Colorectal cancer is one of the most preventable forms of cancer — yet it remains the third leading cause of cancer-related deaths in the United States. The reason? Too many people delay or avoid screening. A colonoscopy is the gold standard for detecting and preventing colon cancer, but many remain uncertain about why it's necessary, what the procedure involves, and what to expect before, during, and after. Understanding this critical screening tool empowers individuals to take control of their digestive health and significantly reduce their risk of developing advanced disease.
Why Get a Colonoscopy: Key Reasons
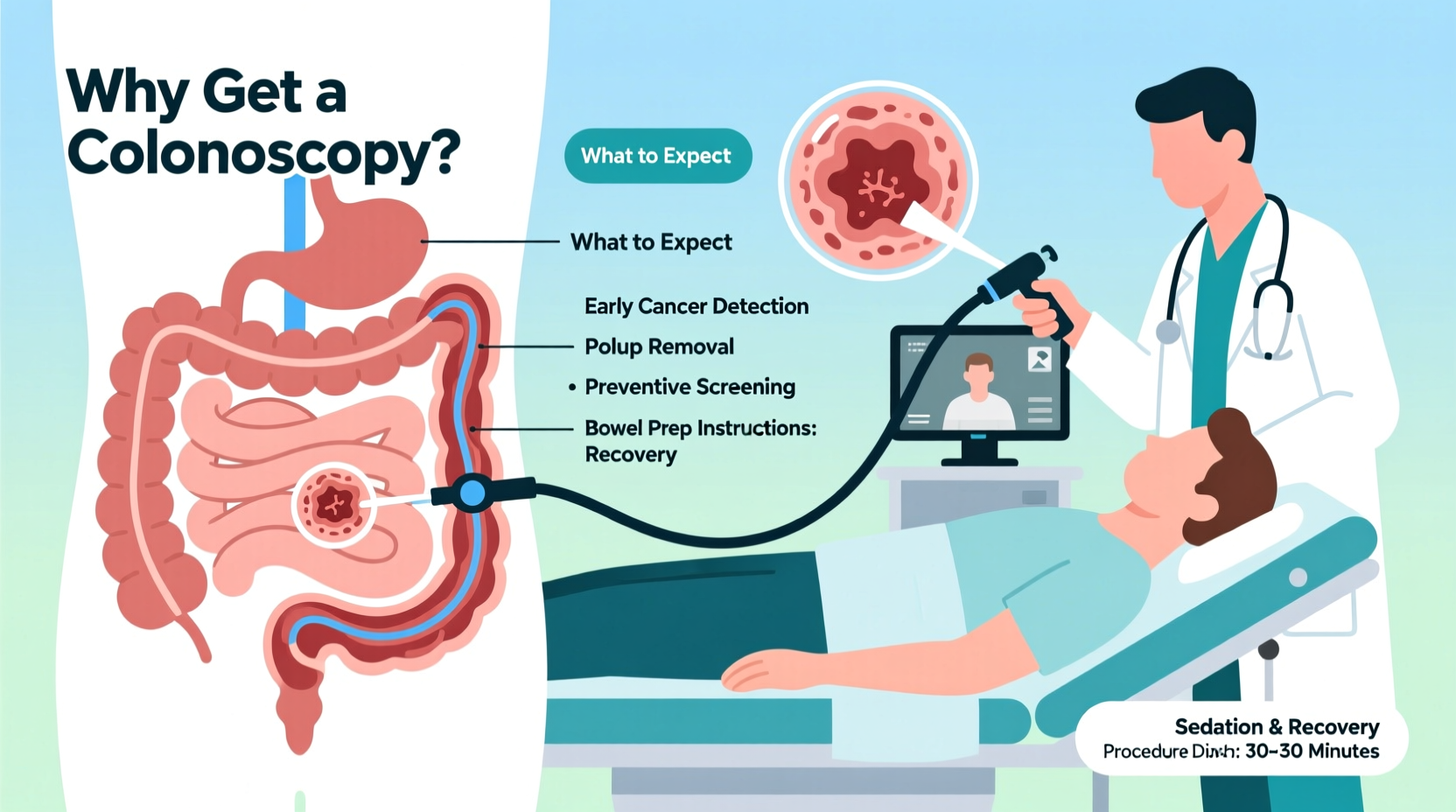
A colonoscopy isn't just a diagnostic test — it's a powerful preventive measure. Unlike other screenings that only detect abnormalities, a colonoscopy allows physicians to identify and remove precancerous growths before they turn into cancer.
- Cancer prevention: Polyps — small growths on the colon lining — can develop into cancer over time. Removing them during a colonoscopy stops cancer before it starts.
- Early detection: If cancer is present, catching it early dramatically improves survival rates. The five-year survival rate for localized colon cancer is over 90%.
- Evaluation of symptoms: Unexplained abdominal pain, chronic diarrhea, rectal bleeding, or unexplained weight loss may indicate underlying issues that a colonoscopy can help diagnose.
- Monitoring high-risk conditions: Individuals with inflammatory bowel disease (IBD), a family history of colon cancer, or certain genetic syndromes require regular surveillance.
- Baseline screening: Even without symptoms, guidelines recommend starting screening at age 45 for average-risk adults.
