Bloating after meals is a surprisingly common complaint—yet it’s not normal when it happens consistently. That tight, swollen feeling in your abdomen isn’t just uncomfortable; it can be disruptive to daily life, confidence, and overall well-being. While occasional bloating may result from overeating or gas buildup, recurrent post-meal bloating points to underlying digestive imbalances or dietary sensitivities. Understanding the root causes and practical solutions can transform how you feel after eating.
This article explores the most likely reasons behind persistent bloating, identifies key triggers based on clinical evidence and patient patterns, and provides actionable steps to reduce discomfort and support long-term gut health.
Common Causes of Post-Meal Bloating
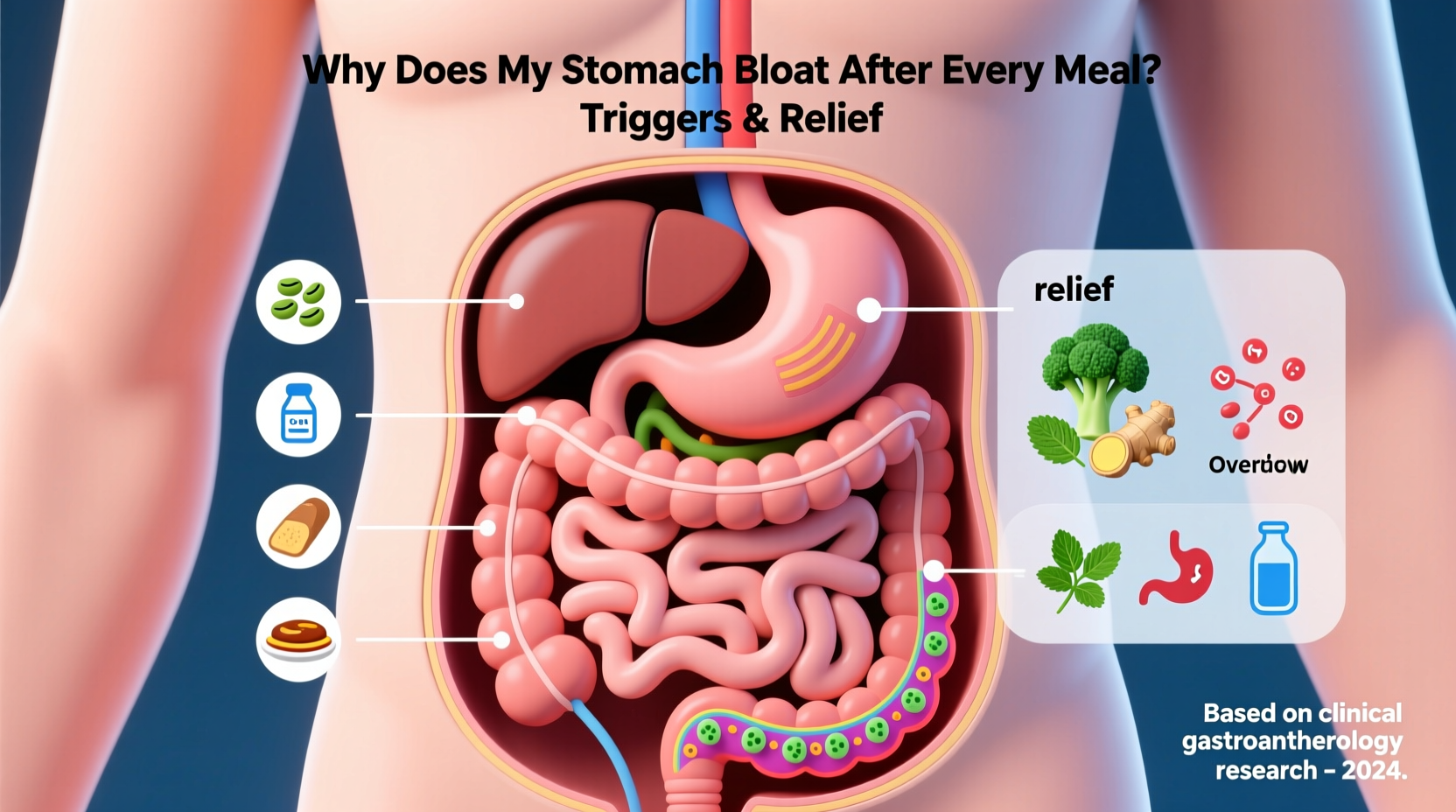
Bloating occurs when the gastrointestinal tract fills with air or gas, leading to distension, pressure, and discomfort. While many assume it's simply due to eating too quickly, the reality is often more complex. The digestive system is highly sensitive to food composition, gut microbiota balance, motility, and immune responses.
