Have you ever stood up quickly from a seated or lying position only to feel dizzy, lightheaded, or notice your vision momentarily fading or blurring? You're not alone. This common experience—often dismissed as a minor inconvenience—can be both unsettling and disruptive. While occasional episodes are usually harmless, frequent or severe symptoms may signal underlying health issues that deserve attention.
This phenomenon is medically recognized as orthostatic hypotension, or postural hypotension—a temporary drop in blood pressure upon standing. When it happens, the brain receives less oxygen-rich blood for a few seconds, causing visual disturbances, dizziness, or even fainting. Understanding why this occurs and how to manage it can improve daily comfort and long-term cardiovascular health.
What Happens to Your Body When You Stand Up?
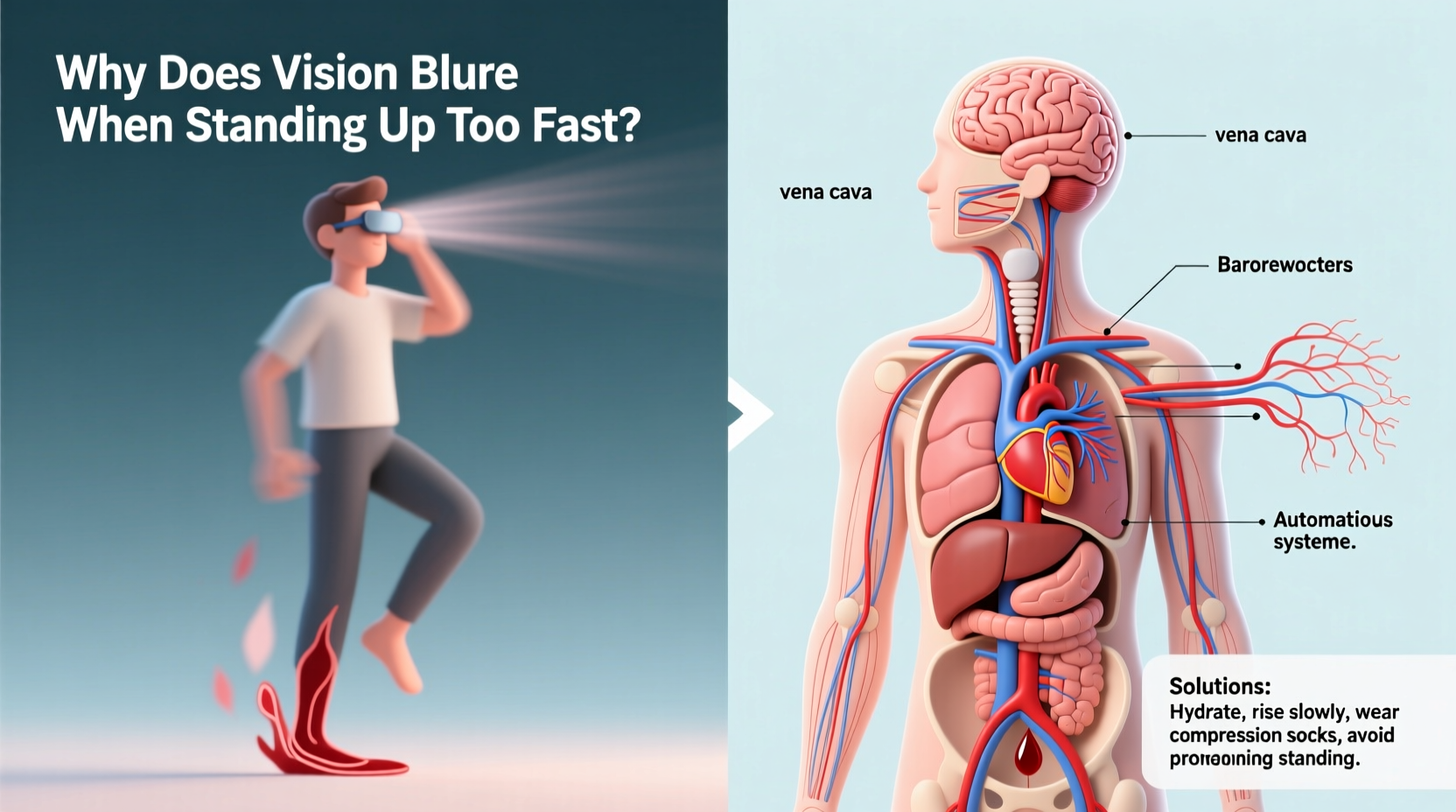
When you transition from sitting or lying down to standing, gravity pulls blood downward into your legs and abdomen. In response, your body must rapidly adjust to maintain consistent blood flow to the brain. Normally, the autonomic nervous system triggers several compensatory mechanisms:
- Narrowing of blood vessels (vasoconstriction) to increase resistance and keep blood pressure stable.
