Cardiac catheterization—commonly referred to as a \"heart cath\"—is a vital diagnostic and sometimes therapeutic procedure used to evaluate heart function and identify cardiovascular issues. It provides doctors with detailed information about blood flow, pressure within the heart chambers, and the condition of coronary arteries. While the idea of a heart cath may sound intimidating, it’s a routine, minimally invasive test that plays a crucial role in managing heart disease.
Understanding why it's performed, how the procedure works, and what you can expect can ease anxiety and help you prepare effectively. Whether you or a loved one has been recommended for a heart cath, this guide breaks down everything you need to know in clear, practical terms.
Why Is a Heart Cath Done? Common Reasons
A heart catheterization serves both diagnostic and interventional purposes. It allows cardiologists to directly assess the heart’s anatomy and function, often when non-invasive tests like stress tests or echocardiograms are inconclusive or suggest significant disease.
Primary reasons include:
- Evaluating chest pain or suspected coronary artery disease (CAD): To check for blockages in the coronary arteries that could restrict blood flow and lead to angina or heart attacks.
- Measuring pressures inside the heart: Helps diagnose conditions like heart failure, pulmonary hypertension, or valvular disease.
- Assessing heart muscle function: The procedure can reveal how well the heart pumps blood (ejection fraction).
- Diagnosing congenital heart defects: Especially in adults with known or suspected structural heart problems present since birth.
- Guiding treatment decisions: Results from a heart cath help determine whether medications, angioplasty, stenting, or bypass surgery are needed.
- Post-heart attack evaluation: Often performed soon after a heart attack to identify blocked arteries and potentially open them immediately.
“Cardiac catheterization remains the gold standard for diagnosing coronary artery disease. No other test gives us such precise images of the coronary vessels.” — Dr. Alan Reyes, Interventional Cardiologist, Cleveland Clinic
How the Procedure Works: Step-by-Step Timeline
A heart cath typically takes 30 to 60 minutes, though preparation and recovery extend the total time spent at the hospital. Here’s what happens during each phase:
- Pre-Procedure Preparation (1–2 hours): You’ll change into a hospital gown, have an IV line placed, and your vital signs monitored. Blood tests and an ECG may be repeated. You’ll sign a consent form and discuss allergies, especially to contrast dye.
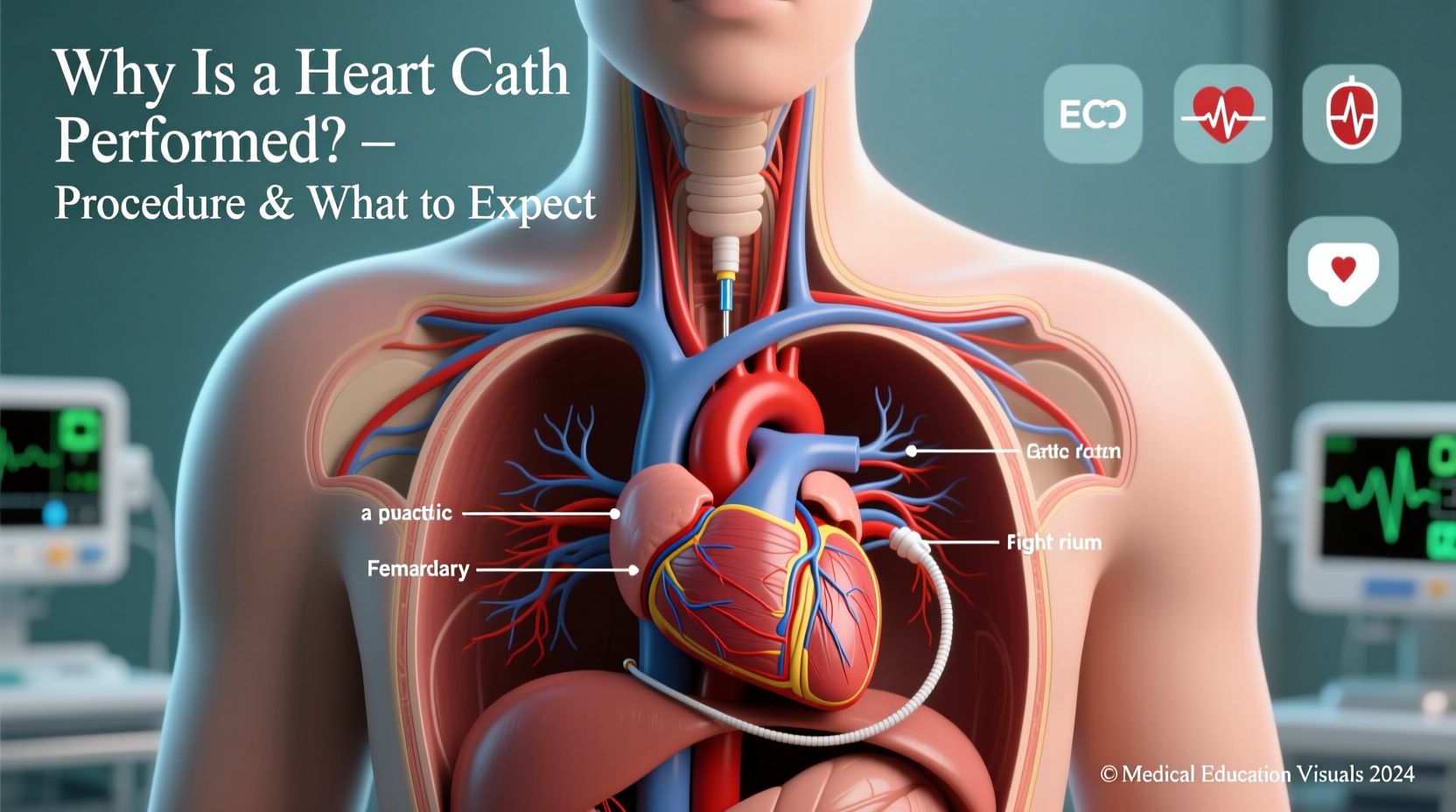
- Access Site Prep: The insertion site—usually the wrist (radial artery) or groin (femoral artery)—is cleaned and numbed with local anesthesia.
