Suddenly standing from a seated or lying position and experiencing blurry vision is more common than many realize. While occasional episodes may not be cause for alarm, frequent or severe blurring can signal underlying physiological changes or medical conditions that warrant attention. This phenomenon—often accompanied by dizziness, lightheadedness, or even momentary tunnel vision—is primarily linked to how blood pressure and circulation respond to postural shifts. Understanding the mechanisms behind this response, the contributing factors, and when to seek help is essential for maintaining long-term cardiovascular and neurological health.
The Science Behind Postural Vision Changes
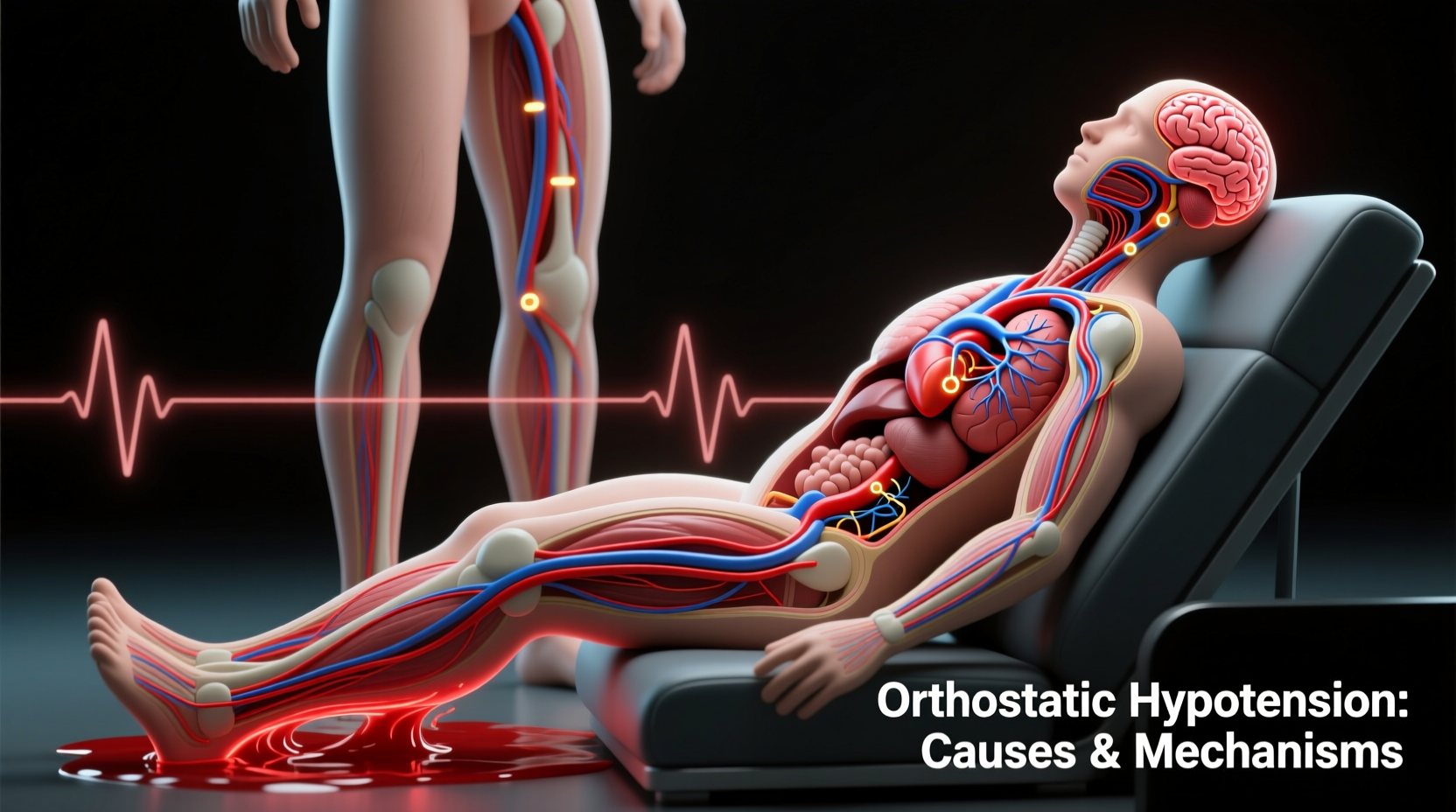
When you stand up quickly, gravity pulls blood downward into your legs and abdomen. This temporary pooling reduces the volume of blood returning to your heart, which in turn lowers cardiac output and blood pressure. The brain, being highly sensitive to oxygen levels, receives less blood flow momentarily—a condition known as cerebral hypoperfusion. Since vision relies heavily on consistent blood supply to the retina and visual cortex, even a brief drop can disrupt clarity, causing blurriness, dimming, or “graying out” of sight.