- A slight increase in heart rate to pump more blood upward.
- Activation of baroreceptors—pressure sensors in major arteries—that signal the brain to regulate blood pressure.
When any part of this system fails to respond quickly enough, blood pressure drops temporarily. As cerebral perfusion decreases, the brain struggles to function at full capacity, resulting in symptoms such as blurred vision, tunnel vision, dizziness, weakness, or nausea.
Common Causes of Blurred Vision Upon Standing
Several factors can impair your body’s ability to regulate blood pressure during positional changes. Some are benign and easily corrected; others require medical evaluation.
1. Dehydration
Insufficient fluid intake reduces blood volume, making it harder for the circulatory system to maintain adequate pressure. Dehydration is especially common in hot climates, during illness, or after intense exercise without proper rehydration.
2. Medications
Certain drugs directly affect blood pressure regulation. These include:
- Diuretics (water pills)
- Alpha-blockers used for high blood pressure or prostate conditions
- Antidepressants, particularly tricyclics
- Parkinson’s disease medications
- Vasodilators and erectile dysfunction drugs
3. Age-Related Changes
As people age, the autonomic nervous system becomes less responsive. Blood vessels lose elasticity, and baroreceptor sensitivity declines, increasing susceptibility to orthostatic drops in blood pressure. It's estimated that up to 30% of adults over 70 experience symptomatic orthostatic hypotension.
4. Prolonged Bed Rest or Inactivity
Extended periods of immobility weaken cardiovascular conditioning. When someone who has been bedridden stands up, their circulatory system may struggle to adapt, leading to pronounced drops in blood pressure.
5. Underlying Medical Conditions
Chronic diseases can interfere with autonomic control. Key contributors include:
- Diabetes: Can damage nerves involved in blood pressure regulation (autonomic neuropathy).
- Parkinson’s disease: Often impairs autonomic function.
- Heart conditions: Arrhythmias, valve problems, or heart failure limit cardiac output.
- Anemia: Low red blood cell count reduces oxygen delivery, exacerbating symptoms.
6. Postprandial Hypotension
Blood pressure can drop significantly within 30–60 minutes after eating, especially large meals rich in carbohydrates. Digestion redirects blood flow to the intestines, leaving less available for the brain when standing.
“Orthostatic hypotension isn’t just about dizziness—it’s a window into cardiovascular and neurological health.” — Dr. Laura Nguyen, Neurologist and Autonomic Specialist
Do’s and Don’ts: Managing Orthostatic Symptoms
| Do’s | Don’ts |
|---|---|
| Increase fluid intake, especially water and electrolyte drinks if sweating heavily. | Stand up abruptly after lying down or sleeping. |
| Raise the head of your bed slightly (6–8 inches) to help maintain overnight blood pressure. | Consume large carbohydrate-heavy meals if prone to post-meal dizziness. |
| Wear compression stockings to reduce blood pooling in the legs. | Ignore recurring symptoms—especially if accompanied by falls or confusion. |
| Engage in regular physical activity to improve circulation and vascular tone. | Overuse alcohol, which dilates blood vessels and worsens hypotension. |
| Review medications with your doctor to identify those affecting blood pressure. | Skip meals or go long periods without eating, risking low blood sugar and pressure. |
Step-by-Step Guide to Preventing Vision Blurring When Standing
If you frequently experience blurred vision upon standing, follow this practical timeline to minimize risk and improve stability.
- Before Rising (0–10 seconds): When waking from sleep or rising after sitting, pause. Sit on the edge of the bed or chair for 10–15 seconds to allow your circulation to adjust.
- Muscle Pump Activation (10–20 seconds): Gently tense your leg muscles and wiggle your toes. This helps push blood back toward the heart through muscle contractions.
- Slow Standing (20–30 seconds): Rise gradually. Use your arms for support if needed. Avoid jerky movements.
