Have you ever stood up quickly from a seated or lying position and suddenly felt lightheaded, dizzy, or noticed your vision going dark or blurry for a few seconds? You're not alone—and more importantly, it’s not usually cause for alarm. This common experience is often due to a temporary drop in blood pressure known as orthostatic hypotension. While typically brief and harmless, understanding why it happens can help you recognize when it's just a fleeting moment of imbalance and when it might signal an underlying health issue.
Orthostatic hypotension—sometimes called postural hypotension—is a condition where blood pressure drops significantly upon standing. The body fails to adjust rapidly enough to maintain adequate blood flow to the brain, leading to symptoms like blurred vision, dizziness, weakness, or even fainting. In this article, we’ll explore the physiology behind this phenomenon, identify who is most at risk, and provide practical strategies to prevent or minimize its impact on daily life.
The Science Behind the Blur: How Blood Pressure Reacts to Gravity
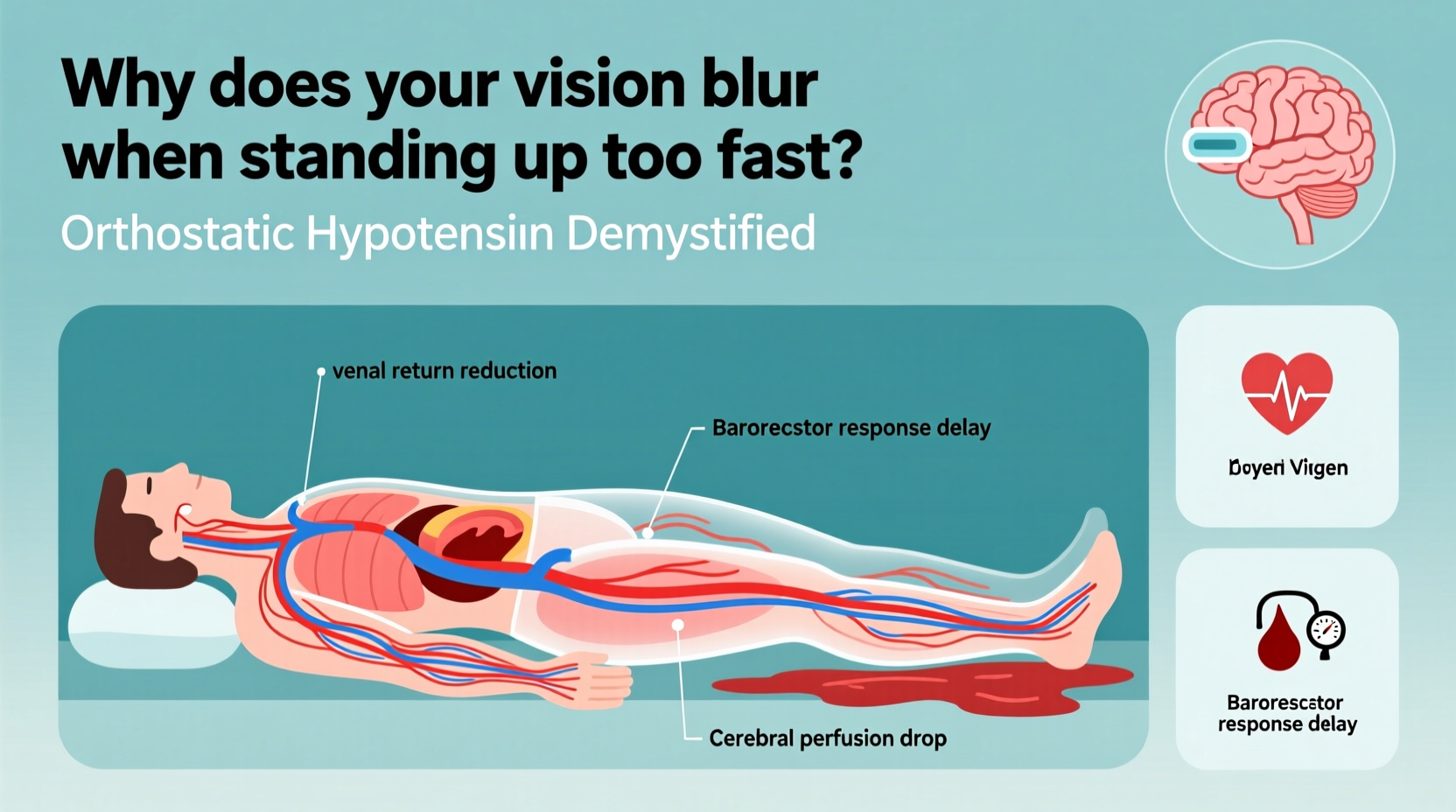
When you lie down, blood distributes relatively evenly throughout your body. But the moment you stand, gravity pulls blood downward into your legs and abdomen. Without immediate compensation, less blood returns to the heart, reducing cardiac output and, consequently, blood flow to the brain.
