree. Some people have more reactive nasal linings or pre-existing sensitivities that amplify the response.
“Cold air is both dry and irritating to the nasal mucosa. The nose compensates by producing more mucus to condition the air—this is a natural defense mechanism.” — Dr. Lena Peterson, Otolaryngologist
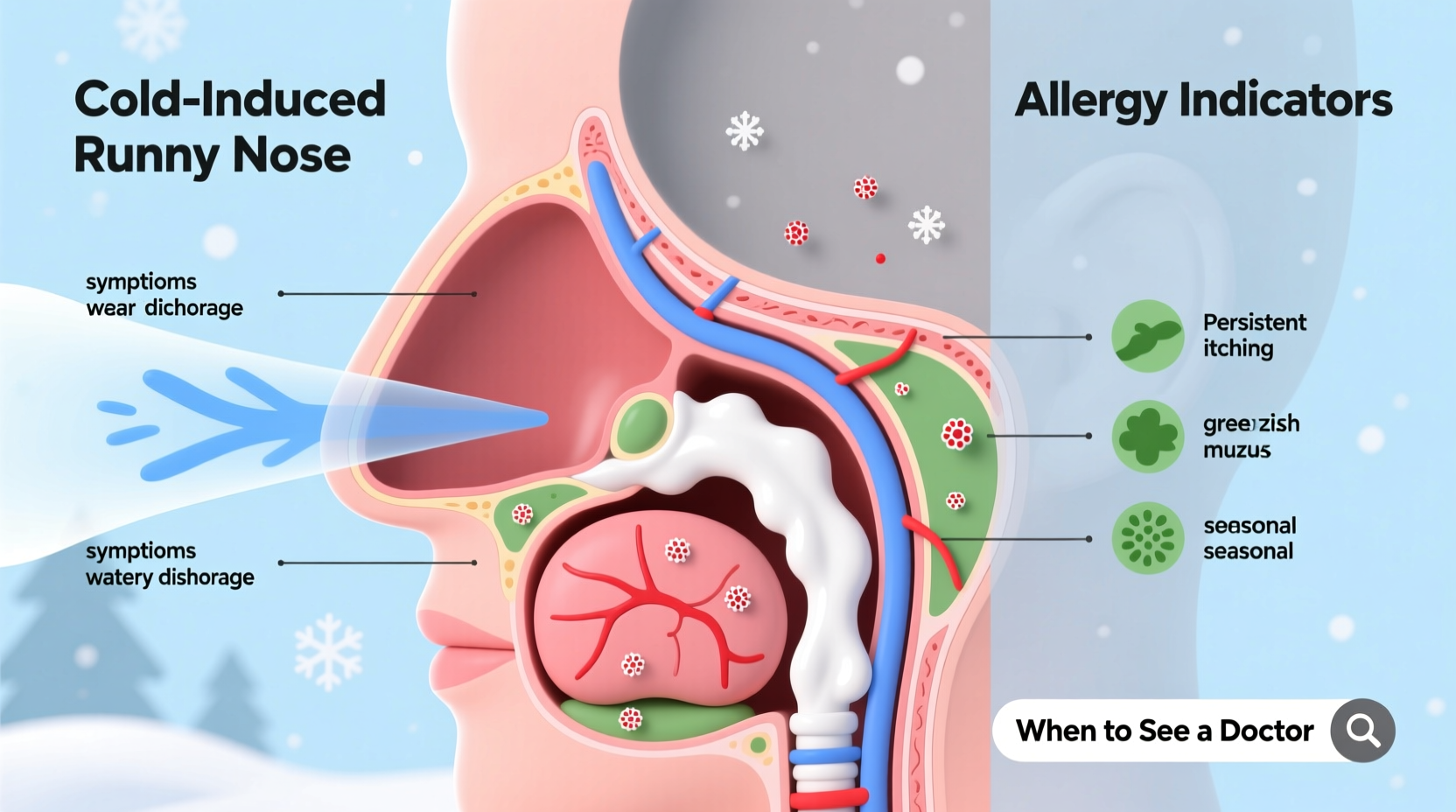
Distinguishing Between Cold-Induced Rhinorrhea and Allergies
While a runny nose in cold weather is typically harmless, similar symptoms can also stem from allergies—especially if they persist beyond exposure to cold air. Recognizing the differences is crucial for proper management.
Allergic rhinitis, commonly triggered by indoor allergens like dust mites, pet dander, or mold, often worsens during winter months when people spend more time indoors with limited ventilation. Unlike cold-induced rhinorrhea, which occurs only during or shortly after cold exposure, allergy symptoms tend to be continuous or recurrent regardless of temperature.
Key distinguishing factors include:
- Timing: Cold-related drips happen mainly outdoors in cold air and subside quickly indoors. Allergy symptoms persist across environments.
- Nasal discharge: Cold weather typically causes clear, watery mucus. Allergies may produce thicker mucus, though still usually clear.
- Accompanying symptoms: Itching, sneezing fits, postnasal drip, and eye irritation are more indicative of allergies.
- Duration: Cold-induced symptoms last minutes to hours. Allergy symptoms can last days or weeks without intervention.
Situations When a Runny Nose Might Signal Allergies
A nose that runs only in cold weather is usually benign. But certain red flags suggest an allergic component:
- Symptoms continue indoors: If your nose runs even after warming up, especially in heated rooms, consider allergens like dust or pet dander.
- Seasonal recurrence: If the same symptoms return every winter without infection, it may be perennial allergic rhinitis.
- Family history of allergies: Genetic predisposition increases the likelihood of environmental sensitivities.
