Stomach gurgling—technically known as borborygmi—is a common bodily sound most people experience daily. These rumbling or growling noises occur as fluids and gases move through the intestines during digestion. While often harmless and even normal, persistent or unusually loud gurgling can sometimes point to underlying digestive issues. Understanding the mechanisms behind these sounds, what triggers them, and when they may indicate a more serious condition is essential for maintaining gut health.
The Science Behind Stomach Gurgling
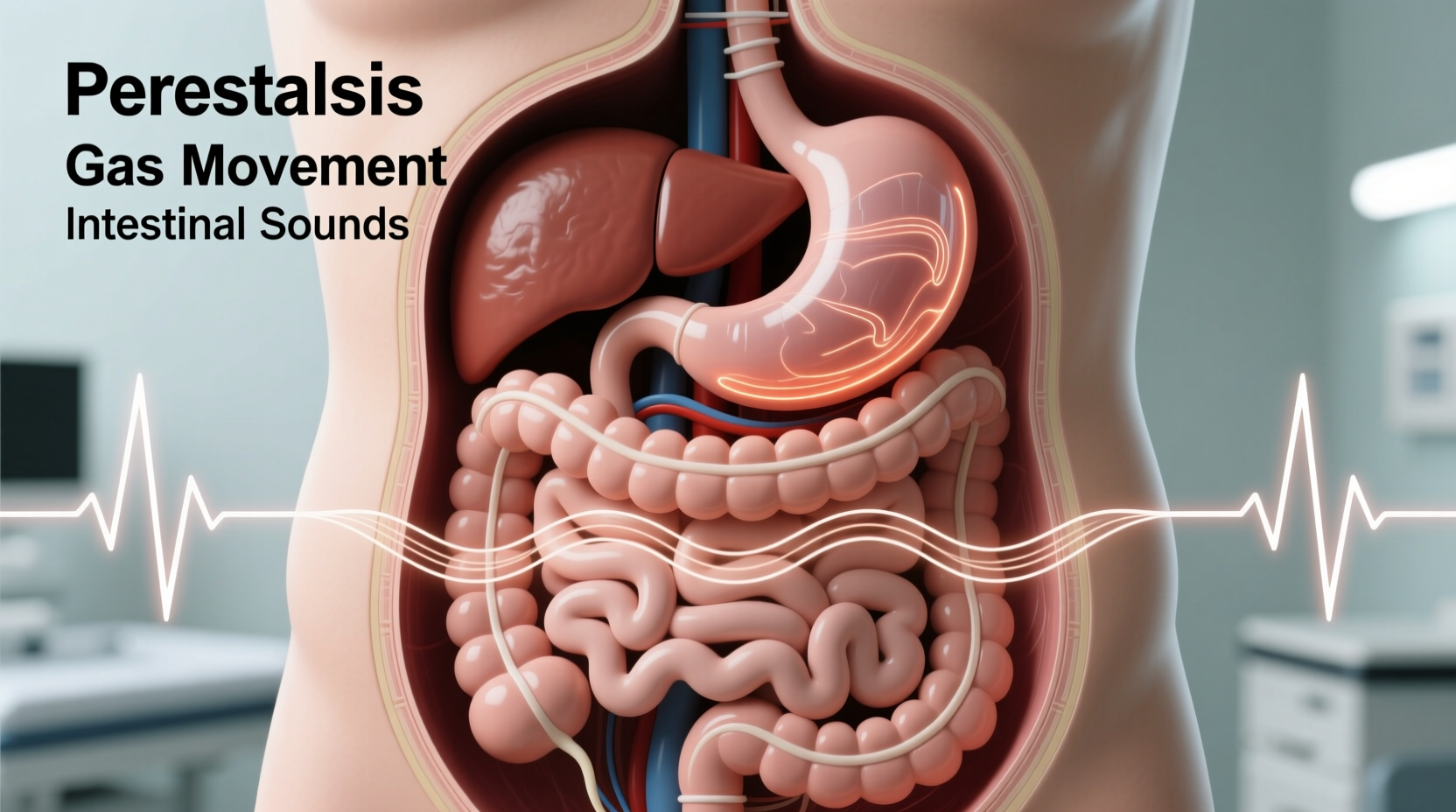
Borborygmi are produced by peristalsis—the rhythmic muscular contractions that push food, liquid, and gas through the gastrointestinal (GI) tract. As the smooth muscles in the stomach and small intestine contract, they mix and propel contents forward, creating vibrations and audible sounds. These noises are typically more noticeable when the stomach is empty, such as between meals or overnight, because there’s less food to muffle the movement.
