Suddenly standing from a seated or lying position and experiencing blurred vision—or even brief dizziness, dimming of sight, or tunnel vision—is more common than many realize. While often fleeting and harmless, this phenomenon can be unsettling and sometimes signals an underlying health concern. The root cause typically lies in how your cardiovascular and nervous systems respond to gravity-induced shifts in blood flow. Understanding the science behind this reaction empowers you to recognize when it’s normal and when it may require medical attention.
The Science Behind Blurred Vision Upon Standing
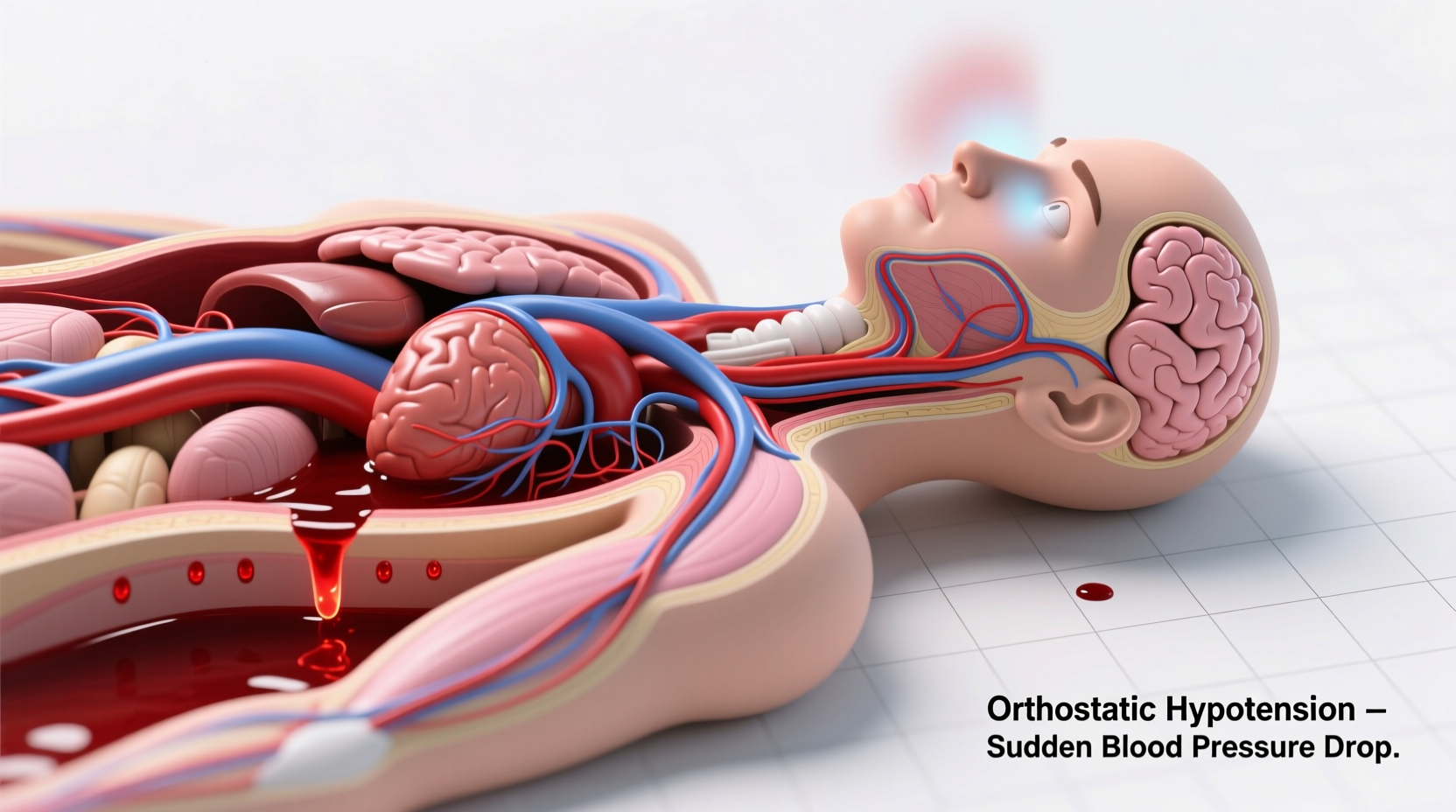
When you stand up quickly, gravity pulls blood downward into your legs and abdomen. This temporary pooling reduces the amount of blood returning to your heart, which in turn lowers cardiac output and blood pressure. As a result, less oxygen-rich blood reaches your brain for a few seconds—particularly affecting the visual cortex and other sensitive neural regions.
