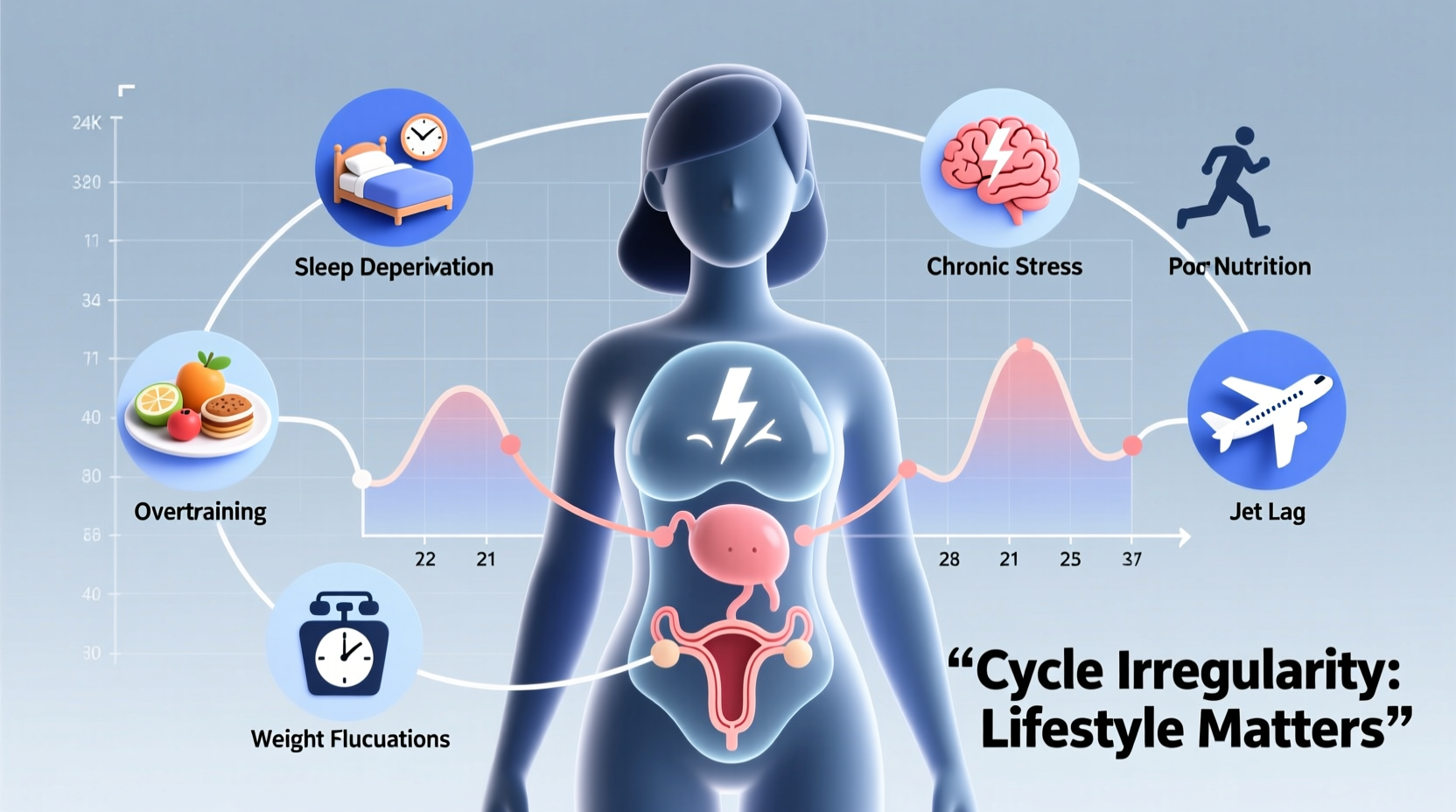
The menstrual cycle is often portrayed as a precise 28-day rhythm, but in reality, variation is normal—and common. Many people experience shifts in their cycle length, flow, or timing from month to month. While occasional irregularity is typically not a cause for concern, frequent or unpredictable changes can be frustrating and sometimes signal underlying imbalances. Although hormones like estrogen and progesterone regulate the cycle, they are highly sensitive to external influences. Lifestyle factors—ranging from stress levels to sleep quality and physical activity—play a significant role in shaping when your period arrives, how long it lasts, and what symptoms you experience.
Understanding the connection between daily habits and hormonal health empowers individuals to make informed choices that support cycle regularity and overall well-being. This article explores the most impactful lifestyle elements that influence menstrual timing, backed by medical insights and practical strategies for greater predictability.
