Suddenly standing from a seated or lying position and experiencing blurred vision, dizziness, or even momentary blackouts is a surprisingly common experience. While often fleeting and harmless, it can be unsettling—and sometimes, a signal of an underlying health issue. This phenomenon, known medically as orthostatic hypotension, occurs when blood pressure drops rapidly upon standing. Understanding why this happens, what factors contribute to it, and when it’s time to consult a healthcare provider can help you respond appropriately and maintain long-term cardiovascular health.
The Science Behind Blurred Vision Upon Standing
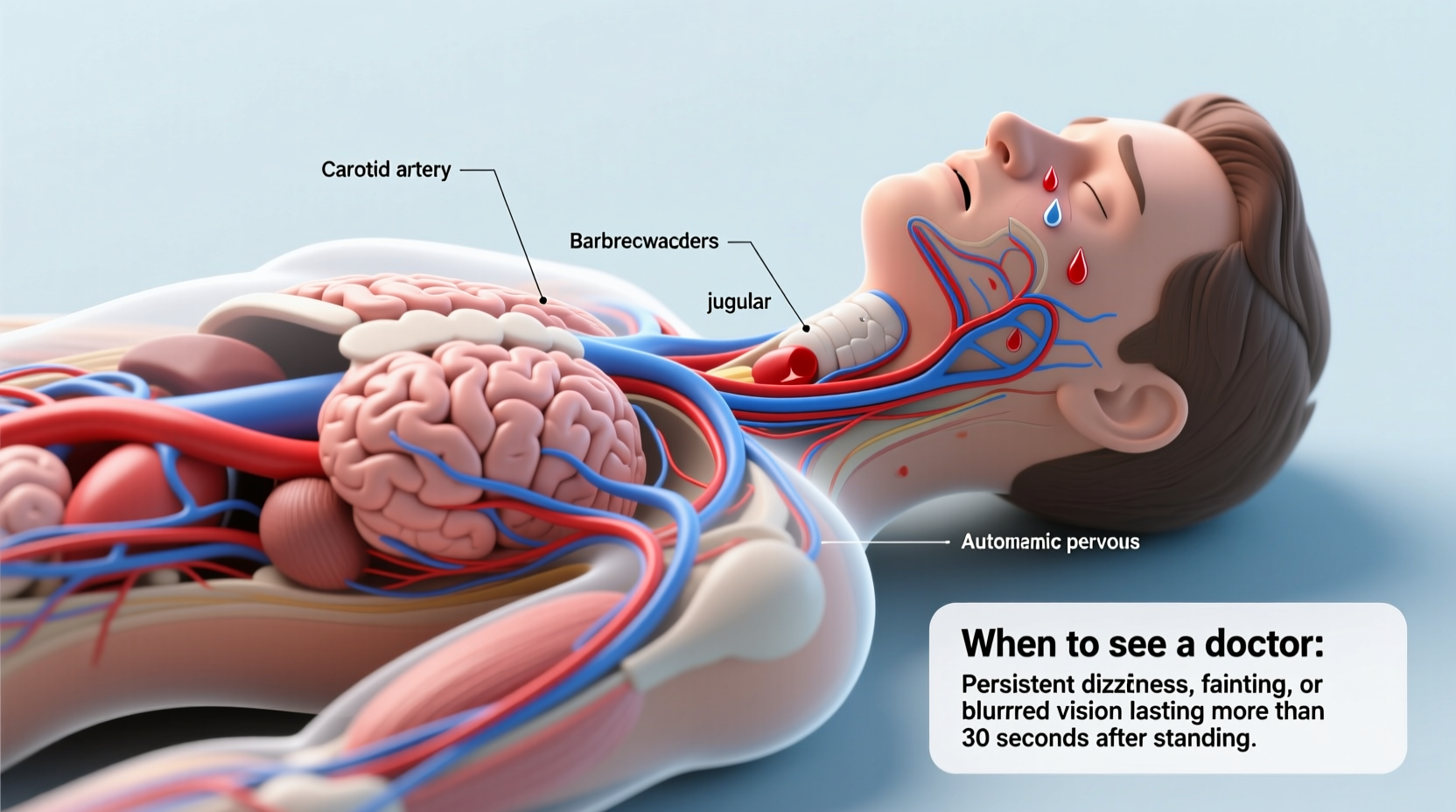
When you transition from sitting or lying down to standing, gravity pulls blood downward into your legs and abdomen. In response, your body must quickly adjust to ensure consistent blood flow to the brain. This process involves several coordinated systems: the autonomic nervous system, heart rate regulation, and vascular tone. Under normal conditions, blood vessels constrict and heart rate increases slightly to maintain adequate cerebral perfusion—blood supply to the brain.
