Many people experience discomfort when wearing wool—itchy skin, a scratchy neck, or even an irritated throat. If you’ve noticed your throat itching every time you put on a wool sweater or scarf, you’re not alone. But is this a sign of a true wool allergy, or something else entirely? Understanding the root cause can help you make better clothing choices and avoid unnecessary discomfort.
Wool is a natural fiber derived from sheep and other animals, prized for its warmth, breathability, and durability. However, its coarse texture and chemical processing can trigger physical and immune responses in some individuals. While a true allergic reaction to wool protein is rare, the symptoms it produces—especially throat irritation—are often mistaken for allergies.
The Science Behind Wool Sensitivity
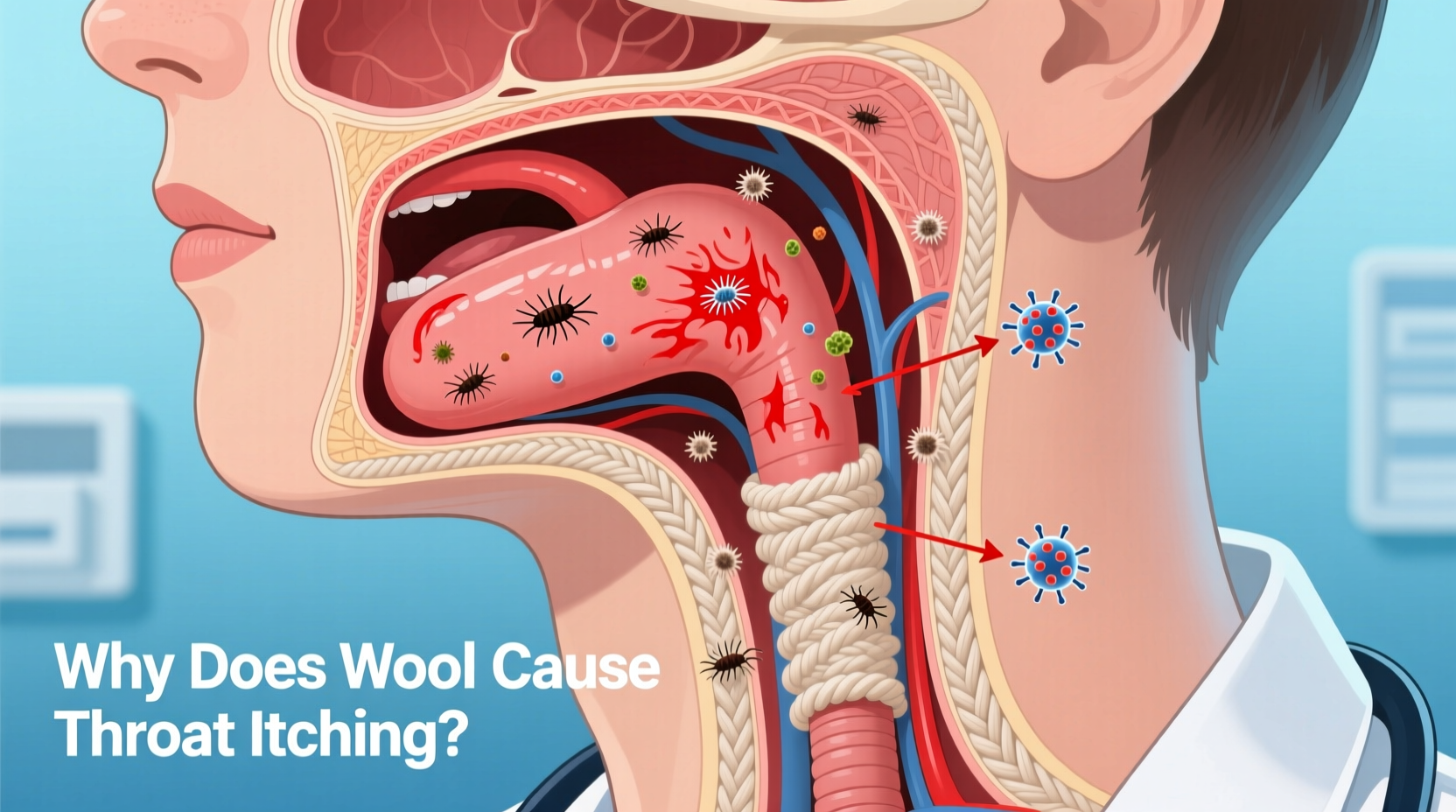
When people report throat itching from wool, they're usually reacting to one of two factors: mechanical irritation or chemical exposure. True immunoglobulin E (IgE)-mediated allergies to wool fibers themselves are extremely uncommon. Instead, most reactions stem from either the physical properties of wool or substances used during manufacturing.
