Suddenly standing from a seated or lying position and experiencing blurred vision—or even brief dimming or graying out of sight—is more common than many realize. While often harmless, this symptom can sometimes signal underlying health concerns that shouldn't be ignored. The phenomenon is typically tied to how blood circulates in the body during positional changes. Understanding why it happens, what factors contribute to it, and when it might indicate a serious issue empowers you to respond appropriately.
This article explores the physiological mechanisms behind blurred vision upon standing, identifies key causes, highlights red flags, and offers practical guidance on prevention and when to consult a healthcare provider.
The Science Behind Vision Changes When Standing Up
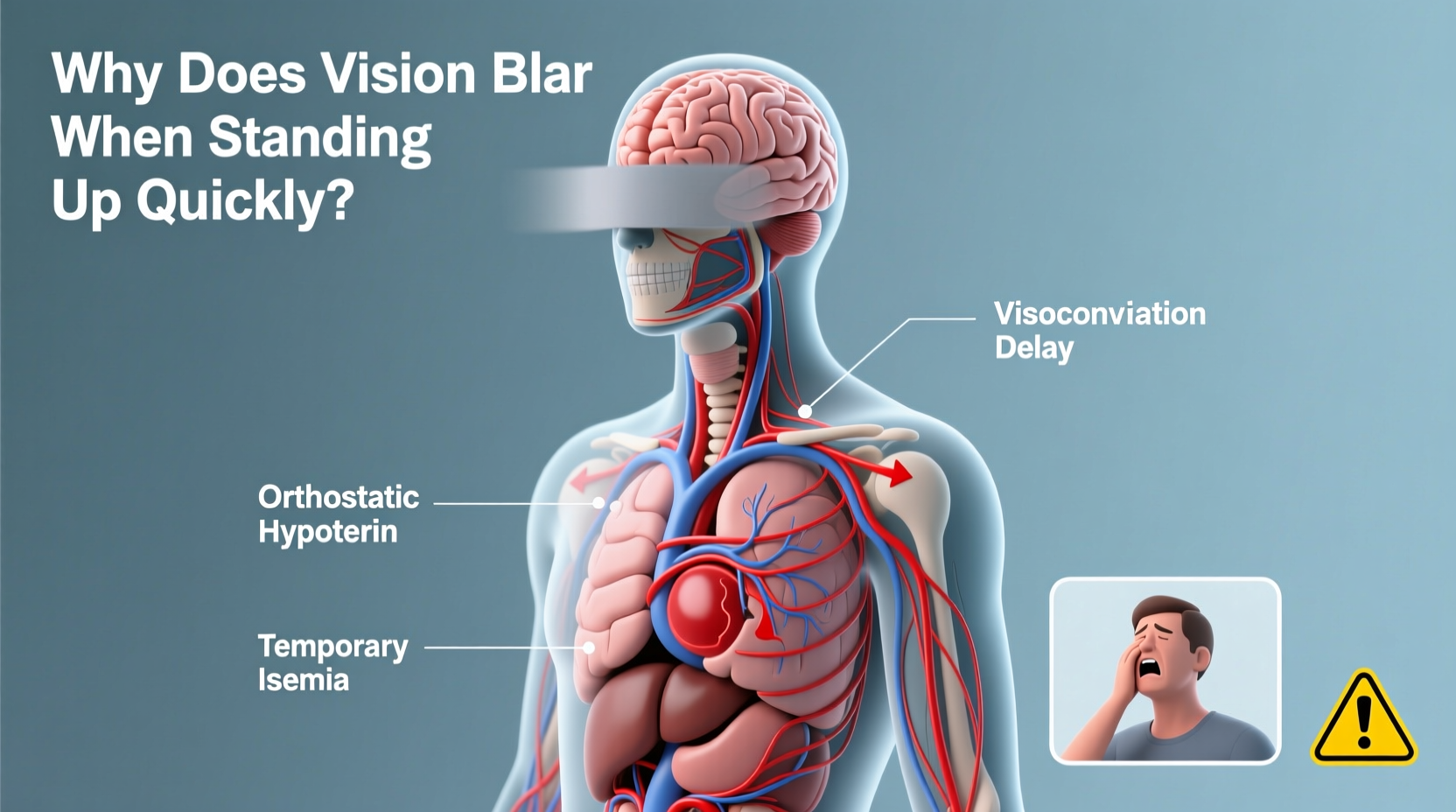
When you transition from sitting or lying down to standing, gravity pulls blood downward into your legs and abdomen. This momentary pooling reduces the amount of blood returning to your heart, which in turn lowers cardiac output and blood pressure. If this drop is significant and rapid, the brain—especially the visual cortex—may receive less oxygenated blood than needed, resulting in temporary visual disturbances like blurring, darkening, or “seeing stars.”
