A spinal tap, also known as a lumbar puncture, is a medical procedure used to collect cerebrospinal fluid (CSF) from the lower back. While the idea may sound intimidating, it’s a routine diagnostic tool that helps physicians detect serious conditions affecting the brain and spinal cord. Understanding why it’s done, how it works, and what to expect can ease anxiety and help patients prepare with confidence.
Why Is a Spinal Tap Performed?
The primary purpose of a spinal tap is to analyze cerebrospinal fluid, a clear liquid that cushions the brain and spinal cord. Changes in its composition—such as protein levels, white blood cell count, or the presence of infectious agents—can signal neurological disorders.
Common reasons for performing a spinal tap include:
- Diagnosing infections: Meningitis, encephalitis, or syphilis can be confirmed by detecting bacteria, viruses, or abnormal immune markers in CSF.
- Evaluating multiple sclerosis (MS): Oligoclonal bands in CSF are a key biomarker for MS.
- Detecting subarachnoid hemorrhage: When a brain bleed doesn’t show clearly on imaging, CSF analysis can reveal red blood cells.
- Investigating dementia or neurodegenerative diseases: Certain proteins like tau or amyloid-beta may indicate Alzheimer’s disease.
- Monitoring cancer: Leptomeningeal carcinomatosis (cancer spread to the nervous system lining) can be diagnosed via CSF cytology.
- Administering medication or anesthesia: In rare cases, chemotherapy or spinal anesthesia is delivered directly into the CSF.
“Lumbar puncture remains one of the most direct ways to assess central nervous system health when imaging alone isn’t enough.” — Dr. Alan Reyes, Neurologist, Massachusetts General Hospital
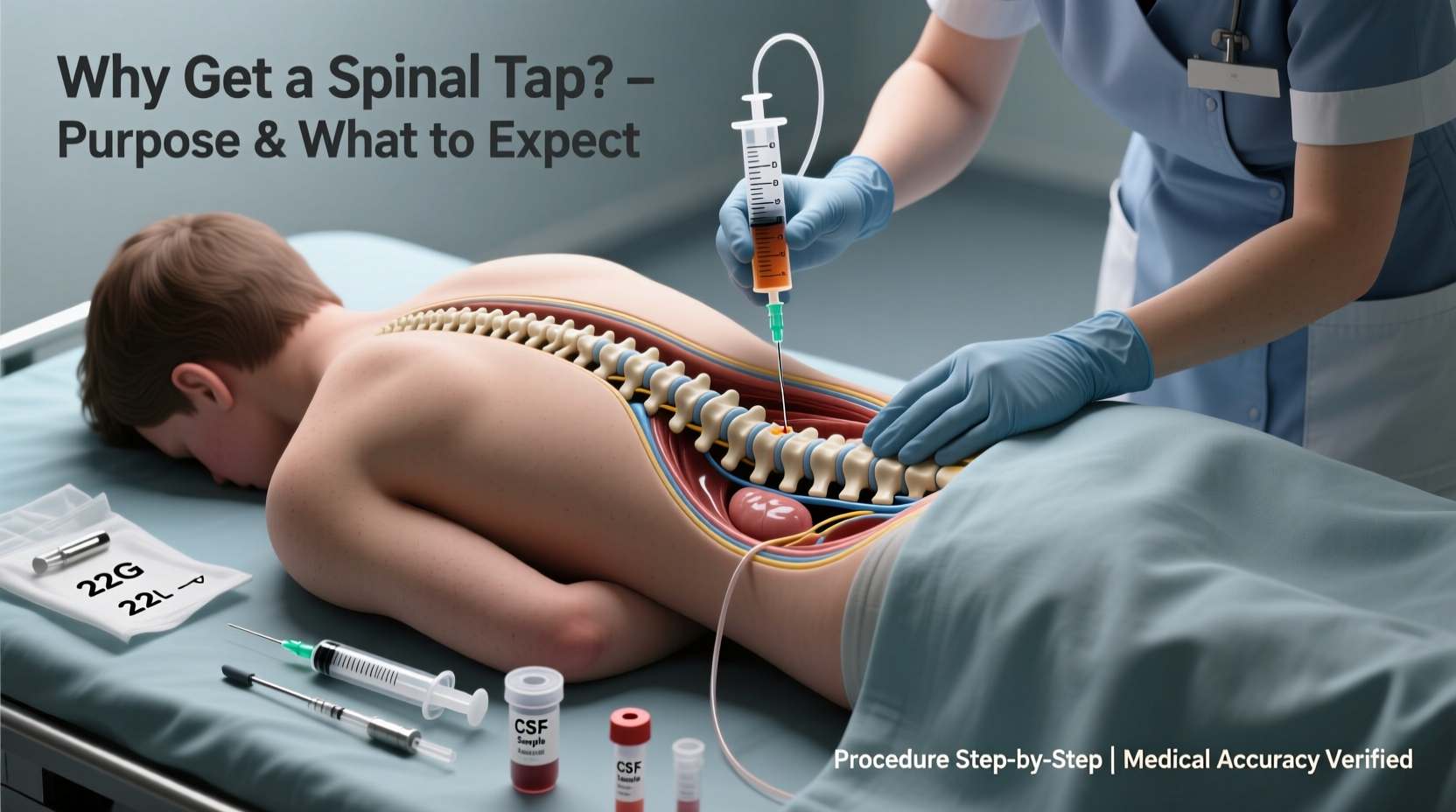
How the Procedure Works: Step-by-Step
A spinal tap is typically performed in a hospital, clinic, or outpatient setting and takes about 30 to 45 minutes. Here’s what happens:
- Patient positioning: You’ll lie on your side with knees drawn up to your chest, or sit bent forward. This opens the spaces between the vertebrae in the lower back.