- Catheter Insertion: A thin, flexible tube (catheter) is threaded through the artery toward the heart under X-ray guidance.
- Contrast Injection & Imaging: Once the catheter reaches the heart, contrast dye is injected into the coronary arteries. Special X-ray images (angiograms) capture real-time blood flow, revealing any narrowing or blockages.
- Pressure Measurements: The catheter measures pressure in the heart chambers and evaluates valve function.
- Possible Intervention: If a significant blockage is found, the team may perform angioplasty and place a stent during the same session.
- Catheter Removal: After imaging, the catheter is removed. Pressure is applied to the site or a closure device used to prevent bleeding.
What to Expect Before, During, and After
Before the Procedure
You’ll receive specific instructions, but generally:
- Fasting for 6–8 hours beforehand is required.
- Inform your doctor about all medications, especially blood thinners like warfarin or clopidogrel.
- Blood tests (including kidney function) are checked due to the use of contrast dye.
- Arrange for someone to drive you home—sedation may be used, even if it’s mild.
During the Procedure
You’ll be awake but relaxed. Sedatives may be given to reduce anxiety. You might feel:
- A brief sting from the local anesthetic.
- Warmth or flushing when contrast dye is injected—this is normal and lasts only seconds.
- Pressure at the insertion site, but not sharp pain.
The medical team will communicate throughout, asking you to hold your breath or stay still during imaging.
After the Procedure
Recovery depends on the access site:
- Radial (wrist): You can usually sit up within 1–2 hours and go home the same day.
- Femoral (groin): Requires lying flat for 2–6 hours to prevent bleeding. Same-day discharge is common unless intervention was performed.
Common after-effects include mild soreness at the insertion site and possible bruising. Drink plenty of fluids to flush out the contrast dye.
Do’s and Don’ts After a Heart Cath
| Do’s | Don’ts |
|---|---|
| Keep the insertion site clean and dry for 24–48 hours. | Don’t lift heavy objects (>10 lbs) for 2–3 days. |
| Monitor the site for swelling, redness, or bleeding. | Don’t submerge the site in water (no baths, swimming). |
| Take prescribed medications as directed, including antiplatelets if a stent was placed. | Don’t drive until cleared by your doctor (usually 24 hours). |
| Resume light activities gradually. | Don’t ignore chest pain, shortness of breath, or signs of infection. |
Real-World Example: A Patient’s Experience
John, a 58-year-old teacher, had been experiencing chest tightness during his morning walks. His stress test showed possible ischemia, so his cardiologist recommended a heart cath. He was anxious but learned the procedure would be done via the radial artery.
On the day of the procedure, John fasted as instructed and arrived early. The team explained each step. He felt a warm flush when the dye was injected but no pain. The test revealed a 70% blockage in one artery. The cardiologist performed angioplasty and placed a stent immediately.
Within two hours, John was sitting up, eating, and talking to his family. He went home the same afternoon with prescriptions and follow-up instructions. Within a week, he was walking again—chest pain-free.
Frequently Asked Questions
Is a heart cath dangerous?
While all medical procedures carry some risk, heart catheterization is generally safe. Complication rates are low (under 1%). Potential risks include bleeding at the insertion site, allergic reaction to contrast dye, kidney injury (especially in those with pre-existing kidney disease), or rare events like stroke or heart attack. Your medical team will assess your individual risk beforehand.
Will I be asleep during the procedure?
Most patients are awake but given mild sedation to help them relax. General anesthesia is not used. You’ll be able to follow instructions, such as holding your breath, which helps obtain clear images.
How long does recovery take?
For uncomplicated diagnostic caths, most people return to light activities within 24 hours and full activity in a few days. If a stent was placed, your doctor may recommend avoiding strenuous exercise for about a week and prescribe medications like aspirin and clopidogrel to prevent clots.
Final Thoughts: Taking Control of Your Heart Health
A heart cath is more than just a diagnostic tool—it’s a gateway to understanding and treating heart disease effectively. Whether confirming a diagnosis, guiding life-saving interventions, or providing peace of mind, the information it delivers is invaluable.
Knowing what to expect demystifies the process and empowers you to participate actively in your care. From preparing properly to following post-procedure guidelines, every step contributes to a safer experience and better outcomes.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?