Raw wool contains lanolin, a waxy substance secreted by sheep that helps waterproof their fleece. Lanolin is sometimes allergenic and can cause contact dermatitis in sensitive individuals. However, most commercial wool garments undergo scouring processes that remove much of the lanolin. Still, trace amounts may remain, especially in less processed or organic wool products.
The more common culprit behind throat itching is the **mechanical stimulation** caused by coarse wool fibers. When wool rubs against the delicate skin of the neck and jawline, it can trigger nerve endings that send signals to the brain interpreted as itching. These signals can extend beyond the skin and create a sensation in the throat due to shared neural pathways.
“While patients often describe wool as ‘allergenic,’ we rarely find evidence of true IgE-mediated allergy. The discomfort is usually due to sensory irritation rather than immune activation.” — Dr. Rebecca Langston, Allergist & Immunologist, Cleveland Clinic
Differentiating Between Irritation and Allergy
It’s crucial to distinguish between physical irritation and a genuine allergic response. Mislabeling irritation as an allergy can lead to unnecessary avoidance of materials or misdiagnosis of underlying conditions.
| Symptom | Mechanical Irritation | True Allergy |
|---|---|---|
| Skin itching at contact site | Common (immediate) | Possible (delayed) |
| Throat itching or tickling | Frequent (reflexive) | Rare, but possible with airborne particles |
| Hives or rash | Uncommon unless scratched | Common (localized or systemic) |
| Nasal congestion or sneezing | No | Yes (if airborne allergens present) |
| Breathing difficulty | No | Possible (in severe cases) |
| Reaction to synthetic wool blends | Yes (if coarse) | Unlikely (unless other allergens present) |
As shown in the table, a true wool allergy would typically involve immune system activation—such as hives, swelling, or respiratory symptoms—and may require medical testing to confirm. In contrast, mechanical irritation tends to be localized, temporary, and directly linked to fabric texture.
Could It Be Something Else?
Before concluding that wool is the sole cause, consider other contributing factors. Environmental allergens trapped in wool fibers—like dust mites, pet dander, or mold spores—can become airborne when the garment is worn, potentially irritating the throat and nasal passages.
In addition, many wool garments are treated with chemicals such as mothproofing agents, dyes, formaldehyde resins, or flame retardants. These substances can off-gas or transfer to the skin and mucous membranes, causing irritation that mimics allergy symptoms. This is known as **contact urticaria** or chemical sensitivity.
Another overlooked factor is dry air. Wool naturally absorbs moisture, which can dry out the skin and mucous membranes in low-humidity environments. A dry throat may feel itchy or scratchy, especially when breathing through the mouth near a wool collar.
Mini Case Study: Sarah’s Winter Itch
Sarah, a 34-year-old teacher from Minnesota, began experiencing throat irritation every winter when she wore her favorite wool turtleneck. She assumed she was allergic and avoided all wool products, switching to synthetic thermals. However, her symptoms persisted.
After consulting an allergist, she discovered she wasn’t allergic to wool at all. Instead, her symptoms were exacerbated by indoor heating, which dried out her throat, and by residual detergent in her clothes. Her doctor recommended using fragrance-free detergent, adding a humidifier to her bedroom, and wearing a soft cotton liner under wool. Within two weeks, her throat itching disappeared—even when she resumed wearing wool.
How to Test for a True Wool Allergy
If you suspect a genuine allergy, proper diagnosis is essential. Self-diagnosis can lead to unnecessary lifestyle changes or missed identification of other conditions like asthma, acid reflux, or chronic sinusitis.
A board-certified allergist can perform the following assessments:
- Skin Prick Test: Small amounts of purified wool or lanolin extract are applied to the skin using a tiny prick. If a raised bump appears within 15–20 minutes, it may indicate sensitization.
- Patch Testing: Used to detect delayed-type hypersensitivity, particularly to lanolin or textile chemicals.
