Suddenly standing from a seated or lying position and experiencing blurred vision is more common than many realize. While it’s often fleeting and harmless, it can be alarming—and in some cases, it signals an underlying health issue. This phenomenon typically results from temporary changes in blood flow and pressure regulation. Understanding the physiological mechanisms behind it, recognizing risk factors, and knowing when to take action can help prevent complications and improve daily well-being.
What Happens When You Stand Up Suddenly?
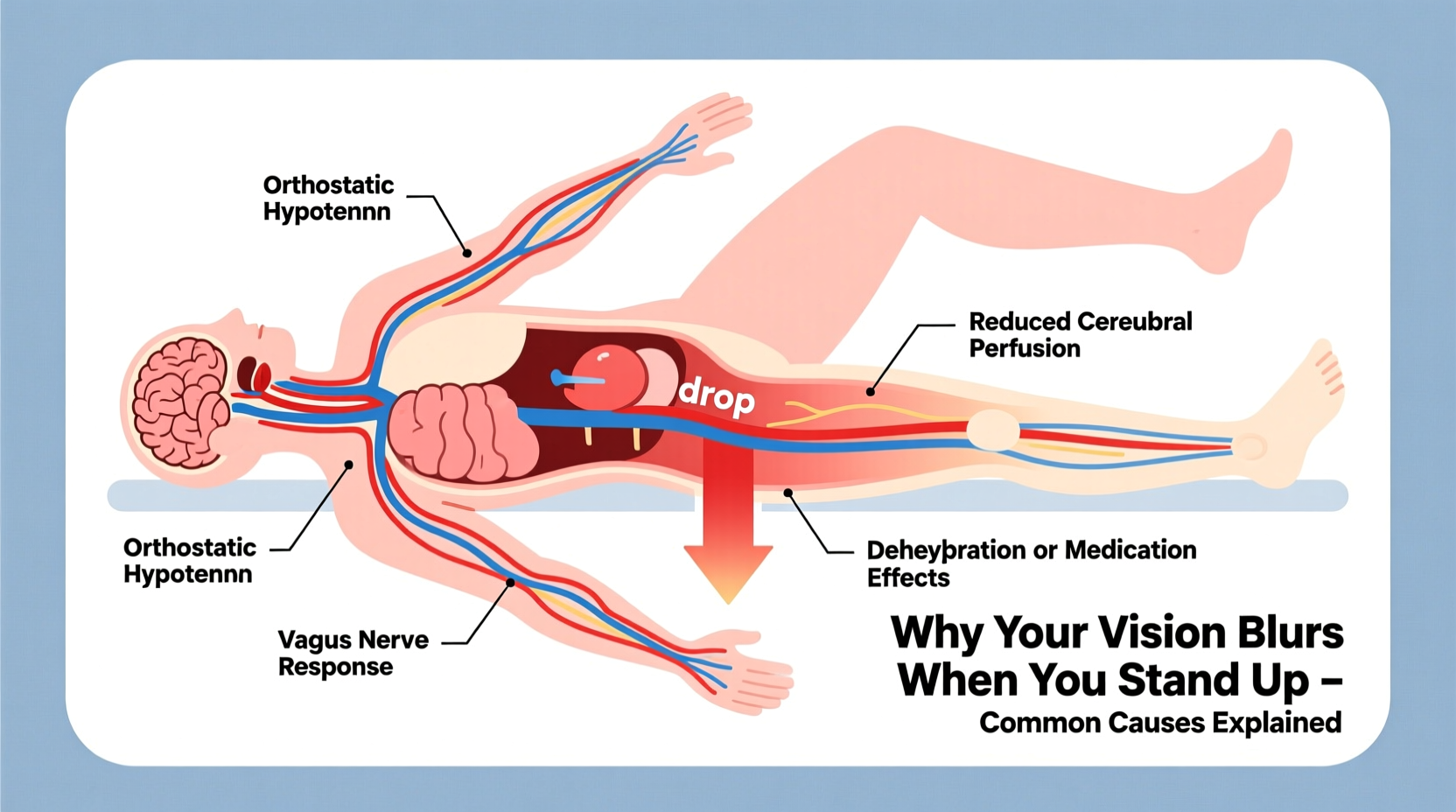
When you rise quickly from a reclining or sitting posture, gravity pulls blood downward into your legs and abdomen. This reduces the amount of blood returning to your heart and, subsequently, the volume of blood pumped to your brain. The brain is highly sensitive to even brief drops in oxygen supply, which can lead to visual disturbances such as blurring, darkening, or “seeing stars.”