How the Menstrual Cycle Works: A Quick Overview
The average menstrual cycle lasts about 28 days, though anywhere from 21 to 35 days is considered within the normal range. It consists of four key phases:
- Menstruation (Days 1–5): The shedding of the uterine lining if pregnancy hasn’t occurred.
- Follicular Phase (Days 1–13): Follicle-stimulating hormone (FSH) prompts the ovaries to mature an egg.
- Ovulation (Day 14, roughly): Luteinizing hormone (LH) surges, triggering the release of the egg.
- Luteal Phase (Days 15–28): The corpus luteum produces progesterone to prepare the uterus for potential implantation.
When any part of this process is disrupted—especially ovulation—the entire cycle can shift. Hormonal fluctuations don't occur in isolation; they're influenced by signals from the brain, particularly the hypothalamus, which acts as the body’s command center for reproductive function. And that command center responds directly to environmental and behavioral cues.
Stress: The Silent Cycle Disruptor
Chronic stress is one of the most common causes of irregular periods. When the body perceives stress—whether emotional, psychological, or physical—it activates the hypothalamic-pituitary-adrenal (HPA) axis. This system releases cortisol, the primary stress hormone, which interferes with the production of gonadotropin-releasing hormone (GnRH). Without adequate GnRH, the cascade of FSH and LH needed for ovulation falters.
In practical terms, this means prolonged work pressure, relationship strain, financial anxiety, or even overexercising can delay or suppress ovulation, leading to late or missed periods. Acute stress might only cause minor delays, but ongoing stress can result in anovulatory cycles (cycles without ovulation), making prediction nearly impossible.
“Even non-reproductive stressors—like final exams or moving cities—can delay menstruation by disrupting the brain’s signaling to the ovaries.” — Dr. Lena Patel, Reproductive Endocrinologist
Sleep Patterns and Circadian Rhythm
Sleep isn’t just restorative—it’s hormonally regulatory. The circadian clock, governed by light exposure and routine, influences the timing of melatonin and cortisol release, both of which interact with reproductive hormones. Irregular sleep schedules, night-shift work, or chronic insomnia have been linked to shorter luteal phases and anovulation.
A 2020 study published in Human Reproduction found that women who slept less than six hours per night were significantly more likely to report irregular cycles compared to those averaging seven to eight hours. Poor sleep also exacerbates stress and insulin resistance, compounding its effect on cycle stability.
Blue light exposure at night—common with late-night screen use—suppresses melatonin, which plays a role in follicular development. Consistently going to bed and waking up at different times each day confuses the body’s internal clock, potentially throwing off ovulation timing.
Key Sleep Hygiene Tips for Cycle Regulation
- Maintain a consistent bedtime and wake-up time, even on weekends.
- Limit screen time one hour before bed.
- Keep your bedroom cool, dark, and quiet.
- Avoid caffeine after 2 p.m.
Nutrition and Body Weight: Fueling Hormonal Balance
Diet profoundly affects menstrual regularity. Both undernutrition and overnutrition can disrupt hormonal signaling. Rapid weight loss, extreme calorie restriction, or eating disorders like anorexia nervosa often lead to amenorrhea (absence of periods) because the body interprets low energy availability as an unsuitable environment for reproduction.
Conversely, excess body fat increases estrogen production since adipose tissue converts androgens into estrogen. This can lead to heavier, more frequent periods or conditions like polycystic ovary syndrome (PCOS), where elevated insulin and androgen levels interfere with ovulation.
Micronutrient deficiencies—especially iron, vitamin D, and B vitamins—also play a role. Low iron may contribute to fatigue and poor ovarian response, while vitamin D deficiency is associated with PCOS and infertility.
| Nutritional Factor | Impact on Cycle | Action Step |
|---|---|---|
| Severe Calorie Deficit | Suppresses GnRH, halting ovulation | Ensure adequate caloric intake for activity level |
| High Sugar/Refined Carb Intake | Spikes insulin, worsens PCOS symptoms | Choose complex carbs and balanced meals |
| Low Healthy Fat Intake | Hinders steroid hormone production | Include omega-3s, nuts, avocado, olive oil |
| Vitamin D Deficiency | Linked to irregular ovulation | Get sunlight or consider supplementation |
Exercise: Finding the Sweet Spot
Physical activity benefits menstrual health—but only up to a point. Moderate exercise improves insulin sensitivity, reduces stress, and helps maintain a healthy weight, all of which support regular cycles. However, excessive exercise without sufficient recovery or fueling can have the opposite effect.
