The human body is full of subtle anatomical features that often go unnoticed—until they spark curiosity. One such feature is the vertical line running from the anus through the scrotum, commonly referred to as the \"stitch line.\" This structure, medically known as the raphe, is not a scar or defect but a natural result of embryonic development. Understanding the raphe offers insight into how male genitalia form and underscores the precision of prenatal biology.
This line may appear prominent in some individuals and faint in others, but its presence is universal in males. While it typically raises no health concerns, misconceptions about its origin persist. This article explores the science behind the raphe, its developmental journey, clinical relevance, and what variations are considered normal.
What Is the Raphe?
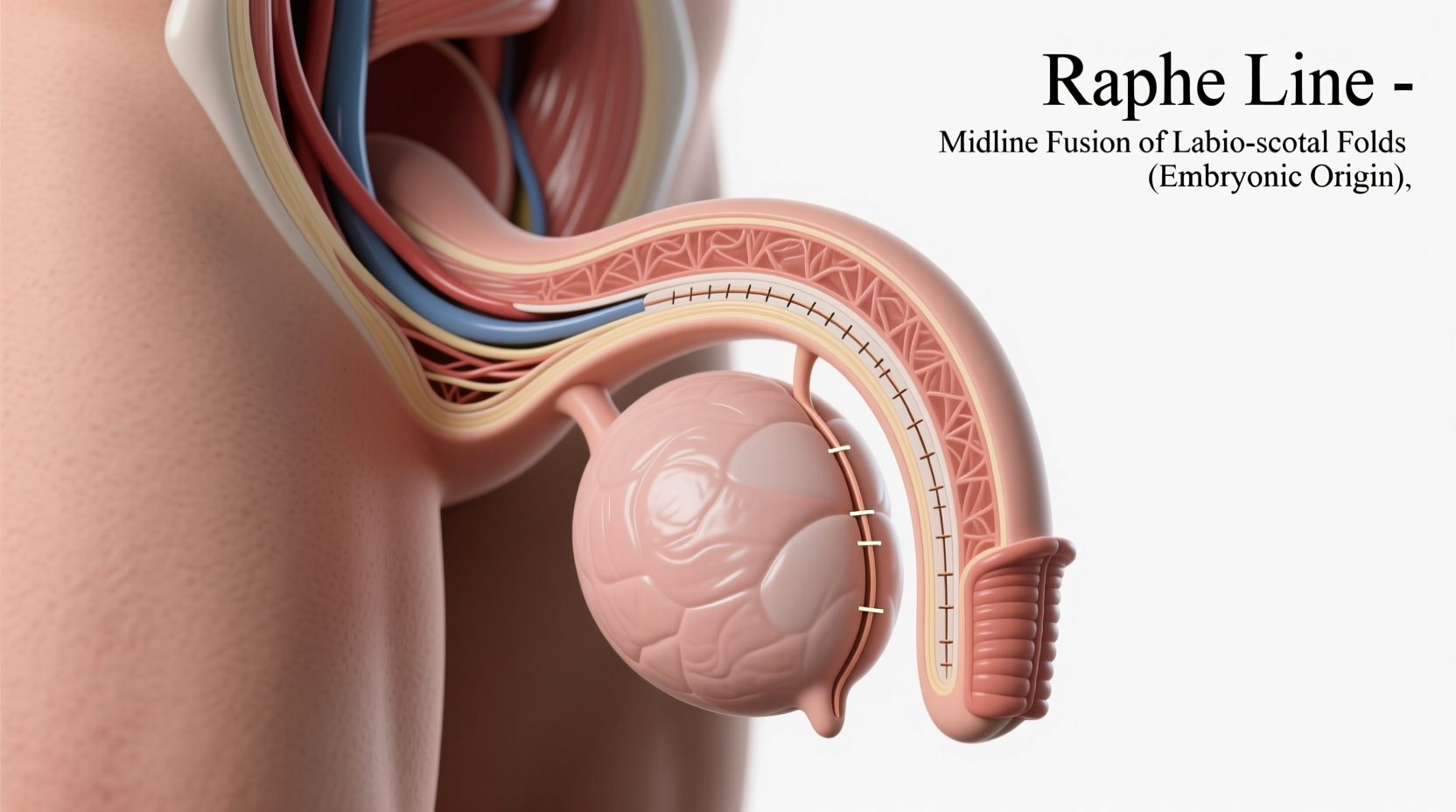
The raphe is a visible ridge of tissue that extends from the anus up through the perineum and along the underside of the penis or scrotum. In males, it marks the point where two embryonic structures fused during development. The term comes from the Greek word *rhaphē*, meaning \"seam,\" which accurately describes its appearance and function.
This line is present in both sexes, though it manifests differently. In females, the labia minora meet at the midline, forming a less noticeable perineal raphe. In males, the raphe runs continuously from the anus to the base of the glans, often continuing onto the ventral side of the penis.
“Every male carries a visible reminder of their earliest development—the raphe is nature’s suture, marking where bilateral tissues united.” — Dr. Alan Pierce, Developmental Biologist
Embryology: How the Raphe Forms
The story of the raphe begins in the first trimester of fetal development. Initially, all embryos follow a similar blueprint, regardless of genetic sex. Around week 6–7, sexual differentiation begins under the influence of hormones, primarily testosterone in male (XY) fetuses.