The body normally compensates for this shift through the autonomic nervous system, which triggers blood vessels to constrict and the heart rate to increase, restoring adequate blood flow within seconds. However, if this regulatory system lags or fails, symptoms like blurred vision, dizziness, or lightheadedness occur. This condition is medically known as **orthostatic intolerance**, with orthostatic hypotension being one of its most common forms.
Common Causes of Blurred Vision Upon Standing
Several factors can disrupt the body's ability to regulate blood pressure during positional changes. Below are the most frequent contributors:
1. Orthostatic Hypotension (Postural Hypotension)
This occurs when systolic blood pressure drops by at least 20 mm Hg or diastolic pressure by 10 mm Hg within three minutes of standing. It directly affects cerebral perfusion, leading to transient vision changes. Common triggers include dehydration, prolonged bed rest, aging, and certain medications.
2. Dehydration
Inadequate fluid intake reduces blood volume, making it harder for the body to maintain stable pressure upon standing. Even mild dehydration—such as after a night’s sleep or during hot weather—can trigger symptoms.
3. Inner Ear and Vestibular Dysfunction
The inner ear plays a critical role in balance and spatial orientation. Conditions like benign paroxysmal positional vertigo (BPPV) or vestibular neuritis may not directly affect blood pressure but can cause disorientation and visual blurring when combined with rapid movement.
4. Medications
Many prescription drugs impact blood pressure regulation. These include:
- Diuretics (water pills)
- Alpha-blockers for prostate issues
- Antidepressants (especially tricyclics)
- Antihypertensives (blood pressure medications)
- Parkinson’s disease treatments
If you’ve recently started or changed medication and notice new symptoms, consult your healthcare provider.
5. Autonomic Nervous System Disorders
Diseases that impair the autonomic nervous system—such as Parkinson’s disease, diabetes-related neuropathy, or multiple system atrophy—can interfere with the body’s ability to adjust blood pressure automatically.
“Transient visual blurring upon standing is often benign, but recurrent episodes warrant evaluation—especially in older adults or those with chronic conditions.” — Dr. Lena Torres, Neurologist and Autonomic Specialist
Who Is Most at Risk?
While anyone can experience momentary vision changes when standing too fast, certain groups face higher risks due to age, health status, or lifestyle factors.
| Group | Risk Level | Primary Contributing Factors |
|---|---|---|
| Adults over 65 | High | Aging-related vascular stiffness, polypharmacy, reduced baroreflex sensitivity |
| People with diabetes | Moderate to High | Autonomic neuropathy, vascular damage |
| Individuals on blood pressure meds | Moderate | Excessive lowering of BP, especially with dose changes |
| Young adults with low BMI | Mild to Moderate | Vasovagal sensitivity, lower circulating blood volume |
| Those with chronic fatigue syndrome or POTS | High | Dysautonomia, exaggerated heart rate response |
Mini Case Study: Sarah’s Morning Episodes
Sarah, a 42-year-old office worker, began noticing that she frequently saw “a gray haze” every morning when getting out of bed. At first, she dismissed it as fatigue, but when the episodes persisted for weeks and were occasionally accompanied by near-fainting sensations, she consulted her doctor.
Testing revealed mildly low blood pressure upon standing (from 120/80 to 98/66 mm Hg), along with slightly elevated heart rate. Her medical history included controlled hypertension and use of a low-dose diuretic. After reviewing her medications and hydration habits, her physician adjusted her dosage and recommended increasing salt and water intake. Within two weeks, Sarah reported a dramatic reduction in symptoms.