However, if this regulatory mechanism lags or fails—even briefly—the brain receives less oxygen-rich blood than needed. This temporary ischemia (reduced blood flow) affects visual processing centers in the occipital lobe, leading to symptoms like:
- Blurred or tunnel vision
- Dizziness or lightheadedness
- Nausea or weakness
- Seeing \"stars\" or flashes
- Ringing in the ears (tinnitus)
- In severe cases, fainting (syncope)
This transient drop in blood pressure is called orthostatic hypotension. The American Heart Association defines it as a decrease of at least 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic pressure within three minutes of standing.
Common Causes of Orthostatic Hypotension
While occasional episodes are usually benign, frequent or worsening symptoms may point to identifiable causes. These range from lifestyle factors to medical conditions and medications.
Dehydration
Insufficient fluid intake reduces blood volume, making it harder for the body to maintain pressure when upright. This is especially common in hot environments, during illness with vomiting or diarrhea, or after intense exercise without proper rehydration.
Medications
Several classes of drugs can interfere with blood pressure regulation:
- Blood pressure medications (e.g., beta-blockers, ACE inhibitors)
- Diuretics (\"water pills\")
- Antidepressants (especially tricyclics)
- Parkinson’s disease medications
- Some erectile dysfunction drugs
Age-Related Changes
As people age, baroreceptor sensitivity (the body’s ability to detect and respond to blood pressure changes) diminishes. Vascular stiffness and slower autonomic responses increase susceptibility to orthostatic drops. It's estimated that up to 30% of adults over 70 experience some degree of orthostatic hypotension.
Underlying Medical Conditions
Certain chronic diseases disrupt the autonomic nervous system or reduce blood volume:
- Diabetes (can cause autonomic neuropathy)
- Parkinson’s disease and other neurodegenerative disorders
- Heart conditions (arrhythmias, valve problems, heart failure)
- Anemia (reduced oxygen-carrying capacity of blood)
- Adrenal insufficiency (e.g., Addison’s disease)
Postprandial Hypotension
Some individuals experience significant drops in blood pressure within 30–75 minutes after eating, particularly large carbohydrate-rich meals. Blood diverts to the digestive tract, reducing availability for the brain. This condition is more common in older adults and those with Parkinson’s.
“Orthostatic hypotension isn’t just a nuisance—it can be an early warning sign of autonomic dysfunction or cardiovascular risk.” — Dr. Lisa Nguyen, Neurologist and Autonomic Specialist
When Should You See a Doctor?
Occasional mild dizziness upon standing, especially after dehydration or prolonged bed rest, typically doesn’t require medical evaluation. However, certain red flags indicate the need for prompt assessment by a healthcare professional.
Warning Signs That Warrant Medical Attention
| Symptom | Frequency/Context | Potential Concern |
|---|---|---|
| Fainting (syncope) | More than once | Cardiac arrhythmia, neurological disorder |
| Confusion or slurred speech | During or after episode | Stroke risk, severe hypoperfusion |
| Chest pain or palpitations | Accompanying dizziness | Heart-related cause |
| Progressive frequency | Increasing over weeks/months | Neurodegenerative disease |
| Leg numbness or weakness | With positional changes | Spinal cord or nerve compression |
If you're over 65, managing chronic illness, or taking multiple medications, even recurrent mild symptoms should be discussed with your physician. Persistent orthostatic hypotension increases fall risk and may contribute to cognitive decline over time due to repeated micro-ischemic events in the brain.