This momentary drop in cerebral perfusion can lead to visual disturbances such as:
- Blurred or hazy vision
- Tunnel vision (peripheral vision loss)
- Seeing \"stars\" or flashes
- Dizziness or lightheadedness
- Nausea or weakness
The body normally compensates almost instantly through a reflex known as the baroreceptor reflex. Baroreceptors in the carotid arteries and aortic arch detect the pressure drop and signal the autonomic nervous system to increase heart rate and constrict blood vessels, restoring blood pressure and brain blood flow within seconds.
However, if this regulatory mechanism is delayed or impaired, symptoms like blurred vision persist longer—sometimes lasting several seconds to a minute.
Orthostatic Hypotension: The Primary Culprit
The medical term for low blood pressure upon standing is orthostatic hypotension, also known as postural hypotension. It's defined as a drop of at least 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic pressure within three minutes of standing.
Orthostatic hypotension directly correlates with transient vision changes. When brain oxygen levels dip due to reduced perfusion, visual processing slows down, leading to blurring or graying out of vision. In severe cases, people may even faint (syncope).
Common triggers include:
- Dehydration
- Prolonged bed rest
- Medications (e.g., antihypertensives, diuretics, antidepressants)
- Alcohol consumption
- Standing after eating (postprandial hypotension)
“Even healthy individuals can experience mild orthostatic symptoms, but recurrent or severe episodes should prompt evaluation.” — Dr. Lena Torres, Neurologist and Autonomic Specialist
Who Is at Higher Risk?
While anyone can experience brief vision blurring upon standing, certain groups are more susceptible due to age-related changes or preexisting conditions.
| Risk Group | Why They’re Vulnerable |
|---|---|
| Older Adults (65+) | Age diminishes baroreflex sensitivity and vascular tone; medications and chronic conditions compound risk. |
| People with Diabetes | Diabetic neuropathy can damage autonomic nerves that regulate blood pressure. |
| Those on Blood Pressure Medications | Drugs like beta-blockers or ACE inhibitors may overcorrect, causing excessive drops upon posture change. |
| Individuals with Parkinson’s Disease | Autonomic dysfunction is common, impairing the body’s ability to stabilize blood pressure. |
| People with Anemia or Low Blood Volume | Reduced red blood cells or plasma volume limits oxygen delivery during sudden shifts. |
Real-Life Example: A Case of Recurrent Blurring
Maria, a 72-year-old retired teacher, began noticing that every time she stood up from her favorite armchair, her vision would blur for about 10 seconds. At first, she dismissed it as aging. But when the episodes became more frequent—and once led to a near-fall—she consulted her doctor.
Blood tests revealed mild anemia and dehydration. Her blood pressure dropped from 130/80 mm Hg while seated to 105/68 mm Hg upon standing. After increasing fluid intake, adjusting her hypertension medication, and adopting slower rising habits, Maria’s symptoms resolved within two weeks.
Her case illustrates how multiple factors can converge to disrupt blood pressure regulation—and how simple interventions can make a significant difference.
Other Possible Causes Beyond Orthostasis
While orthostatic hypotension is the most common explanation, other conditions may contribute to or mimic this symptom:
- Inner Ear Disorders: Conditions like benign paroxysmal positional vertigo (BPPV) affect balance and can distort spatial awareness, sometimes accompanied by visual disturbance.
- Low Blood Sugar (Hypoglycemia): Especially in diabetics, sudden drops in glucose can cause blurry vision, shakiness, and confusion—regardless of posture.