This condition is medically known as **orthostatic hypotension**, or postural hypotension. It's defined as a drop in systolic blood pressure of at least 20 mm Hg or diastolic blood pressure of 10 mm Hg within three minutes of standing. Not everyone with orthostatic hypotension experiences symptoms, but those who do may report:
- Blurred or tunnel vision
- Dizziness or lightheadedness
- Nausea
- Weakness
- Fainting (syncope)
The brain normally compensates for these shifts through the autonomic nervous system, which signals blood vessels to constrict and the heart to beat faster. However, if this reflex response is delayed or impaired, symptoms occur.
Common Causes of Blurred Vision Upon Standing
Several everyday factors can trigger or worsen transient vision blurring when standing. Most are benign and manageable with lifestyle adjustments.
Dehydration
Insufficient fluid intake reduces blood volume, making it harder for the body to maintain stable blood pressure during posture changes. Even mild dehydration—common after exercise, in hot environments, or due to inadequate water consumption—can provoke symptoms.
Low Blood Sugar (Hypoglycemia)
Glucose is essential for brain function. When blood sugar drops, especially in people with diabetes or those who skip meals, cognitive and sensory functions—including vision—can become impaired. This may compound dizziness when standing.
Prolonged Bed Rest or Inactivity
Extended periods of lying down reduce cardiovascular conditioning. The body’s ability to regulate blood pressure diminishes, increasing susceptibility to orthostatic symptoms upon resuming activity.
Medications
Certain drugs interfere with blood pressure regulation. Common culprits include:
- Blood pressure medications (e.g., beta-blockers, ACE inhibitors)
- Diuretics (“water pills”)
- Antidepressants (especially tricyclics)
- Alpha-blockers used for prostate issues
- Parkinson’s disease medications
Alcohol Consumption
Alcohol dilates blood vessels and can dehydrate the body, both of which contribute to low blood pressure and delayed vascular compensation.
Standing Too Quickly
Rapid movement doesn’t allow the autonomic system enough time to respond. Slowing the transition significantly reduces risk.
“Even healthy individuals can experience transient visual blurring when standing too fast, especially if dehydrated or fatigued. But recurrent episodes warrant evaluation.” — Dr. Lena Torres, Neurologist and Autonomic Specialist
When to Worry: Red Flags and Underlying Conditions
Occasional, fleeting blurring that resolves within seconds is usually not concerning. However, persistent or worsening symptoms may point to chronic conditions requiring medical attention.
Chronic Orthostatic Hypotension
Recurrent episodes could indicate an ongoing issue with blood pressure regulation. This is more common in older adults but can affect younger people, particularly those with certain neurological or endocrine disorders.
Autonomic Nervous System Disorders
The autonomic nervous system controls involuntary functions like heart rate and blood vessel tone. Diseases such as **Parkinson’s disease**, **multiple system atrophy (MSA)**, and **pure autonomic failure** impair this system, leading to poor blood pressure control.
Heart Conditions
Arrhythmias, heart valve problems, or heart failure can limit the heart’s ability to pump effectively upon standing, reducing cerebral perfusion.
Anemia
Low red blood cell count reduces oxygen-carrying capacity. Even with normal blood pressure, the brain may not get enough oxygen during sudden movements.
Neurological Issues
Conditions affecting the brain or spinal cord—such as multiple sclerosis or spinal injuries—can disrupt nerve signals involved in blood pressure regulation.
Endocrine Disorders
Adrenal insufficiency (like Addison’s disease) or thyroid dysfunction can interfere with fluid balance and vascular tone.
Prevention and Management Strategies
Most cases of vision blurring upon standing can be improved with simple, consistent lifestyle changes. These strategies focus on supporting circulation and minimizing sudden drops in blood pressure.
Step-by-Step Guide to Safer Position Changes
- Lie flat – Begin in a reclined position.
- Sit up slowly – Move to a seated position and wait 30–60 seconds.