- Pause and Stabilize (30–45 seconds): Once upright, remain still for a few moments. Breathe deeply and assess how you feel before walking.
- Daily Prevention Habits: Stay hydrated, eat balanced small-to-moderate meals, wear supportive footwear, and consider waist-high compression garments if recommended by a physician.
- Weekly Check-In: Monitor symptom frequency. Keep a simple log noting time of day, recent food intake, medications, and severity of symptoms.
Real-Life Example: Maria’s Experience with Orthostatic Hypotension
Maria, a 68-year-old retired teacher, began noticing frequent dizziness and blurry vision when getting up from her recliner or bed. At first, she attributed it to aging. But after nearly falling one morning while rushing to answer the phone, she consulted her primary care physician.
Her doctor reviewed her medications—she was taking a diuretic for mild hypertension and an older antidepressant—and measured her blood pressure lying down and standing. Her systolic pressure dropped from 130 mmHg to 98 mmHg within three minutes of standing, confirming orthostatic hypotension.
The solution involved several steps: switching to a different antidepressant with fewer cardiovascular side effects, adjusting her diuretic dose, adding a recommendation for increased salt and fluid intake (under supervision), and advising her to perform “pre-rise” exercises like ankle pumps. Within two weeks, Maria reported dramatic improvement. She now rises slowly, keeps water by her bedside, and uses a raised toilet seat to make standing easier.
When to Seek Medical Attention
While occasional lightheadedness is normal, certain warning signs warrant prompt evaluation:
- Frequent or worsening episodes of blurred vision or dizziness
- Loss of consciousness, even briefly
- Chest pain or palpitations during episodes
- Confusion, slurred speech, or difficulty walking
- Symptoms occurring without positional change
Persistent orthostatic hypotension can increase fall risk, especially in older adults, and may indicate serious neurological or cardiac disorders. Diagnostic tests may include tilt-table testing, echocardiograms, blood work (for anemia, electrolytes, glucose), and autonomic function assessments.
FAQ: Common Questions About Blurry Vision When Standing
Can low blood sugar cause blurred vision when standing?
Yes. Hypoglycemia (low blood sugar) can mimic or worsen orthostatic symptoms. Both conditions reduce energy supply to the brain, leading to dizziness, blurred vision, shakiness, and confusion. People with diabetes should monitor blood glucose levels when experiencing these symptoms.
Is it dangerous if my vision blacks out for a few seconds when I stand?
Occasional brief episodes are typically not dangerous, but they do indicate a significant drop in cerebral blood flow. Recurrent blackouts increase the risk of falls and injury. They should be evaluated, especially if they occur multiple times per week or lead to near-falls.
Can exercise help prevent this issue?
Absolutely. Regular aerobic and resistance training improves vascular tone, enhances autonomic reflexes, and strengthens the muscles involved in venous return. Exercises like walking, cycling, swimming, and leg lifts can all contribute to better blood pressure stability.
Checklist: What You Can Do Today
Use this actionable checklist to reduce the frequency and severity of vision blurring when standing:
- ✅ Drink at least 6–8 glasses of water daily (more in heat or after exercise).
- ✅ Rise slowly from sitting or lying positions—pause for 10–15 seconds.
- ✅ Review all medications with your doctor, including over-the-counter drugs.
- ✅ Eat smaller, more frequent meals to avoid postprandial drops.
- ✅ Perform gentle leg exercises before standing (ankle circles, calf raises).
- ✅ Consider wearing compression stockings if approved by your healthcare provider.
- ✅ Monitor symptoms and keep a short journal for your next medical visit.
- ✅ Avoid excessive alcohol and caffeine, both of which can dehydrate and affect circulation.
“Prevention starts with awareness. Many patients don’t report these symptoms because they think they’re normal. But they’re treatable.” — Dr. Rajiv Mehta, Cardiologist
Conclusion
Blurred vision when standing up too fast is more than just a fleeting annoyance—it’s a physiological signal that your body is struggling to maintain stable blood flow to the brain. While often benign, repeated episodes should not be ignored. Simple lifestyle adjustments like staying hydrated, moving deliberately, and reviewing medications can make a profound difference.
For some, underlying medical conditions may need targeted treatment. The key is recognizing patterns, responding proactively, and seeking professional guidance when necessary. By understanding the causes and applying practical solutions, you can regain confidence in your daily movements and protect your long-term health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?