- Eye-Related Issues: Dry eyes, uncorrected refractive errors, or optic nerve problems may worsen temporarily under stress but aren’t typically triggered solely by standing.
- Cardiac Arrhythmias: Irregular heartbeats can reduce cardiac output abruptly, mimicking orthostatic symptoms.
- Autonomic Nervous System Disorders: Rare conditions like pure autonomic failure or multiple system atrophy severely impair blood pressure control.
If blurred vision occurs without postural change, or is accompanied by double vision, speech difficulties, or limb weakness, seek immediate medical evaluation to rule out neurological emergencies like stroke.
Practical Steps to Reduce Episodes
You don’t have to live with recurring visual disturbances when changing positions. Implementing targeted lifestyle adjustments can significantly reduce or eliminate symptoms.
Step-by-Step Guide to Safer Position Changes
- Sit up slowly: If lying down, first roll to your side and prop yourself up on your elbows before fully sitting.
- Dangle legs off the bed: Before standing in the morning, let your legs hang for 30–60 seconds to allow circulation to adjust.
- Contract leg muscles: While seated or before rising, tense your calves and thighs to push blood upward.
- Stand still initially: After standing, pause for a few moments before walking to let your blood pressure stabilize.
- Stay hydrated: Drink water consistently throughout the day, especially in hot weather or after exercise.
Checklist: Prevent Blurred Vision When Standing
- ✅ Rise slowly from sitting or lying positions
- ✅ Stay well-hydrated (aim for 6–8 glasses of water daily)
- ✅ Review medications with your doctor for blood pressure effects
- ✅ Avoid large carbohydrate-heavy meals that trigger postprandial drops
- ✅ Wear compression stockings if recommended (improves venous return)
- ✅ Monitor blood pressure at home in different positions
- ✅ Limit alcohol and caffeine, which can dehydrate and affect circulation
When to See a Doctor
Occasional, brief blurring upon standing is usually not dangerous. However, consult a healthcare provider if you experience any of the following:
- Frequent or worsening episodes
- Symptoms lasting more than a minute
- Fainting or near-fainting
- Chest pain, palpitations, or shortness of breath
- Confusion, slurred speech, or muscle weakness
- History of heart disease, diabetes, or neurological disorders
Your doctor may perform a tilt-table test, check autonomic function, or order blood work to assess hemoglobin, electrolytes, and hormone levels. Treatment depends on the underlying cause but may include medication adjustment, fluid management, or physical counter-maneuvers.
FAQ: Common Questions About Vision Blurring Upon Standing
Is it normal for young people to experience blurred vision when standing up?
Yes, even healthy young adults can experience mild symptoms, especially if dehydrated, fatigued, or standing too quickly. However, persistent or severe blurring warrants evaluation to rule out arrhythmias, anemia, or autonomic issues.
Can anxiety cause vision blurring when standing?
Anxiety itself doesn’t directly cause orthostatic symptoms, but hyperventilation during anxious episodes can lower carbon dioxide levels in the blood, leading to vasoconstriction and reduced cerebral blood flow—which may mimic or worsen visual disturbances.
Are there exercises that help prevent this?
Yes. Regular aerobic activity improves cardiovascular fitness and autonomic regulation. Additionally, practicing “counter-pressure maneuvers” like crossing your legs and tensing your thighs can help maintain blood pressure when standing. Physical therapists may recommend specific exercises for those with chronic orthostatic intolerance.
Conclusion: Listen to Your Body, Act Proactively
Blurred vision when standing up suddenly is often a minor, correctable issue rooted in circulatory dynamics. But it shouldn’t be ignored when it becomes routine or disruptive. Your body uses these moments as signals—subtle warnings that something in your hydration, medication, or health may need recalibration.
By understanding the mechanisms behind orthostatic changes, identifying personal risk factors, and applying practical strategies, you can regain confidence in your daily movements. Don’t dismiss repeated episodes as just “getting older.” Take control with small, sustainable changes that support long-term circulatory and neurological health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?