To counteract this, your autonomic nervous system kicks in within seconds. Baroreceptors—specialized sensors in the arteries of your neck and chest—detect the drop in pressure and send signals to your brainstem. In response, your nervous system triggers several adjustments:
- Narrowing of blood vessels (vasoconstriction) to increase resistance and raise pressure.
- A slight increase in heart rate to pump more blood per minute.
- Hormonal release (like norepinephrine) to support vascular tone.
These mechanisms normally work so efficiently that you don’t notice any change. However, if they are delayed, weakened, or impaired, blood pressure remains low long enough for symptoms to appear—most notably blurred vision, tunnel vision, or a sensation of “graying out.”
Who Is at Risk? Common Causes and Contributing Factors
While anyone can experience a momentary episode of orthostatic hypotension, certain individuals are more susceptible due to age, medical conditions, or medication use.
Age-Related Changes
As we age, the autonomic nervous system becomes less responsive. Blood vessels lose elasticity, and baroreceptor sensitivity declines. These changes make older adults—especially those over 65—more prone to postural drops in blood pressure.
Medications
Several classes of drugs can interfere with blood pressure regulation:
- Antihypertensives (blood pressure medications)
- Diuretics (increase fluid loss)
- Alpha-blockers (used for prostate issues or high blood pressure)
- Tricyclic antidepressants and antipsychotics
- Parkinson’s disease medications
Dehydration and Low Blood Volume
Inadequate fluid intake, excessive sweating, vomiting, or diarrhea reduce circulating blood volume. With less fluid to circulate, even normal gravitational shifts can lead to significant drops in pressure upon standing.
Underlying Medical Conditions
Certain chronic illnesses impair the body’s ability to regulate blood pressure:
- Diabetes: Can damage nerves involved in blood pressure control (autonomic neuropathy).
- Parkinson’s disease: Affects autonomic function and dopamine pathways tied to vascular tone.
- Heart conditions: Arrhythmias, heart failure, or valve disorders limit cardiac output.
- Adrenal insufficiency: Reduces production of hormones essential for blood pressure stability.
“Transient orthostatic hypotension is common and often benign, but recurrent or symptomatic episodes warrant evaluation—especially in older patients.” — Dr. Lena Patel, Neurologist and Autonomic Disorders Specialist
Symptoms and When to Seek Help
The hallmark symptom of orthostatic hypotension is dizziness or lightheadedness upon standing, typically lasting less than a few minutes. Other signs include:
- Blurred or dimmed vision
- Nausea
- Weakness or fatigue
- Confusion or difficulty concentrating
- Fainting (syncope)
Episodes usually resolve quickly once standing stops or you sit/lie back down. However, frequent or severe symptoms should not be ignored.
Red Flags That Warrant Medical Attention
Seek prompt evaluation if you experience:
- Fainting without warning
- Chest pain or palpitations during episodes
- Shortness of breath
- Symptoms lasting longer than 5 minutes
- Multiple falls related to dizziness
These could indicate serious cardiovascular, neurological, or metabolic issues requiring diagnosis and treatment.
Diagnosis: How Doctors Evaluate Orthostatic Hypotension
If symptoms persist, a healthcare provider may perform a simple test to confirm orthostatic hypotension. The standard protocol involves measuring blood pressure and heart rate in three positions:
- Lying down for 5 minutes
- Sitting for 1–2 minutes
- Standing, with readings taken at 1 and 3 minutes
A drop of at least 20 mm Hg in systolic pressure or 10 mm Hg in diastolic pressure within three minutes of standing confirms the condition.
In more complex cases, additional tests may be used:
- Tilt table test: Monitors responses while the body is tilted upright.
- Autonomic function testing: Assesses nerve control over heart rate and blood pressure.