Female athlete triad—a condition involving disordered eating, amenorrhea, and bone loss—is a recognized consequence of high-intensity training combined with low energy availability. Even recreational exercisers who drastically increase running mileage or gym sessions may notice delayed periods due to energy imbalance.
The key is balance. For most people, 30–60 minutes of moderate activity most days of the week supports cycle health. Signs that exercise may be too intense include:
- Frequent missed or very light periods
- Increased injury rate or persistent fatigue
- Difficulty recovering between workouts
Mini Case Study: Sarah’s Story
Sarah, a 29-year-old graphic designer, noticed her periods became unpredictable after starting a new job with tight deadlines. She was sleeping five hours a night, surviving on takeout, and began intense daily HIIT workouts to “decompress.” Within three months, her once-regular 27-day cycle stretched to 38 days, then skipped entirely.
After consulting her gynecologist, she learned her lifestyle had created a perfect storm of stress, poor nutrition, and overtraining. With guidance, she reduced workouts to four moderate sessions per week, prioritized sleep, and started meal prepping balanced lunches. Within two months, her cycles returned to a consistent 26–28 day pattern.
Environmental and Behavioral Influences
Beyond the core pillars of stress, sleep, diet, and exercise, other lifestyle factors subtly shape cycle regularity:
- Travel and Time Zone Changes: Jet lag disrupts circadian rhythms, potentially delaying ovulation.
- Caffeine and Alcohol: High caffeine intake (>400mg/day) may increase estrogen levels; alcohol affects liver metabolism of hormones.
- Smoking: Associated with earlier menopause and shorter cycles due to ovarian toxicity.
- Endocrine Disruptors: Chemicals in plastics, cosmetics, and pesticides (like BPA and phthalates) mimic estrogen and may interfere with natural hormone function.
While these factors may not cause dramatic shifts alone, their cumulative effect over time can contribute to cycle variability.
Checklist: Lifestyle Factors That May Be Affecting Your Cycle
- ☑️ Have I experienced major stress recently?
- ☑️ Am I consistently getting less than 7 hours of sleep?
- ☑️ Has my weight changed significantly in the past 3 months?
- ☑️ Am I exercising more than 6 times per week at high intensity?
- ☑️ Do I skip meals or follow restrictive diets?
- ☑️ Am I exposed to environmental toxins (e.g., plastic containers, synthetic fragrances)?
- ☑️ Have I traveled across time zones lately?
When to Seek Medical Advice
While lifestyle factors explain many cases of irregular periods, some underlying conditions require medical evaluation. See a healthcare provider if you experience:
- Periods that are consistently shorter than 21 days or longer than 35 days
- No period for more than 90 days (and not pregnant)
- Extremely heavy bleeding (soaking through a pad/tampon every hour)
- Severe pain during menstruation
- Sudden onset of irregularity after years of regular cycles
Potential diagnoses include PCOS, thyroid disorders, hyperprolactinemia, or premature ovarian insufficiency. Blood tests, ultrasounds, and cycle tracking can help determine the cause.
FAQ
Can birth control masks lifestyle-related cycle issues?
Yes. Hormonal contraceptives override the natural cycle, creating artificial bleeds. While effective for managing symptoms, they can hide underlying irregularities. After stopping birth control, it may take several months for natural cycles to reestablish.
How long does it take for lifestyle changes to improve cycle regularity?
Most people see improvements within 2–3 months. Hormonal shifts require time, especially if ovulation has been suppressed. Consistency with sleep, diet, and stress management is key.
Is it normal for cycles to change with age?
Yes. In the teens, cycles often stabilize over several years. In the late 30s and 40s, declining ovarian reserve leads to shorter cycles and eventual perimenopause. But sudden unexplained changes at any age warrant attention.
Conclusion: Taking Control of Your Cycle Health
Your menstrual cycle is more than a biological function—it’s a vital sign of overall health. Random date changes aren’t always random; they’re often messages from your body responding to how you live, eat, move, and rest. By tuning into these signals and adjusting lifestyle factors thoughtfully, you can foster greater cycle predictability and long-term hormonal resilience.
You don’t need perfection—just consistency. Small, sustainable changes in sleep, stress management, nutrition, and movement add up. Track your cycles mindfully, honor your body’s needs, and seek professional support when necessary. Your period shouldn’t be a mystery. With awareness and action, it can become a reliable reflection of your well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?