Many people experience a frustrating phenomenon: their skin feels perfectly fine during the day but erupts into relentless itching as soon as they lie down to sleep. This nocturnal itch can disrupt rest, lead to skin damage from scratching, and even affect mood and daytime function. While occasional nighttime irritation is normal, persistent or worsening itch demands attention. The causes are often multifactorial—ranging from environmental influences to internal biological rhythms and underlying health conditions. Understanding why your skin itches only at night is the first step toward effective relief.
The Science Behind Nighttime Itch Intensification
Your body undergoes several physiological changes after dark that can amplify skin sensitivity. One major factor is the natural fluctuation of cortisol, an anti-inflammatory hormone. Cortisol levels drop in the evening, reducing your body’s ability to suppress inflammatory responses—including those that trigger itch. At the same time, core body temperature rises slightly at night, increasing blood flow to the skin and potentially stimulating nerve endings involved in itch perception.
Additionally, your brain becomes more attuned to internal sensations when external stimuli decrease. During the day, distractions like work, conversation, and movement help divert attention from minor discomforts. But in the quiet of bedtime, the absence of sensory competition allows subtle itch signals to dominate your awareness.
“Nighttime pruritus isn’t just psychological—it’s rooted in real shifts in neurobiology and immune activity,” says Dr. Lena Patel, dermatology researcher at the National Skin Health Institute. “The body’s circadian rhythm plays a significant role in how we perceive itch.”
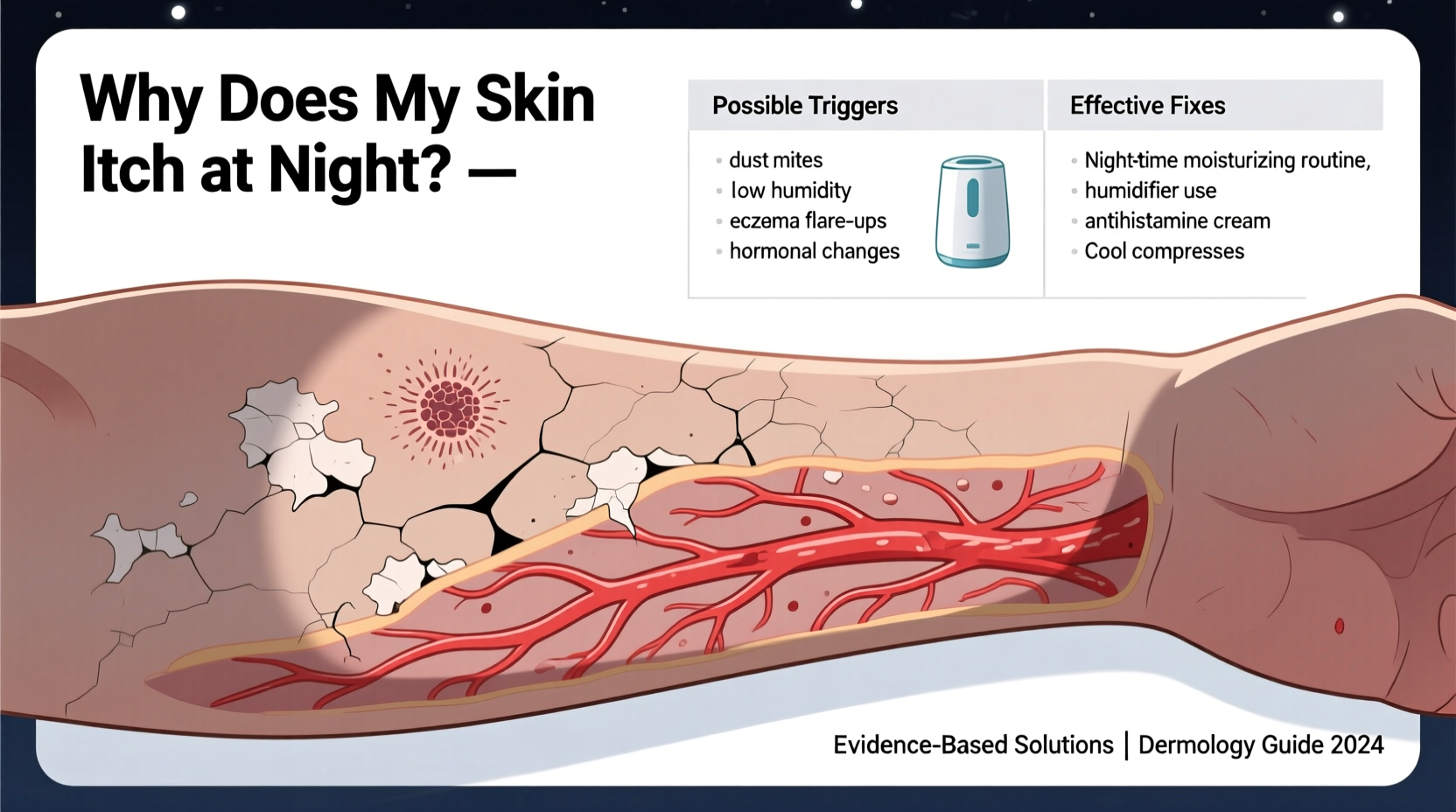
Common Triggers of Nighttime Itching
Numerous factors contribute to nocturnal itching. Some are environmental, others stem from skin conditions, and a few relate to systemic health. Identifying the root cause is essential for targeted treatment.