- Blood tests: To check for anemia, electrolyte imbalances, or hormonal deficiencies.
Do’s and Don’ts When Managing Symptoms
| Do’s | Don’ts |
|---|---|
| Rise slowly from bed or chair | Stand up abruptly after lying down |
| Stay well-hydrated (especially in heat) | Skip meals or restrict fluids excessively |
| Perform leg muscle contractions before standing | Stand still for long periods |
| Review medications with your doctor | Stop prescribed meds without consultation |
| Wear compression stockings if advised | Ignore recurrent dizziness or falls |
Practical Strategies to Prevent Episodes
You don’t have to live with frequent dizzy spells. Simple lifestyle adjustments can dramatically reduce the frequency and severity of orthostatic hypotension.
Step-by-Step Guide to Safer Standing
- Pause before rising: After waking or sitting, sit on the edge of the bed or chair for 30–60 seconds.
- Engage leg muscles: Flex your calves, squeeze your thighs, or march in place to push blood upward.
- Stand slowly: Use your arms to assist and avoid locking your knees.
- Hold onto support: Grab a wall, counter, or furniture until you feel stable.
- Breathe steadily: Avoid holding your breath, which can further lower blood pressure.
Hydration and Diet Tips
Maintaining blood volume is key. Aim for 6–8 glasses of water daily unless restricted by a medical condition. Some people benefit from slightly increasing salt intake under medical supervision, as sodium helps retain fluid and boost blood pressure.
Smaller, more frequent meals can also help. Large meals divert blood to the digestive tract, potentially worsening postural drops—a phenomenon known as *postprandial hypotension*.
Physical Counterpressure Maneuvers
For those prone to sudden symptoms, certain techniques can instantly raise blood pressure:
- Cross your legs and tense your thigh muscles.
- Squeeze a rubber ball or clench your fists.
- Bend forward slightly at the waist (e.g., leaning over a shopping cart).
These actions compress blood vessels and increase venous return, helping sustain cerebral perfusion.
Real-Life Example: Managing Daily Challenges
Consider Maria, a 72-year-old retired teacher managing type 2 diabetes and hypertension. She began noticing frequent dizziness when getting out of bed, sometimes accompanied by tunnel vision. One morning, she nearly fell while walking to the bathroom.
After visiting her primary care physician, Maria was diagnosed with orthostatic hypotension. Her medications were reviewed—she was taking a diuretic and an ACE inhibitor, both of which can lower blood pressure. Her doctor adjusted her dosing schedule, recommending the diuretic be taken earlier in the day and advising against rapid position changes.
Maria also started doing leg exercises before standing, increased her fluid intake, and began wearing mid-thigh compression stockings. Within two weeks, her symptoms improved significantly. She now uses a raised toilet seat and keeps a nightlight on to safely navigate at night.
Her case illustrates how a combination of medication review, lifestyle changes, and awareness can restore confidence and safety.
FAQ: Common Questions About Orthostatic Hypotension
Is it dangerous to black out for a few seconds when standing?
Occasional brief lightheadedness is usually not dangerous. However, repeated or prolonged episodes increase fall risk, especially in older adults. If you lose consciousness, even briefly, consult a healthcare provider to rule out cardiac or neurological causes.
Can young people get orthostatic hypotension?
Yes. While more common in older adults, younger individuals—especially those with dehydration, eating disorders, or conditions like POTS (Postural Orthostatic Tachycardia Syndrome)—can experience similar symptoms. Athletes or those recovering from illness may also be temporarily affected.
Does caffeine help or hurt?
Caffeine can cause a short-term rise in blood pressure and may offer mild protection against orthostatic drops. However, its diuretic effect can contribute to dehydration over time. Moderation is key—especially for sensitive individuals.
Conclusion: Take Control of Your Stability
Blurred vision when standing up too fast isn't something you must simply accept as part of aging or daily life. Understanding orthostatic hypotension empowers you to take proactive steps—whether it’s adjusting how you rise from bed, staying hydrated, or reviewing medications with your doctor. Small changes can yield significant improvements in balance, safety, and overall well-being.
If symptoms persist or interfere with your routine, don’t hesitate to seek medical advice. Early intervention can prevent complications like falls, fractures, or reduced quality of life. Your body is designed to adapt—but sometimes, it just needs a little help keeping pace.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?