The human digestive system produces roughly two to three liters of fluid daily, including saliva, gastric juices, bile, and intestinal secretions. Combined with swallowed air and gases produced by bacterial fermentation in the colon, this creates a dynamic internal environment where movement naturally generates sound.
“The gut is never truly silent. Some level of gurgling is expected—it’s a sign the digestive system is active.” — Dr. Lena Patel, Gastroenterologist, Cleveland Clinic
Interestingly, not all stomach noises originate in the stomach itself. Many so-called “stomach rumbles” actually come from the small intestine, particularly the jejunum, which is highly active in moving digested material along the tract.
Common Causes of Random Stomach Gurgling
In most cases, stomach gurgling is benign and tied to routine digestive processes. The following are frequent, non-concerning explanations:
- Hunger signals: When the stomach has been empty for several hours, the brain triggers the migrating motor complex (MMC), a cleaning wave that sweeps residual particles toward the colon. This process is often accompanied by loud gurgling.
- Digestion after eating: Certain foods—especially those high in fiber, sugar, or fat—can increase gas production and intestinal activity, leading to more pronounced noises.
- Swallowed air: Talking while eating, chewing gum, drinking carbonated beverages, or using straws introduces excess air into the digestive tract, contributing to gurgling.
- Lactose intolerance: Inability to digest lactose leads to fermentation by gut bacteria, producing gas and increased bowel sounds.
- High-FODMAP foods: Foods like onions, beans, apples, and wheat contain fermentable carbohydrates that can cause bloating and noisy digestion in sensitive individuals.
When Gurgling Signals a Digestive Disorder
While occasional gurgling is normal, certain patterns or accompanying symptoms may suggest an underlying medical condition. Persistent, disruptive, or painful intestinal sounds warrant attention, especially when combined with other red flags.
Conditions Associated with Abnormal Bowel Sounds
Excessively loud, high-pitched, or rapid gurgling—particularly if localized to one area—may be linked to:
- Irritable Bowel Syndrome (IBS): A functional disorder affecting up to 15% of the global population, IBS often presents with abdominal pain, bloating, and altered bowel habits. Increased intestinal sensitivity and motility can amplify normal digestive sounds.
- Gastroenteritis: Viral or bacterial infections inflame the GI tract, accelerating motility and causing hyperactive bowel sounds, diarrhea, nausea, and cramping.
- Small Intestinal Bacterial Overgrowth (SIBO): An abnormal increase in bacteria in the small intestine leads to excessive gas, bloating, and prominent gurgling, often shortly after eating.
- Celiac Disease: An autoimmune reaction to gluten damages the small intestine lining, impairing digestion and increasing gas and noise.
- Intestinal Obstruction: Partial or complete blockages in the intestines cause high-pitched, tinkling sounds followed by silence in advanced cases. This is a medical emergency.
Warning Signs That Require Medical Evaluation
Not all gurgling is concerning, but the following symptoms should prompt consultation with a healthcare provider:
- Severe or worsening abdominal pain
- Persistent nausea or vomiting
- Inability to pass gas or have a bowel movement
- Fever accompanying digestive symptoms
- Unintentional weight loss
- Blood in stool
- Sudden onset of intense gurgling after surgery or trauma
“If bowel sounds become erratic—either too loud or completely absent—and are paired with distension or pain, it could indicate a mechanical obstruction. Immediate imaging is critical.” — Dr. Marcus Tran, Emergency Medicine Specialist
Do’s and Don’ts: Managing Stomach Gurgling
For most people, simple lifestyle adjustments can reduce bothersome gurgling. The table below outlines key strategies to adopt—or avoid.