- No improvement with basic protection: Wearing scarves or using humidifiers helps with cold-induced symptoms but won’t resolve allergy-driven ones.
In some cases, cold air itself can trigger non-allergic rhinitis with eosinophilia syndrome (NARES) or exacerbate asthma in allergic individuals. These conditions mimic allergies but lack an immune-mediated IgE response, making diagnosis more complex.
Mini Case Study: Sarah’s Winter Symptoms
Sarah, a 34-year-old teacher, noticed her nose ran every time she walked to school in winter. She assumed it was just the cold. But over two seasons, she began experiencing congestion, itchy eyes, and fatigue—especially on days with high indoor heating. After consulting an allergist, skin testing revealed sensitivity to dust mites, which thrive in warm, dry bedrooms during winter. Her “cold weather” runny nose was actually allergy-driven, worsened by temperature shifts. With antihistamines and improved bedroom hygiene, her symptoms dropped significantly—even on freezing mornings.
Do’s and Don’ts: Managing Nasal Symptoms in Winter
| Do’s | Don’ts |
|---|---|
| Use a scarf to cover your nose and mouth – warms incoming air and reduces nasal irritation. | Ignore persistent symptoms – ongoing drainage may need medical evaluation. |
| Run a humidifier indoors – adds moisture to dry heated air, easing nasal passages. | Overuse decongestant sprays – can lead to rebound congestion if used more than 3 days. |
| Stay hydrated – thin mucus is easier to clear and less irritating. | Assume all runny noses are “just cold air” – especially if other allergy signs are present. |
| Wash bedding weekly in hot water – reduces exposure to dust mites during winter months. | Smoke or expose yourself to secondhand smoke – irritates nasal lining and worsens symptoms. |
Step-by-Step Guide to Assessing Your Winter Runny Nose
If you're unsure whether your symptoms are due to cold air or allergies, follow this practical assessment process:
- Observe the timing: Does your nose run only when outside in cold air? Or does it continue after coming inside?
- Note associated symptoms: Track sneezing, itching, congestion, or eye irritation over a week.
- Modify your environment: Use a humidifier, change furnace filters, and wash pillows/bedding.
- Try a trial of antihistamine: Over-the-counter options like loratadine or cetirizine can reduce allergy symptoms within 24–48 hours if allergies are involved.
- Consult a healthcare provider: If symptoms persist beyond two weeks or interfere with daily life, see an ENT specialist or allergist for testing.
This structured approach helps differentiate between temporary irritation and chronic conditions requiring treatment.
When to Seek Medical Advice
Most cases of cold-induced rhinorrhea require no medical intervention. However, professional evaluation is recommended if you experience any of the following:
- Thick yellow or green nasal discharge lasting more than 10 days (possible sinus infection)
- Facial pain or pressure
- Fever accompanying nasal symptoms
- Blood-tinged mucus regularly
- Symptoms disrupting sleep or daily activities
An allergist may perform skin prick tests or specific IgE blood tests to confirm sensitivities. For non-allergic rhinitis, diagnosis is often based on exclusion and symptom history.
Expert Insight: The Role of Environment and Immunity
Cold weather doesn’t cause illness, but it can weaken local immune defenses in the nasal cavity. Research shows that cooler nasal temperatures reduce the antiviral response, making individuals more susceptible to infections. This effect, combined with increased indoor crowding and low humidity, creates ideal conditions for both viral spread and allergic flare-ups.
“The nose is our first line of defense. When it’s constantly irritated—whether by cold, dry air or allergens—it becomes more vulnerable to secondary issues like infections.” — Dr. Raj Mehta, Immunology Researcher
Therefore, maintaining nasal health isn't just about comfort—it's a key part of overall wellness during colder months.
Practical Tips for Daily Relief
Whether your runny nose stems from cold exposure or allergies, these strategies can provide relief:
- Use saline nasal sprays: Helps moisturize dry nasal passages and flush out irritants.
- Invest in a HEPA air purifier: Reduces airborne allergens in living spaces.
- Keep indoor humidity between 40–50%: Prevents drying of mucous membranes without promoting mold growth.
- Avoid sudden temperature changes: Transition gradually between cold outdoor and warm indoor environments when possible.
- Shower before bed: Removes allergens collected on hair and skin during the day.
FAQ
Can cold weather directly cause a cold or flu?
No, colds and flu are caused by viruses, not cold temperatures. However, cold, dry air can impair nasal immunity and increase susceptibility to viral infections. Additionally, people tend to gather indoors more during winter, facilitating virus transmission.
Is it possible to be allergic to cold air?
True “cold allergy” (cold urticaria) is rare and typically causes hives, swelling, or systemic reactions—not just a runny nose. Most people reacting to cold air are experiencing non-allergic rhinitis, not an immunoglobulin-mediated allergy.
Why does my nose run more on windy days?
Wind increases evaporation from the nasal lining, drying it out and triggering reflexive mucus production. It can also carry allergens like pollen or mold spores, even in winter, potentially aggravating allergic individuals.
Conclusion: Take Control of Your Winter Nasal Health
A runny nose in cold weather is usually a natural, temporary response—but it shouldn’t be dismissed outright. By paying attention to patterns, managing your environment, and understanding when symptoms may point to allergies, you gain control over your comfort and health. Simple habits like covering your face outdoors, using a humidifier, and tracking symptoms can make a significant difference. If uncertainty persists, don’t hesitate to consult a healthcare provider. Your nose is more than a passage for air—it’s a finely tuned filter and protector of your respiratory system. Treat it with care, especially when the thermometer drops.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?