Dry Skin (Xerosis)
One of the most frequent culprits, especially in colder months, is dry skin. Indoor heating reduces humidity, stripping moisture from the air and your skin. As natural oil production slows at night, the skin barrier weakens, leading to tightness, flaking, and itchiness—particularly on arms, legs, and torso.
Allergens in Bedding
Your mattress, sheets, and pillows can harbor allergens such as dust mites, mold spores, pet dander, and laundry detergent residues. These irritants come into prolonged contact with your skin during sleep, triggering localized or widespread itching. Synthetic fabrics may also trap heat and moisture, exacerbating irritation.
Skin Conditions
Certain dermatological disorders flare at night due to biological rhythms or behavioral patterns:
- Eczema (Atopic Dermatitis): Inflammation worsens in low-humidity environments and when cortisol dips.
- Psoriasis: Though not always itchy, plaques can become irritated at night, especially if scratched unconsciously.
- Lichen Simplex Chronicus: A cycle of scratch-itch-scratch often intensifies during sleep, leading to thickened, leathery skin patches.
Infestations
Parasitic infestations like scabies are notorious for causing severe nighttime itching. The female mite burrows into the skin to lay eggs, and the immune response peaks at night. Common sites include between fingers, wrists, elbows, and genital areas. Bed bugs also feed at night, leaving clusters of red, itchy bites—though this is technically an allergic reaction to saliva rather than direct infestation of the skin.
Hormonal and Systemic Causes
Internal medical conditions can manifest through skin symptoms. These include:
- Liver disease: Bile salt buildup leads to generalized pruritus, often worse at night.
- Kidney failure: Accumulation of waste products in advanced stages causes intense itching.
- Diabetes: Nerve damage (neuropathy) and poor circulation can produce burning or tingling sensations.
- Thyroid disorders: Both hyper- and hypothyroidism are linked to dry, itchy skin.
Medication Side Effects
Some drugs list pruritus as a side effect. Opioids, certain antibiotics, antifungals, and statins are known to induce itching. If you started a new medication around the time symptoms began, consult your doctor before making any changes.
Do’s and Don’ts: Managing Nighttime Itch
| Do | Don't |
|---|---|
| Moisturize within 3 minutes of showering to lock in hydration | Use hot water for baths or long showers |
| Wear loose, breathable pajamas made of cotton or bamboo | Scratch with nails—use palm or knuckles if needed |
| Keep bedroom humidity between 40–60% using a humidifier | Sleep in synthetic fabrics or wool next to skin |
| Apply fragrance-free, hypoallergenic moisturizers nightly | Use scented lotions, soaps, or detergents |
| Take a lukewarm oatmeal bath before bed if skin is inflamed | Ignore persistent itching lasting over two weeks |
Step-by-Step Guide to Reduce Nighttime Itching
If you're struggling with recurrent nighttime itch, follow this structured approach to identify and resolve the issue:
- Assess Your Environment: Inspect bedding for signs of pests, wash all linens in hot water, and vacuum the mattress. Consider switching to fragrance-free laundry detergent.
- Adjust Skincare Routine: Replace harsh soaps with gentle, pH-balanced cleansers. Limit showers to 5–10 minutes with lukewarm water.