Two key structures—the urogenital folds and labioscrotal swellings—start as paired, symmetrical tissues on either side of the genital tubercle. In males, rising testosterone levels trigger these folds and swellings to grow toward the midline. As they meet, they fuse together:
- The urogenital folds close over the developing urethra, forming the penile shaft and urethral tube.
- The labioscrotal swellings merge to create the single, divided sac of the scrotum.
This fusion process creates the raphe. Think of it like zipping up a jacket: the two sides come together, sealing along a central line. The raphe is the healed seam where this union occurred. Without this precise fusion, proper formation of the scrotum and urethra would not be possible.
Clinical Significance of the Raphe
While the raphe itself is benign, its development is crucial. Errors in fusion can lead to congenital conditions that require medical attention. These include:
- Hypospadias: A condition where the urethral opening forms on the underside of the penis instead of the tip, indicating incomplete closure of the urogenital folds.
- Bifid scrotum: A partial or complete failure of the labioscrotal swellings to fuse, resulting in a cleft scrotum.
- Epispadias: A rarer condition where the urethra opens on the upper side of the penis due to faulty development.
These conditions underscore the importance of proper embryological timing and hormonal signaling. Most are diagnosed at birth and corrected surgically in infancy with high success rates.
Raphe Abnormalities and When to Seek Help
In adulthood, changes along the raphe—such as lumps, sores, or persistent pain—may signal infection, cysts, or rarely, malignancy. For example:
- Epidermoid cysts can develop along the raphe due to trapped skin cells.
- Perineal abscesses may arise from blocked glands or infections in hair follicles.
- Pearly penile papules sometimes align near the coronal ridge but are unrelated; true raphe lesions should be evaluated by a urologist.
Any new or changing lesion along the raphe warrants medical evaluation to rule out serious conditions like squamous cell carcinoma, especially in uncircumcised men or those with HPV exposure.
Normal Variations of the Raphe
The appearance of the raphe varies widely among healthy individuals. Factors influencing its visibility include:
- Skin pigmentation (darker in some)
- Texture (smooth, raised, or slightly ridged)
- Length (may extend fully or partially)
- Pigmentation changes during puberty due to hormonal shifts
It is not uncommon for the raphe to be more pronounced after puberty, as increased melanin production and tissue growth enhance its definition. Some men report a darker line, while others barely notice it.
| Variation Type | Description | Normal or Concerning? |
|---|---|---|
| Thin, pale line | Faint ridge with little pigmentation | Normal |
| Dark, prominent ridge | Clearly visible, possibly raised or pigmented | Normal |
| Lump or nodule | New mass along the raphe | Concerning – seek evaluation |
| Open cleft in scrotum | Visible separation at midline | May indicate bifid scrotum – requires diagnosis |
Common Misconceptions About the Scrotal Seam
Because the raphe resembles a surgical incision, many assume it results from circumcision, injury, or disease. None of these are correct. The raphe is not:
- A scar from birth trauma
- Related to circumcision (which affects the foreskin, not midline fusion)
- A sign of abnormality in otherwise healthy males
It is also not unique to humans. The raphe appears in most mammals, particularly those with external testes, reinforcing its role in reproductive anatomy across species.
Mini Case Study: A Patient’s Concern
A 24-year-old man visited a urology clinic concerned about a “weird line” on his scrotum he’d noticed since adolescence. He feared it was a birth defect or undiagnosed surgery. After examination, the physician explained the raphe’s embryological origin, reassured him it was normal, and noted only mild pigmentation—common in his ethnic background. The patient left relieved, having mistaken a natural anatomical landmark for a medical issue.
This case highlights how lack of education about basic anatomy can fuel unnecessary anxiety. Open dialogue in healthcare settings can demystify such features.
Frequently Asked Questions
Is the raphe a sign of surgery or trauma?
No. The raphe is a natural line formed during fetal development when tissues fuse to create the scrotum and penile urethra. It is not related to any surgical procedure or injury.
Can the raphe change over time?
Yes. During puberty, hormonal changes may darken or make the raphe more prominent due to increased melanin and tissue growth. Minor changes are normal, but sudden lumps or sores should be checked.
Do women have a raphe?
Yes, but it’s less visible. In females, the labioscrotal folds become the labia majora, meeting at the midline to form a subtle perineal raphe extending from the anus to the posterior fourchette.
Actionable Checklist: What to Do If You're Concerned
- Examine the raphe in good lighting to assess symmetry and texture.
- Note any changes: color, swelling, pain, or discharge.
- Compare current appearance to old photos, if available.
- Avoid squeezing or picking at any bumps.
- Schedule a visit with a urologist or primary care provider if you observe new or growing lesions.
Conclusion: Embracing Anatomical Literacy
The scrotal raphe is far more than a curious line—it’s a testament to the intricate choreography of human development. Its presence reflects a critical phase in fetal growth, where symmetry becomes singularity, and potential becomes form. Recognizing it as a normal, functional landmark fosters better self-awareness and reduces stigma around male anatomy.
Understanding your body isn’t just empowering—it’s essential for timely health decisions. If something changes along the raphe, don’t ignore it. But equally, don’t fear what’s simply part of your natural design.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?