Phlegm is a thick, often sticky fluid produced by the respiratory system that many people encounter during colds, allergies, or infections. While it’s a natural part of the body’s defense mechanism, excessive or discolored phlegm can signal underlying issues. Understanding why phlegm forms, what it does, and when it becomes a cause for concern helps individuals make informed decisions about their health.
The Role of Phlegm in the Body
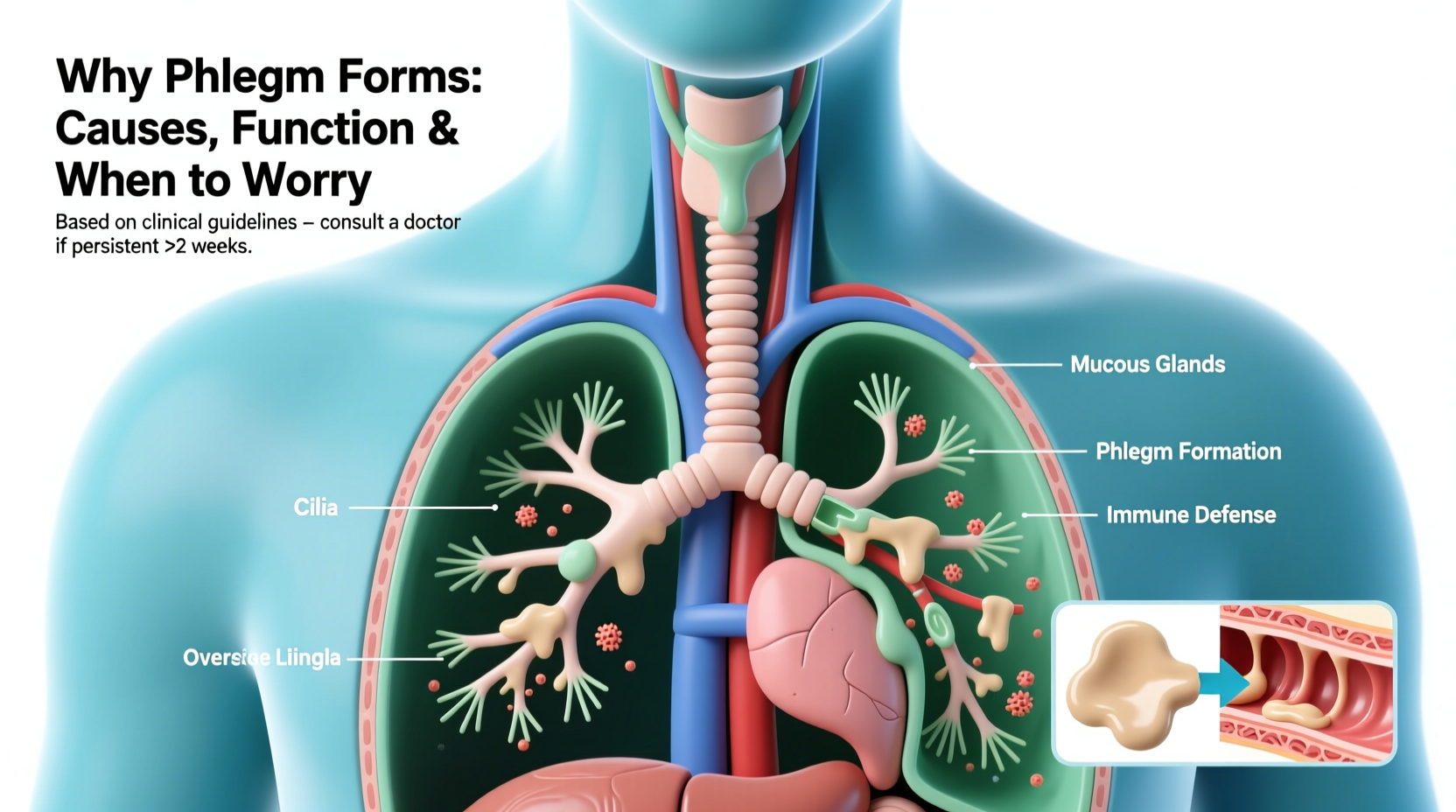
Phlegm is a type of mucus specifically produced by the lower airways — the trachea and bronchi — in response to irritation or infection. Unlike nasal mucus, which drains from the sinuses, phlegm is coughed up from the lungs and throat. Its primary function is protective: it traps foreign particles like dust, bacteria, viruses, and allergens, preventing them from reaching deeper into the lungs.
The respiratory tract is lined with cilia — tiny hair-like structures — that move in coordinated waves to push phlegm upward so it can be expelled through coughing or swallowed. This mucociliary clearance is essential for maintaining clean, functional airways.
“Phlegm is not just a nuisance — it’s one of the lungs’ first lines of defense. Without it, we’d be far more vulnerable to respiratory infections.” — Dr. Alan Reyes, Pulmonologist at National Respiratory Institute
Common Causes of Phlegm Production
Phlegm production increases when the respiratory system detects a threat. The following are among the most frequent triggers:
- Viral infections: Colds and flu stimulate mucus glands to produce more phlegm as a barrier against spreading pathogens.
- Bacterial infections: Conditions like bronchitis or pneumonia often result in thick, colored phlegm due to white blood cells and dead bacteria.
- Allergies: Pollen, mold, and pet dander trigger immune responses that increase mucus secretion.
- Asthma: Chronic inflammation leads to excess mucus, especially during flare-ups.
- Smoking: Tobacco smoke irritates the airways, causing chronic phlegm production — commonly known as “smoker’s cough.”