- Hydrate Skin Immediately After Bathing: Pat skin dry and apply a thick emollient like ceramide-based cream or petroleum jelly while skin is still damp.
- Optimize Bedroom Climate: Use a humidifier during winter or in dry climates. Keep room temperature below 70°F (21°C) to reduce sweating and irritation.
- Wear Appropriate Sleepwear: Choose soft, natural fibers. Avoid tight-fitting clothes that rub against sensitive areas.
- Rule Out Medical Causes: If home care fails, schedule a visit with your primary care provider or dermatologist. Blood tests may be needed to check liver, kidney, or thyroid function.
- Track Symptoms: Keep a daily log noting when itching occurs, severity, location, and any potential triggers (e.g., food, stress, new product).
Real-Life Example: Sarah’s Story
Sarah, a 42-year-old teacher from Portland, struggled with intense leg itching every night for nearly three months. She initially blamed her new laundry detergent, but switching brands didn’t help. The itch was worst right after getting into bed and often woke her up. Over time, she developed rough, discolored patches on her shins from scratching.
After seeing a dermatologist, Sarah learned she had a combination of xerosis and early-stage eczema exacerbated by low indoor humidity and nightly use of a heavily perfumed body lotion. Her doctor recommended discontinuing fragranced products, installing a bedroom humidifier, and applying a prescription-strength barrier repair cream nightly.
Within two weeks, her symptoms improved dramatically. By week four, the itching had stopped entirely. “I didn’t realize how much my nighttime routine was working against me,” Sarah said. “Simple changes made all the difference.”
Expert-Recommended Treatments and Products
Treatment depends on the underlying cause, but several evidence-based options are effective across multiple triggers:
- Topical Corticosteroids: Low-potency hydrocortisone (1%) can reduce inflammation in mild eczema or allergic reactions. Use sparingly and only for short durations unless directed otherwise.
- Antihistamines: Non-drowsy options like loratadine are useful during the day, while sedating types like diphenhydramine may help break the itch-scratch cycle at night—but should not be used long-term without medical advice.
- Barrier Repair Moisturizers: Look for ingredients like ceramides, glycerin, hyaluronic acid, and colloidal oatmeal. These strengthen the skin’s natural defense and retain moisture.
- Prescription Therapies: For chronic conditions like atopic dermatitis, newer treatments such as topical calcineurin inhibitors (tacrolimus) or biologics (dupilumab) may be prescribed.
“Consistent moisturization is the cornerstone of managing nocturnal pruritus,” says Dr. Alan Wu, board-certified dermatologist. “Even if you don’t see visible dryness, compromised barrier function can still cause itch.”
When to See a Doctor
While many cases of nighttime itching respond to lifestyle adjustments, some signs indicate a need for professional evaluation:
- Itching persists beyond two weeks despite self-care
- Rash spreads or becomes painful, blistered, or infected
- You notice unexplained weight loss, fatigue, or fever alongside itching
- Itch is generalized and not linked to a specific area or product
- There’s a history of liver, kidney, or autoimmune disease
A healthcare provider can perform tests, review medications, and determine whether further investigation is warranted.
Frequently Asked Questions
Can anxiety cause nighttime itching?
Yes. Stress and anxiety can heighten sensory perception and trigger histamine release, worsening itch. Additionally, anxious thoughts at bedtime may increase focus on bodily sensations. Mindfulness techniques, breathing exercises, or cognitive behavioral therapy (CBT) can help break this cycle.
Is it safe to use hydrocortisone cream every night?
No. Long-term use of topical steroids—even over-the-counter strengths—can thin the skin, cause discoloration, or lead to dependency. Use only as directed, typically for no more than one to two weeks without medical supervision.
Why do I only itch in bed and not during the day?
This pattern is common due to reduced distractions, cooler room temperatures triggering dryness, increased skin contact with bedding allergens, and circadian-driven changes in hormone and immune activity—all converging at bedtime.
Final Steps Toward Restful Nights
Nighttime skin itching is more than just an annoyance—it can erode sleep quality, emotional well-being, and overall health. The key to relief lies in understanding the interplay between environment, biology, and skin integrity. Start with simple, sustainable changes: upgrade your moisturizing routine, optimize your sleep environment, and eliminate common allergens. Track your progress and don’t hesitate to seek medical guidance if symptoms persist.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?