This reaction is part of a normal physiological process called orthostatic regulation. In healthy individuals, baroreceptors—specialized sensors in the arteries of the neck and chest—detect the drop in blood pressure and trigger an immediate compensatory response: the heart beats faster and blood vessels constrict to restore adequate circulation within seconds. However, if this system is delayed, impaired, or overwhelmed, symptoms like blurred vision persist longer than normal.
“Even a two-second delay in autonomic correction can result in noticeable visual disturbances upon standing.” — Dr. Lena Torres, Neurocardiologist at Boston General Hospital
Common Underlying Factors
While transient blurring upon standing is often benign, several underlying conditions can exacerbate or prolong the effect. Identifying these contributors helps determine whether the symptom is isolated or part of a broader health issue.
1. Orthostatic Hypotension
Also known as postural hypotension, this condition occurs when systolic blood pressure drops by at least 20 mm Hg or diastolic by 10 mm Hg within three minutes of standing. It’s one of the most direct causes of vision blurring during positional change. Common in older adults, it can also affect younger people with autonomic dysfunction.
2. Dehydration
Inadequate fluid intake reduces blood volume, making it harder for the body to maintain pressure when upright. Even mild dehydration—such as after a night’s sleep or prolonged exercise without rehydration—can trigger temporary vision issues upon rising.
3. Medication Side Effects
Several classes of medications influence blood pressure regulation:
- Blood pressure drugs (e.g., beta-blockers, calcium channel blockers)
- Diuretics (“water pills”)
- Antidepressants (especially tricyclics)
- Parkinson’s disease medications
- Some erectile dysfunction treatments
These can impair the body’s ability to adjust rapidly to posture changes.
4. Autonomic Nervous System Disorders
The autonomic nervous system controls involuntary functions like heart rate and vascular tone. Conditions such as Parkinson’s disease, multiple system atrophy, diabetic neuropathy, and pure autonomic failure interfere with its signaling, leading to poor orthostatic compensation.
5. Anemia
Low red blood cell count reduces oxygen-carrying capacity. When combined with reduced cerebral perfusion upon standing, this can amplify visual symptoms due to insufficient oxygen delivery to the eyes and brain.
Who Is Most at Risk?
Certain populations are more prone to experiencing vision disturbances upon standing due to age-related changes, chronic illnesses, or lifestyle factors.
| Group | Risk Level | Primary Contributing Factors |
|---|---|---|
| Adults over 65 | High | Reduced vascular elasticity, medication use, slower autonomic response |
| People with diabetes | Moderate to High | Autonomic neuropathy, dehydration from frequent urination |
| Individuals on antihypertensives | Moderate | Medication-induced low BP, especially if dosed incorrectly |
| Young adults with POTS | Moderate | Dysautonomia, rapid heart rate increase, poor venous return |
| Athletes or those fasting | Low to Moderate | Lower baseline BP, electrolyte imbalance |
When Blurry Vision Signals Something Serious
Occasional blurring lasting only a few seconds is typically not dangerous. However, certain red flags suggest the need for medical evaluation:
- Episodes lasting longer than 10–15 seconds
- Frequent falls or near-falls after standing
- Loss of consciousness (syncope)
- Double vision, slurred speech, or limb weakness accompanying blurriness
- Nighttime urination and persistent fatigue (possible signs of autonomic failure)
If blurry vision upon standing is paired with palpitations, excessive sweating, or tremors, it may indicate dysautonomia or endocrine disorders such as adrenal insufficiency. Similarly, sudden onset in younger individuals without clear triggers should prompt investigation for conditions like Postural Orthostatic Tachycardia Syndrome (POTS), where heart rate spikes abnormally upon standing.