This case illustrates how seemingly minor imbalances—especially involving medication and hydration—can significantly affect circulatory stability.
When to Seek Medical Attention
Occasional, brief blurring that resolves within seconds is usually not concerning. However, certain red flags indicate the need for professional evaluation:
- Symptoms lasting longer than 30 seconds
- Frequent recurrence (daily or multiple times per week)
- Associated chest pain, palpitations, or shortness of breath
- Fainting or near-fainting episodes
- New neurological symptoms like slurred speech or limb weakness
Persistent or worsening symptoms could point to cardiovascular disease, adrenal insufficiency, or neurological disorders requiring targeted treatment.
Step-by-Step Guide to Reduce Episodes
Managing sudden vision blurring involves both immediate behavioral adjustments and long-term lifestyle strategies. Follow this sequence to minimize occurrences:
- Move Gradually: When rising from bed, sit on the edge for 10–15 seconds before standing. This allows your circulation time to adapt.
- Stay Hydrated: Aim for 6–8 glasses of water daily. Increase intake in hot climates or after exercise.
- Review Medications: Discuss all current prescriptions and supplements with your doctor, especially if symptoms began after a change.
- Boost Salt Intake (if advised): For individuals with low blood pressure, modest increases in dietary sodium can help maintain volume—consult your physician first.
- Exercise Regularly: Aerobic activity improves vascular tone and autonomic function. Walking, swimming, or cycling for 30 minutes most days supports better circulation.
- Avoid Triggers: Skip prolonged standing in hot environments, large carbohydrate-heavy meals, and alcohol—all of which can exacerbate blood pooling.
- Monitor Blood Pressure: Use a home monitor to check readings while lying down and again after standing to detect orthostatic drops.
Prevention Checklist
Use this checklist to proactively reduce the likelihood of blurred vision when standing:
- ✅ Rise slowly from sitting or lying positions
- ✅ Drink water consistently throughout the day
- ✅ Wear compression stockings if recommended by your doctor
- ✅ Avoid skipping meals or fasting for extended periods
- ✅ Limit alcohol and caffeine consumption
- ✅ Engage in regular physical activity
- ✅ Review medications with your healthcare provider annually
- ✅ Monitor for signs of dehydration (dry mouth, dark urine)
Frequently Asked Questions
Is blurred vision when standing a sign of low blood sugar?
Not typically. While hypoglycemia can cause blurred vision, dizziness, and confusion, it usually occurs alongside other symptoms like sweating, shaking, and hunger—often unrelated to posture changes. If you have diabetes and experience these symptoms upon standing, check both glucose levels and blood pressure to determine the cause.
Can anxiety cause vision blurring when I stand up?
Anxiety itself doesn’t directly cause orthostatic visual changes, but it can amplify awareness of bodily sensations. Rapid breathing (hyperventilation) during anxiety attacks may alter blood chemistry and contribute to lightheadedness or visual disturbances. However, true orthostatic hypotension should still be ruled out through clinical assessment.
Why do I see black spots or floaters when I stand?
Seeing black spots or “floaters” briefly upon standing is different from generalized blurring. Floaters are usually related to eye anatomy (like vitreous detachment) and aren’t typically caused by blood pressure shifts. However, if they appear suddenly or increase in number, consult an ophthalmologist immediately to rule out retinal issues.
Conclusion: Take Control of Your Circulatory Health
Blurred vision when standing up suddenly is often a manageable condition rooted in circulatory dynamics. By understanding the underlying causes—from simple dehydration to complex neurological regulation—you empower yourself to make informed decisions about your health. Small daily habits—like staying hydrated, moving mindfully, and monitoring symptoms—can prevent discomfort and reduce the risk of falls or injury.
If episodes persist or worsen, don’t hesitate to seek medical advice. Early intervention can uncover treatable conditions and restore confidence in your body’s resilience. Your vision—and overall well-being—is worth protecting.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?