“Colonoscopy is unique among cancer screening tools because it both detects and prevents cancer. That dual capability makes it indispensable.” — Dr. Linda Chen, Gastroenterologist and Colorectal Cancer Prevention Specialist
What Happens During a Colonoscopy: Step-by-Step Procedure
The colonoscopy itself typically takes 30 to 60 minutes and is performed on an outpatient basis. Here’s what occurs from arrival to recovery:
- Check-in and prep verification: You’ll arrive at the endoscopy center, where staff will review your medical history, confirm your bowel prep completion, and start an IV line for sedation.
- Sedation administration: Most patients receive moderate sedation (often called “conscious sedation”) or propofol for deeper relaxation. You’ll likely sleep through the procedure.
- Positioning: You’ll lie on your left side with knees drawn toward your chest to allow easier access.
- Scope insertion: The doctor gently inserts a thin, flexible tube called a colonoscope through the rectum and advances it slowly through the entire colon.
- Examination and imaging: A tiny camera on the scope transmits real-time video to a monitor, allowing the physician to inspect the intestinal lining for inflammation, ulcers, polyps, or tumors.
- Polyp removal or biopsy: If any polyps are found, they are removed using specialized tools passed through the scope. Tissue samples (biopsies) may also be taken.
- Withdrawal: As the scope is carefully withdrawn, the physician re-examines the colon lining for missed areas.
- Recovery: After the procedure, you’re moved to a recovery area. Most people wake up within 30–60 minutes, though grogginess can last several hours due to sedation.
You will not be allowed to drive yourself home, so arranging transportation is essential. Most patients resume normal activities the following day.
Bowel Preparation: What You Need to Do Beforehand
The success of a colonoscopy depends heavily on how well your colon is cleaned out. Poor prep can lead to missed polyps and may require repeating the procedure.
Preparation usually begins 1–2 days before the exam and includes:
- Switching to a clear liquid diet (broth, apple juice, gelatin, tea — no red or purple liquids)
- Consuming a prescribed laxative solution (such as GoLYTELY, MiraLAX + Gatorade, or Sutab)
- Drinking large volumes of fluid (often 1–2 gallons) over several hours
- Avoiding solid foods, dairy, seeds, nuts, and high-fiber items for 2–3 days prior
| Do’s | Don’ts |
|---|---|
| Start prep exactly as instructed | Ignore prep instructions thinking “I know better” |
| Stay near a bathroom — expect frequent, watery bowel movements | Eat solid food the day before |
| Use wet wipes or barrier cream to prevent skin irritation | Drink red, purple, or opaque liquids |
| Continue essential medications unless told otherwise | Take blood thinners or diabetes meds without consulting your doctor |
Real Experience: A Patient’s First Colonoscopy
James, a 52-year-old teacher with no symptoms, avoided his first colonoscopy for years due to fear of discomfort and embarrassment. Encouraged by his wife and primary care provider, he finally scheduled the procedure after turning 50.
He followed the prep instructions closely, drinking the entire solution the night before. Though uncomfortable, he managed nausea with slow sipping and light music. During the colonoscopy, he was fully asleep. Upon waking, his doctor informed him that three small polyps had been removed — all benign, but potentially dangerous if left untreated.
“I wish I hadn’t waited,” James said later. “The prep was the worst part, and even that wasn’t as bad as I imagined. Knowing I stopped something serious from happening is worth every minute.”
His experience underscores a common truth: anxiety about colonoscopy is often worse than the actual process.
Frequently Asked Questions
Is a colonoscopy painful?
Most patients feel little to no pain due to sedation. Some report mild cramping or bloating afterward from air introduced during the exam, but this usually resolves within a few hours.
How often do I need a colonoscopy?
For average-risk individuals with a normal result, the next screening is typically recommended in 10 years. If polyps are found, follow-up may be needed in 3–5 years, depending on size, number, and type.
Are there alternatives to colonoscopy?
Yes, but they have limitations. Options include stool-based tests (like FIT or Cologuard) and virtual colonoscopy (CT scan). However, these cannot remove polyps. A positive result usually requires a follow-up colonoscopy anyway.
Action Plan: Your Colonoscopy Checklist
Preparing for your colonoscopy doesn’t have to be overwhelming. Use this checklist to stay on track:
- 📅 Schedule your appointment with a board-certified gastroenterologist.
- 📄 Review prep instructions and mark key times on your calendar.
- 🛒 Purchase supplies: laxative kit, electrolyte drinks, soft toilet paper, barrier cream.
- 🍎 Adjust your diet 3 days prior: avoid seeds, skins, raw vegetables, and tough meats.
- 🚽 Clear your schedule the day before and the day of — plan to stay home.
- 🚗 Arrange for a responsible adult to drive you home.
- 💊 Confirm which medications to stop or continue with your doctor (especially blood thinners).
- 😴 Rest after the procedure — avoid operating machinery for 24 hours.
Final Thoughts: Take Control of Your Health
A colonoscopy is more than a medical test — it’s an act of self-care with long-term benefits. With rising rates of colorectal cancer in younger adults, putting off screening is a growing risk. The procedure is safe, effective, and often life-saving. While the preparation may seem daunting, millions of people complete it every year with minimal discomfort and maximum peace of mind.
If you're due for a screening — whether you're 45 or 75 — don’t let fear or misinformation stand in your way. Talk to your doctor, ask questions, and take the next step. Preventing cancer is always better than treating it.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?