- Dangle legs – Let feet hang off the bed or chair to encourage blood flow redistribution.
- Stand gradually – Use support (like a wall or furniture) and rise slowly.
- Pause and stabilize – Remain still for 10–15 seconds after standing to let your body adjust.
Hydration and Nutrition
Maintain consistent fluid intake throughout the day. Aim for at least 6–8 glasses of water daily, more in hot climates or during physical activity. Some individuals benefit from slightly increased salt intake under medical supervision, as sodium helps retain fluid and raise blood pressure.
Eat balanced meals regularly to avoid blood sugar dips. Include protein-rich snacks between meals if prone to hypoglycemia.
Compression Stockings
These garments apply gentle pressure to the legs, reducing blood pooling and improving venous return. They are especially helpful for those with chronic orthostatic symptoms.
Exercise Regularly
Cardiovascular fitness strengthens the heart and improves vascular responsiveness. Activities like walking, swimming, or cycling enhance circulation and autonomic control over time.
Review Medications
If you're on medication and notice new or worsening symptoms, consult your doctor. Dose adjustments or alternative treatments may alleviate side effects without compromising primary care goals.
Avoid Triggers
Limit alcohol, avoid prolonged standing in hot environments, and don’t skip meals. Be cautious after large meals, as blood diverts to the digestive tract—a phenomenon called **postprandial hypotension**.
| Do’s | Don’ts |
|---|---|
| Stay well-hydrated | Stand up abruptly |
| Rise slowly from bed | Ignore recurring symptoms |
| Wear compression socks if advised | Consume excessive alcohol |
| Monitor symptoms and track patterns | Self-adjust prescribed medications |
| Consult a doctor if symptoms persist | Dismiss fainting as “just getting old” |
Real-Life Example: Recognizing a Hidden Condition
Mark, a 58-year-old office worker, began noticing that he frequently felt “washed out” when standing from his desk chair. At first, he dismissed it as fatigue. Over several months, the episodes became more frequent, sometimes accompanied by nausea and near-fainting. He started keeping notes and brought them to his primary care physician.
After checking his blood pressure lying and standing, the doctor found a 28 mm Hg drop in systolic pressure. Further testing revealed mild autonomic neuropathy, likely related to prediabetes. With early intervention—blood sugar management, hydration, and gradual standing techniques—Mark’s symptoms improved significantly. His case underscores how tracking symptoms can lead to timely diagnosis and prevent complications.
Frequently Asked Questions
Is it normal for young people to experience blurred vision when standing?
Yes, especially if dehydrated, tired, or rising too quickly. However, frequent or severe symptoms in otherwise healthy young adults should be evaluated to rule out conditions like POTS (Postural Orthostatic Tachycardia Syndrome), where heart rate spikes abnormally upon standing.
Can anxiety cause blurred vision when standing?
Anxiety itself doesn’t directly cause orthostatic visual changes, but hyperventilation or panic attacks can alter blood flow and mimic symptoms. Additionally, stress may exacerbate existing blood pressure instability. A thorough assessment helps differentiate psychological from physiological causes.
How is orthostatic hypotension diagnosed?
A simple clinical test involves measuring blood pressure and heart rate after five minutes of lying down, then immediately upon standing and again after one and three minutes. A sustained drop confirms the diagnosis. In complex cases, a tilt-table test may be used for further evaluation.
Action Plan: What You Should Do Now
If you’ve experienced blurred vision when standing, start by evaluating your habits. Are you drinking enough water? Do you stand up too fast? Are you on medications that affect blood pressure? Implement the step-by-step rising technique and monitor your symptoms for a week.
If episodes continue more than once or twice a week, worsen, or are accompanied by chest pain, palpitations, confusion, or fainting, schedule an appointment with your healthcare provider. Early assessment can identify reversible causes and prevent falls or injury from sudden loss of balance.
“Patients often wait too long to report these symptoms, assuming they’re just part of aging. But we can often improve quality of life significantly with proper diagnosis and management.” — Dr. Alan Meeks, Internal Medicine Specialist
Conclusion
Blurred vision when standing up quickly is often a minor, temporary event caused by simple physiological shifts. However, it can also be an early warning sign of conditions affecting circulation, nerves, or metabolism. By understanding the causes, recognizing red flags, and taking proactive steps—from slowing your movements to seeking medical advice—you protect both your immediate safety and long-term health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?