- Dietary triggers: Certain foods ferment in the colon, producing gas. High-FODMAP foods like onions, garlic, beans, and dairy are frequent culprits.
- Swallowing air (aerophagia): Eating too fast, chewing gum, drinking carbonated beverages, or talking while eating introduces excess air into the stomach.
- Lactose intolerance: A deficiency in lactase enzyme leads to undigested lactose fermenting in the gut, causing gas and bloating.
- Irritable Bowel Syndrome (IBS): IBS affects up to 15% of people globally and commonly presents with bloating after meals as a primary symptom.
- Small Intestinal Bacterial Overgrowth (SIBO): An abnormal increase in bacteria in the small intestine ferments carbohydrates prematurely, generating significant gas.
- Delayed gastric emptying (gastroparesis): When the stomach empties slowly, food lingers, increasing fermentation and pressure.
- Food intolerances: Beyond lactose, sensitivities to gluten, fructose, eggs, or additives can trigger inflammation and bloating.
Foods That Commonly Trigger Bloating
Not all bloating is caused by poor digestion mechanics—some foods are inherently more likely to cause gas and distension due to their chemical structure or how they’re processed in the gut.
| Food Group | Why It Causes Bloating | Alternatives |
|---|---|---|
| Beans & Lentils | High in raffinose, a complex sugar fermented by gut bacteria | Soak and rinse before cooking; try smaller portions |
| Cabbage, Broccoli, Cauliflower | Contain raffinose and sulfur compounds that produce gas | Steam instead of raw; moderate intake |
| Onions & Garlic | High in fructans (FODMAPs), which ferment easily | Use garlic-infused oil (fructans not fat-soluble) |
| Dairy (milk, soft cheeses) | Lactose intolerance affects ~65% of adults worldwide | Lactose-free milk, hard cheeses, plant-based options |
| Carbonated Drinks | Introduce CO₂ directly into the digestive tract | Still water, herbal teas, infused waters |
| Wheat & Rye | Contain fructans and gluten (problematic for some) | Gluten-free grains like rice, quinoa, oats (certified) |
“Many patients report dramatic improvement once they eliminate high-FODMAP foods—even without a formal diagnosis of IBS.” — Dr. Lena Torres, Gastroenterologist, Cleveland Clinic
Hidden Triggers Beyond Food
While diet plays a central role, other factors contribute significantly to post-meal bloating. These are often overlooked but can make or break your digestive comfort.
Eating Habits and Pace
Eating quickly reduces chewing efficiency and increases swallowed air. Saliva contains enzymes critical for early digestion—rushing through meals compromises this process. Studies show that chewing each bite 20–30 times improves nutrient absorption and reduces bloating.
Stress and Digestive Function
The gut-brain axis means emotional stress directly impacts digestion. Elevated cortisol slows motility, alters gut microbiota, and increases intestinal permeability (“leaky gut”), all contributing to bloating. Chronic stress may even worsen conditions like IBS.
Medications and Supplements
Some medications—including antibiotics, NSAIDs, and certain antidepressants—affect gut flora and motility. Iron supplements and calcium carbonate antacids are notorious for causing gas and constipation-related bloating.
Hormonal Fluctuations
Women often experience increased bloating during menstruation due to progesterone-induced smooth muscle relaxation in the gut, slowing transit time. This can lead to fermentation and gas accumulation even with normal eating patterns.
Step-by-Step Guide to Reducing Bloating
If bloating disrupts your life, a structured approach yields better results than random dietary changes. Follow this timeline to identify, test, and resolve the issue.
- Week 1–2: Track Symptoms and Diet
Use a notebook or app to log meals, portion sizes, timing, and bloating severity (rate 1–10). Include notes on stress levels, bowel movements, and sleep quality. - Week 3: Eliminate Top Suspects
Remove common triggers: dairy, wheat, carbonated drinks, artificial sweeteners (sorbitol, xylitol), and cruciferous vegetables. Replace with low-FODMAP alternatives. - Week 4: Reintroduce One at a Time
Add back one eliminated food every 3 days. For example, reintroduce lactose via a small glass of milk and monitor symptoms. This helps pinpoint specific intolerances. - Week 5: Optimize Eating Patterns
Eat smaller, more frequent meals. Chew thoroughly. Avoid lying down within 2 hours of eating. Consider taking a short walk after meals to stimulate motility. - Week 6+: Assess and Adjust
Evaluate your progress. If bloating persists despite elimination, consult a healthcare provider to rule out SIBO, celiac disease, or other conditions.