- Cleaning and numbing: The skin over the lower spine is cleaned with antiseptic. A local anesthetic is injected to numb the area, which may cause a brief stinging sensation.
- Insertion of the needle: Using sterile technique, a thin, hollow needle is inserted between two lumbar vertebrae (usually L3-L4 or L4-L5), avoiding the spinal cord itself.
- Fluid collection: CSF drips into collection tubes—typically 2 to 10 milliliters are gathered. Pressure may be measured using a manometer.
- Needle removal and dressing: Once enough fluid is collected, the needle is removed, and a small bandage is applied.
What to Expect Before and After the Procedure
Preparation and recovery are crucial parts of the experience. Knowing what lies ahead can significantly reduce stress.
Before the Spinal Tap
- You may be asked to stop blood-thinning medications (like aspirin or warfarin) a few days prior, if safe.
- Fasting is usually not required unless sedation is planned.
- Inform your doctor if you have a history of bleeding disorders, back surgery, or increased intracranial pressure.
- An MRI or CT scan might be ordered first to rule out brain swelling that could make the procedure risky.
During Recovery
After the procedure:
- You’ll be asked to lie flat for 1 to 2 hours to reduce the risk of headache.
- Hydration is encouraged—drinking water or sports drinks helps replenish fluids and may prevent post-lumbar puncture headaches.
- Mild soreness at the injection site is common and usually resolves within a few days.
- Avoid strenuous activity, heavy lifting, or bending over for 24–48 hours.
Common Risks and Side Effects
While generally safe, spinal taps carry some risks. Most side effects are mild and temporary.
| Side Effect | Likelihood | Management |
|---|---|---|
| Post-dural puncture headache | Up to 30% | Bed rest, hydration, caffeine, or epidural blood patch if severe |
| Back pain or tenderness | Common | Over-the-counter pain relievers (e.g., acetaminophen) |
| Nausea or dizziness | Occasional | Rest and slow position changes |
| Infection or bleeding | Rare | Requires immediate medical attention |
| Nerve irritation | Very rare | Temporary tingling or shooting pain; resolves on its own |
Real-World Example: Diagnosing Suspected Meningitis
Sarah, a 24-year-old graduate student, arrived at the emergency room with a high fever, stiff neck, and sensitivity to light. A CT scan showed no structural abnormalities, but meningitis was suspected. Doctors performed a spinal tap, and the CSF analysis revealed elevated white blood cells, low glucose, and high protein—classic signs of bacterial meningitis. Prompt antibiotic treatment was started, and Sarah recovered fully within a week. Without the spinal tap, the diagnosis could have been delayed, risking severe complications.
This case illustrates how critical timely CSF analysis can be in life-threatening conditions.
Preparing for Your Spinal Tap: A Checklist
To ensure a smooth experience, use this checklist:
- ✅ Discuss all medications with your doctor, especially blood thinners.
- ✅ Arrange for someone to drive you home afterward.
- ✅ Wear comfortable, loose-fitting clothing.
- ✅ Ask questions—understand the risks, benefits, and alternatives.
- ✅ Stay hydrated before and after the procedure.
- ✅ Plan to rest for the remainder of the day.
Frequently Asked Questions
Does a spinal tap hurt?
Most people feel pressure rather than sharp pain. The area is numbed with a local anesthetic, so while you may feel a pinch from the numbing shot and some pressure during needle insertion, severe pain is uncommon. Many report it being less uncomfortable than expected.
How long does it take to get results?
Preliminary results (like cell count or appearance) may be available within hours. More detailed tests—such as cultures, protein electrophoresis, or PCR for viruses—can take 24 to 72 hours. Complex autoimmune or genetic panels may require several days.
Can I refuse a spinal tap?
Yes, you have the right to informed refusal. However, your doctor will explain why the test is recommended and what alternative diagnostic options exist. In emergencies like suspected meningitis, delaying the procedure can be dangerous.
Final Thoughts: Knowledge Empowers Confidence
Understanding the purpose, process, and expectations surrounding a spinal tap transforms fear into preparedness. This procedure, though invasive, provides invaluable insights that imaging alone cannot offer. Whether ruling out infection, diagnosing MS, or monitoring neurological health, the data gathered from cerebrospinal fluid can guide life-changing treatments.
If your doctor recommends a lumbar puncture, ask questions, follow pre-procedure advice, and trust the medical team’s expertise. With proper care and realistic expectations, most patients tolerate the procedure well and walk away with answers that matter.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?