Mini Case Study: Sarah’s Morning Episodes
Sarah, a 34-year-old graphic designer, began noticing that every morning when she got out of bed, her vision would blur and the room would spin slightly. At first, she dismissed it as fatigue. But when it started happening after lunch breaks at work, she consulted her physician. Blood tests revealed mild anemia and low sodium levels. Further evaluation showed she had been unknowingly restricting salt and fluids while trying to reduce bloating. Her doctor advised gradual increases in hydration, moderate salt intake, and a slow rise routine. Within two weeks, her symptoms resolved completely.
This case highlights how seemingly minor lifestyle choices—when compounded—can disrupt circulatory stability and manifest as visual disturbances.
Step-by-Step Guide to Managing and Preventing Symptoms
For those experiencing recurrent blurriness upon standing, proactive measures can significantly reduce frequency and severity. Follow this sequence to improve orthostatic tolerance:
- Hydrate consistently throughout the day. Aim for 2–2.5 liters of water daily unless contraindicated by kidney or heart conditions.
- Review medications with your doctor. Ask whether any prescriptions could contribute to low blood pressure or autonomic suppression.
- Move slowly when changing positions. After lying down, sit up first and wait 30 seconds before standing.
- Perform counter-pressure maneuvers if symptoms begin. Cross your legs and tense leg muscles, or squat slightly to push blood back toward the heart.
- Increase salt intake moderately—if approved by your physician. Sodium helps retain fluid volume and supports blood pressure.
- Engage in regular cardiovascular exercise. Activities like walking, swimming, or cycling enhance circulatory efficiency and autonomic control.
- Monitor symptoms with a home blood pressure cuff. Check readings while lying down and again after standing to detect significant drops.
Expert-Recommended Checklist for Daily Prevention
Checklist: Reduce Risk of Vision Blurring When Standing
- ✅ Drink water first thing in the morning before getting out of bed
- ✅ Avoid alcohol, especially in excess—it dilates blood vessels and worsens drops in pressure
- ✅ Wear compression stockings if recommended by a doctor (helps prevent blood pooling)
- ✅ Eat smaller, more frequent meals (large meals divert blood to the gut, lowering central pressure)
- ✅ Avoid hot environments like saunas or long hot showers—they promote vasodilation
- ✅ Keep a symptom journal noting frequency, duration, and triggers
- ✅ Schedule annual physicals with blood work and BP assessment
Frequently Asked Questions
Is it normal for young people to have blurry vision when standing?
Yes, though less common, younger individuals—especially women—can experience this due to conditions like POTS, dehydration, or anxiety-related hyperventilation. If symptoms are frequent or disruptive, evaluation by a cardiologist or neurologist is recommended.
Can low blood sugar cause vision blurring when standing?
Indirectly, yes. Hypoglycemia can cause generalized dizziness and visual disturbances. However, the combination of low blood sugar and orthostatic stress can amplify symptoms. Eating balanced meals with complex carbohydrates helps stabilize both glucose and circulation.
Should I worry if my vision blurs only once in a while?
Infrequent, brief episodes—especially after skipping meals or sleeping poorly—are usually not concerning. However, increasing frequency, longer duration, or associated symptoms like fainting should prompt a visit to your healthcare provider.
Conclusion: Listen to Your Body’s Signals
Blurry vision when standing quickly is not something to routinely dismiss. While often temporary and harmless, it serves as a physiological warning sign—a message from your cardiovascular system that balance has been disrupted. By understanding the underlying mechanisms and addressing modifiable risk factors like hydration, medication effects, and movement habits, you can regain stability and confidence in your daily routines.
Don’t wait for symptoms to worsen. Small adjustments today can prevent falls, injuries, or the progression of undiagnosed conditions tomorrow. Pay attention to patterns, take preventive steps, and consult a healthcare professional if concerns persist.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?