- Elimination and Challenge: You stop wearing wool for 2–3 weeks, then reintroduce it under observation to monitor symptoms.
- Blood Test (Specific IgE): Measures antibodies to wool or lanolin proteins in the bloodstream—less commonly used but available.
Keep in mind: a positive test doesn’t always mean clinical allergy. Some people show sensitization without experiencing real-world symptoms. Diagnosis must correlate with actual exposure history and symptom patterns.
Practical Solutions and Alternatives
Whether your reaction is allergic or irritative, relief is possible. The goal isn’t necessarily to eliminate wool entirely—but to manage exposure and choose smarter alternatives when needed.
Step-by-Step Guide to Reducing Throat Itching from Wool
- Wash New Wool Garments Before Wearing: Use a mild, hypoallergenic detergent to remove residual chemicals and loose fibers.
- Wear a Barrier Layer: Choose a breathable undershirt made of cotton, silk, or microfiber to minimize direct contact.
- Opt for Fine-Gauge Merino Wool: Merino fibers are much finer (typically 17–20 microns) than traditional wool (25+ microns), making them softer and less likely to irritate.
- Check Fabric Blends: Look for wool blended with silk or nylon, which improves softness and reduces coarseness.
- Use a Humidifier: Maintain indoor humidity between 40–60% to prevent dry throat irritation, especially in winter.
- Switch Detergents: Avoid fabric softeners and scented detergents, which can leave residues that irritate skin and airways.
- Store Wool Properly: Keep in sealed containers with natural cedar blocks instead of chemical mothballs, which can emit volatile compounds.
Best Wool Alternatives for Sensitive Individuals
- Merino Wool: Naturally soft, moisture-wicking, and temperature-regulating with minimal itch.
- Cashmere: Luxuriously soft but requires careful handling; best layered over a base.
- Bamboo Fiber: Hypoallergenic, silky, and sustainable—excellent for base layers.
- TENCEL™ (Lyocell): Made from wood pulp, smooth to the touch and resistant to odor.
- Organic Cotton: Breathable and gentle, ideal for layering under outerwear.
FAQ: Common Questions About Wool and Throat Itching
Can wool fibers actually get into my throat?
While wool fibers don’t typically “enter” the throat like inhaled particles, microscopic fibers can become airborne when garments are rubbed or shaken. In sensitive individuals, these fibers may settle on mucous membranes and trigger a reflexive itch or cough. However, this is more common with damaged or frayed wool and in poorly ventilated spaces.
Is lanolin allergy common?
Lanolin allergy affects approximately 1.5–2% of the general population, according to studies published in *Dermatitis*. It’s more prevalent among people with atopic dermatitis or frequent exposure to lanolin-containing products (e.g., lip balms, lotions). If you react to skincare products with lanolin, you may also react to unprocessed wool.
Why do some wool sweaters itch more than others?
The degree of itchiness depends on fiber diameter, weave tightness, and finishing treatments. Coarser wools (like traditional Shetland or Icelandic wool) have larger fiber diameters (>25 microns) that physically stimulate nerve endings. Finer weaves and mercerized wool (chemically smoothed) are less irritating. Garment construction also matters—seams and collars with exposed edges tend to be scratchier.
Checklist: Managing Wool-Related Throat Itching
- ✔ Wash new wool items before first use
- ✔ Wear a soft inner layer (cotton or silk)
- ✔ Choose merino or fine-gauge wool
- ✔ Avoid wool blends with harsh synthetics
- ✔ Use fragrance-free, dye-free laundry products
- ✔ Maintain indoor humidity above 40%
- ✔ Consult an allergist if symptoms persist
- ✔ Patch-test new wool garments on forearm first
Conclusion: Listen to Your Body, But Don’t Jump to Conclusions
An itchy throat when wearing wool is a common complaint, but it’s rarely due to a true allergy. More often, it results from physical irritation, chemical residues, or environmental factors that amplify sensitivity. By understanding the mechanisms behind the discomfort, you can take targeted steps to reduce or eliminate symptoms—without giving up the warmth and sustainability of wool altogether.
Start with simple adjustments: add a barrier layer, switch detergents, or try merino wool. If symptoms continue despite precautions, seek professional evaluation to rule out allergies or other underlying conditions. With informed choices, you can enjoy the benefits of wool while keeping your throat—and peace of mind—soothed.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?