| Do’s | Don’ts |
|---|---|
| Eat smaller, more frequent meals to prevent extreme hunger | Overeat or consume large meals rapidly |
| Chew food thoroughly and eat slowly to reduce swallowed air | Drink carbonated beverages regularly |
| Stay hydrated with water throughout the day | Consume excessive caffeine or alcohol, which can irritate the gut |
| Identify and limit trigger foods (e.g., dairy, beans, artificial sweeteners) | Ignore persistent symptoms out of embarrassment |
| Practice stress management; anxiety can heighten gut sensitivity | Self-diagnose serious conditions without medical input |
Step-by-Step Guide to Assessing Your Symptoms
If stomach gurgling concerns you, follow this practical timeline to evaluate whether professional care is needed:
- Day 1–3: Track your symptoms
Record meal times, food types, bowel movements, and when gurgling occurs. Note any associated discomfort, bloating, or changes in stool. - Day 4–7: Adjust diet and habits
Eliminate obvious triggers like carbonation, gum, and high-FODMAP foods. Eat slowly and stay hydrated. See if symptoms improve. - Week 2: Evaluate progress
If gurgling persists despite changes, consider a temporary elimination diet (e.g., low-FODMAP) under guidance. Monitor for patterns. - Week 3–4: Seek medical advice if unresolved
Consult a primary care physician or gastroenterologist if symptoms continue, worsen, or include warning signs like pain or weight loss. - Medical evaluation phase
Your doctor may recommend blood tests, breath tests (for SIBO or lactose intolerance), stool analysis, or imaging such as an abdominal ultrasound or CT scan.
Real-Life Example: When Gurgling Was a Clue to a Bigger Problem
Sarah, a 34-year-old teacher, began noticing her stomach made unusually loud gurgling sounds about 20 minutes after every meal. At first, she dismissed it as indigestion. But over six weeks, the noises became more frequent, accompanied by bloating, diarrhea, and fatigue. She also lost seven pounds unintentionally.
After tracking her meals and trying over-the-counter remedies without success, Sarah visited a gastroenterologist. A hydrogen breath test revealed Small Intestinal Bacterial Overgrowth (SIBO). Further investigation showed she had undiagnosed celiac disease, which had damaged her intestinal lining and allowed bacteria to proliferate abnormally.
With a gluten-free diet and a course of antibiotics, Sarah’s symptoms resolved within two months. Her case illustrates how seemingly minor digestive noises can be early indicators of systemic issues when persistent and paired with other symptoms.
Frequently Asked Questions
Is it normal for my stomach to gurgle when I’m not hungry?
Yes. Even outside of hunger, the digestive tract continues its housekeeping functions. The migrating motor complex activates every 90–120 minutes between meals to clear residual matter, often producing audible gurgling. This is normal unless accompanied by pain or irregular bowel habits.
Can stress cause my stomach to gurgle more?
Absolutely. The gut and brain are closely linked via the gut-brain axis. Stress and anxiety can accelerate intestinal motility, leading to louder or more frequent bowel sounds. Techniques like deep breathing, meditation, or mindfulness may help regulate gut activity.
Why do I hear gurgling at night when I’m trying to sleep?
Nocturnal gurgling often results from the MMC activating during fasting periods. With fewer external noises, internal sounds become more noticeable. If disruptive, avoid late-night snacks and consider elevating your head slightly to reduce abdominal pressure.
Conclusion: Listen to Your Gut—Literally
Stomach gurgling is usually a mundane part of digestion, reflecting the quiet yet constant work of your gastrointestinal system. But like any bodily signal, it deserves attention when patterns shift or intensity increases. By understanding the science behind these sounds and recognizing when they deviate from the norm, you empower yourself to take proactive steps toward better digestive health.
Don’t ignore persistent symptoms out of dismissal or discomfort. Many digestive disorders are manageable when caught early. Whether it’s adjusting your diet, reducing stress, or seeking medical insight, small actions today can prevent larger complications tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?