Diagnostic Process and What to Expect
If you visit a doctor for recurrent episodes, expect a thorough evaluation focused on identifying reversible causes and ruling out serious conditions.
Step-by-Step Diagnostic Timeline
- Medical History Review: Your doctor will ask about symptom frequency, timing, associated factors (e.g., meals, medications), and pre-existing conditions.
- Orthostatic Vital Signs: Blood pressure and heart rate are measured while lying down, then again after one and three minutes of standing.
- Physical Examination: Focus on heart, neurological function, and signs of dehydration or neuropathy.
- Laboratory Tests: CBC (for anemia), electrolytes, glucose, kidney function, cortisol levels if adrenal issues are suspected.
- Electrocardiogram (ECG): To check for arrhythmias or structural heart problems.
- Advanced Testing (if indicated): Tilt table test, autonomic function testing, or Holter monitor for intermittent rhythm disturbances.
A tilt table test, considered the gold standard for diagnosing neurogenic orthostatic hypotension, involves securing the patient to a table that tilts from horizontal to near-vertical while continuously monitoring blood pressure and heart rate.
Practical Tips and Prevention Strategies
Even if no serious condition is found, proactive measures can significantly reduce the frequency and severity of symptoms.
Everyday Adjustments to Reduce Risk
- Stay hydrated: Aim for 6–8 glasses of water daily; more in heat or during illness.
- Rise slowly: Use a two-step transition—sit first, then stand.
- Flex leg muscles before standing: Pump your calves or cross your legs to push blood upward.
- Avoid large meals: Opt for smaller, more frequent meals to prevent postprandial drops.
- Limit alcohol: Alcohol dilates blood vessels and worsens orthostatic effects.
- Wear compression stockings: These help prevent blood pooling in the legs.
Checklist: Managing Orthostatic Symptoms at Home
- ✅ Measure blood pressure at home in lying and standing positions
- ✅ Review all medications with your doctor annually
- ✅ Monitor hydration—urine should be pale yellow
- ✅ Avoid standing still for long periods
- ✅ Sleep with head elevated 6–10 inches if nighttime urination contributes to morning symptoms
- ✅ Keep a symptom diary noting triggers, duration, and severity
Real-Life Example: Recognizing a Hidden Condition
John, a 68-year-old retiree, began noticing increasing dizziness when getting out of bed. Initially dismissing it as aging, he eventually fainted while paying bills at a standing kiosk. After an ER visit ruled out cardiac events, his primary care physician conducted orthostatic testing and discovered a 30-point drop in systolic pressure upon standing. Further investigation revealed autonomic neuropathy linked to undiagnosed type 2 diabetes. With improved glucose control, medication adjustment, and lifestyle changes—including increased fluid and salt intake—his symptoms resolved within months.
This case illustrates how seemingly minor symptoms can mask significant underlying conditions. Early recognition prevented potential falls and allowed timely management of a chronic disease.
Frequently Asked Questions
Is it normal to see spots when standing up quickly?
Yes, seeing brief “spots” or “stars” is common and usually results from transient reduced blood flow to the visual cortex. If infrequent and short-lived, it’s typically not concerning. However, regular occurrences warrant evaluation.
Can anxiety cause blurred vision when standing?
Anxiety itself doesn’t directly cause orthostatic hypotension, but hyperventilation during anxious episodes can lower carbon dioxide levels in the blood, leading to vasoconstriction and dizziness. Anxiety may also amplify awareness of normal physiological sensations.
Are children affected by this condition?
Orthostatic hypotension is less common in healthy children but can occur during growth spurts, dehydration, or in those with chronic fatigue syndrome (e.g., POTS—Postural Orthostatic Tachycardia Syndrome). Pediatric cases require specialized evaluation.
Conclusion: Listen to Your Body
Blurred vision upon standing is more than just a fleeting inconvenience—it’s a physiological signal worth understanding. While often benign, recurring or worsening symptoms should never be ignored. By recognizing patterns, adjusting habits, and seeking medical advice when necessary, you protect not only your balance but your overall cardiovascular and neurological health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?