“A systematic elimination and reintroduction protocol is far more effective than lifelong restriction. Most people can tolerate small amounts of trigger foods once their gut heals.” — Dr. Rajiv Mehta, Functional Medicine Practitioner
When to See a Doctor
Occasional bloating is normal. But if you experience any of the following, seek medical evaluation:
- Bloating that occurs after nearly every meal
- Severe pain, cramping, or visible abdominal distension
- Unexplained weight loss
- Changes in bowel habits (diarrhea, constipation, or both)
- Blood in stool or persistent nausea
These could indicate conditions such as celiac disease, inflammatory bowel disease (IBD), ovarian cysts, or gastroparesis. Diagnostic tools like hydrogen breath tests (for SIBO or lactose intolerance), blood panels (celiac screening), or endoscopy may be necessary.
Practical Relief Strategies You Can Start Today
Even before identifying exact triggers, several safe, evidence-based methods can reduce bloating and improve comfort.
Hydration and Fiber Balance
Drinking enough water supports digestion and prevents constipation-related bloating. However, increasing fiber too quickly—especially insoluble fiber—can worsen gas. Gradually add soluble fiber sources like oats, psyllium, and peeled apples, and pair them with adequate fluids.
Movement After Meals
A 10–15 minute walk after eating stimulates peristalsis—the wave-like contractions that move food through the digestive tract. This simple habit can prevent stagnation and fermentation.
Probiotics and Gut Support
Strain-specific probiotics (like *Bifidobacterium infantis* 35624) have demonstrated efficacy in reducing bloating. Fermented foods such as kefir, sauerkraut (in moderation), and kimchi may also help—but introduce slowly to avoid initial gas increases.
Abdominal Massage and Positioning
Gentle clockwise massage along the path of the colon can encourage gas movement. Lying on your left side after meals may also aid digestion by leveraging gravity for stomach emptying.
Mini Case Study: Sarah’s Journey to Relief
Sarah, a 34-year-old teacher, came to a functional nutritionist complaining of daily bloating, fatigue, and irregular bowel movements. She had tried cutting out gluten and dairy with no lasting improvement. Her food diary revealed she consumed large salads for lunch, drank kombucha daily, and ate dinner late after long workdays.
After analysis, three key issues emerged: excessive raw vegetables (high in insoluble fiber), kombucha (carbonated and high in FODMAPs), and chronic stress affecting digestion. She was advised to cook her vegetables, switch to still herbal tea, eat dinner earlier, and practice diaphragmatic breathing before meals.
Within three weeks, Sarah reported a 70% reduction in bloating. A subsequent hydrogen breath test confirmed mild SIBO, which was treated with a short course of antibiotics and dietary adjustments. Six months later, she maintains a balanced diet with occasional reintroductions and reports feeling “lighter and more energetic than in years.”
Checklist: Reduce Bloating in 7 Actions
- ✅ Eat slowly and chew food thoroughly
- ✅ Limit carbonated drinks and artificial sweeteners
- ✅ Identify and eliminate personal food triggers using an elimination diet
- ✅ Stay hydrated with water and herbal teas
- ✅ Take a short walk after meals
- ✅ Manage stress with mindfulness, breathing, or yoga
- ✅ Consult a professional if bloating persists beyond 4–6 weeks of self-management
FAQ
Can drinking water help with bloating?
Yes. Dehydration causes the body to retain sodium and fluid, worsening abdominal swelling. Drinking enough water actually reduces water retention and supports healthy digestion. Aim for pale yellow urine as a hydration guide.
Is bloating a sign of weight gain?
Not necessarily. Bloating causes temporary distension from gas or fluid, not fat accumulation. However, chronic bloating linked to poor digestion may indirectly affect metabolism and appetite regulation over time.
Are probiotics good for bloating?
They can be—but results vary. Some people initially experience more gas when starting probiotics. Strains like *Lactobacillus acidophilus* and *Bifidobacterium* species show promise, especially in those with IBS. Choose clinically studied formulations and give them 4–6 weeks to assess effectiveness.
Conclusion
Bloating after every meal is not something you must accept as inevitable. With careful observation, targeted dietary changes, and lifestyle adjustments, most people can achieve meaningful relief. The key is understanding your unique triggers rather than adopting generic fixes. Whether it’s a hidden food intolerance, eating too quickly, or an imbalance in gut bacteria, solutions exist—and they start with awareness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?