- Environmental irritants: Air pollution, chemical fumes, and dry air can all prompt the body to generate protective phlegm.
- Gastroesophageal reflux disease (GERD): Stomach acid rising into the throat can irritate tissues and lead to persistent mucus buildup.
Color and Consistency: What They Reveal
The appearance of phlegm offers clues about its cause. While clear or white phlegm is usually benign, changes in color may indicate progression or severity of illness.
| Color | Possible Meaning | When to Monitor |
|---|---|---|
| Clear | Normal mucus; mild irritation or allergies | No concern unless volume is excessive |
| White | Viral infection or congestion; may indicate swollen airways | If persistent beyond 10 days |
| Yellow | Immune activity; white blood cells fighting infection | Common in later stages of colds |
| Green | Bacterial presence or prolonged infection | Warrants evaluation if lasting over a week |
| Brown/Gray | Inhalation of smoke, dirt, or pollutants | Especially common in smokers |
| Pink or Red | Blood in phlegm (hemoptysis); possible tissue irritation or serious condition | Seek medical advice immediately |
| Rusty or Dark Brown | Old blood or chronic lung disease (e.g., bronchiectasis) | Requires prompt evaluation |
When to Worry: Red Flags and Warning Signs
While occasional phlegm is normal, certain symptoms suggest a need for medical attention. Persistent or worsening signs may point to chronic conditions or serious infections.
Key Warning Signs
- Duration: Phlegm lasting more than three weeks without improvement may indicate chronic bronchitis, asthma, or another ongoing condition.
- Blood in phlegm: Even small amounts of red or pink-tinged mucus should be evaluated, as they can stem from infections, bronchitis, or, rarely, lung cancer.
- Fever above 101°F (38.3°C) lasting over 48 hours: Suggests a bacterial infection such as pneumonia.
- Shortness of breath or chest pain: These may signal pneumonia, pulmonary embolism, or heart-related issues.
- Unexplained weight loss or night sweats: When paired with chronic phlegm, these could indicate tuberculosis or malignancy.
- Wheezing or stridor: Noisy breathing may reflect airway obstruction or severe asthma.
Real-Life Example: Recognizing a Hidden Infection
Sarah, a 42-year-old teacher, noticed she had been coughing up green phlegm for nearly two weeks after a cold. She assumed it was lingering post-viral mucus and tried over-the-counter expectorants. However, she began experiencing sharp chest pain when breathing deeply and developed a fever of 102°F. Concerned, she visited her primary care physician, who ordered a chest X-ray. The scan revealed a pocket of infection consistent with bacterial pneumonia. With a course of antibiotics and rest, Sarah recovered fully within 10 days.
This case illustrates how seemingly routine phlegm can mask a serious condition when accompanied by systemic symptoms. Early recognition and medical evaluation prevented complications.
Managing Phlegm: Practical Steps You Can Take
Most cases of increased phlegm resolve on their own with supportive care. The goal is to thin the mucus, support the body’s natural clearance mechanisms, and reduce irritation.
Step-by-Step Guide to Easing Phlegm Discomfort
- Stay Hydrated: Drink plenty of water throughout the day. Warm liquids like herbal teas or broths are especially effective at loosening mucus.
- Use a Humidifier: Moist air prevents drying of the airways, particularly helpful in heated indoor environments during winter.
- Gargle with Salt Water: A simple solution (1/2 tsp salt in warm water) soothes the throat and may help dislodge mucus.
- Elevate Your Head While Sleeping: Reduces postnasal drip and nighttime coughing.
- Avoid Irritants: Steer clear of cigarette smoke, strong perfumes, and polluted air.
- Try Expectorants: Over-the-counter medications containing guaifenesin help thin and loosen mucus for easier expulsion.
- Practice Controlled Coughing: Take a slow breath in, hold briefly, then use your abdominal muscles to cough forcefully — this clears mucus more effectively than shallow hacking.
Do’s and Don’ts for Managing Phlegm
| Do’s | Don’ts |
|---|---|
| Drink warm fluids regularly | Smoke or expose yourself to secondhand smoke |
| Use saline nasal sprays | Suppress a productive cough completely |
| Rest to support immune function | Use decongestants long-term without medical advice |
| Monitor phlegm changes daily | Ignore blood or rust-colored phlegm |
| Wash hands frequently to prevent reinfection | Self-prescribe antibiotics |
FAQ: Common Questions About Phlegm
Is it safe to swallow phlegm?
Yes. Swallowing phlegm is harmless for most people. Once ingested, stomach acids destroy any trapped bacteria or viruses. It’s a natural part of the clearance process.
Can allergies cause green phlegm?
Occasionally. While green phlegm is typically linked to bacterial infections, prolonged allergic inflammation can lead to stagnant mucus that becomes discolored due to concentrated immune cells. However, if symptoms persist, a secondary infection should be ruled out.
Why do I have more phlegm in the morning?
During sleep, mucus accumulates in the airways because swallowing and ciliary movement slow down. Upon waking, the body works to clear this buildup, leading to increased coughing and phlegm production early in the day.
Conclusion: Listen to Your Body and Act Wisely
Phlegm formation is a vital, protective response designed to keep your lungs healthy. Most episodes are temporary and manageable with home care. However, ignoring persistent symptoms or dismissing alarming signs like blood or difficulty breathing can delay treatment of potentially serious conditions.
Understanding the causes and functions of phlegm empowers you to distinguish between normal immune activity and signals that require professional evaluation. By staying informed and responsive to your body’s cues, you take meaningful steps toward better respiratory health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?