A tracheostomy is a surgical procedure that creates an opening in the neck into the windpipe (trachea) to help a person breathe when normal airflow is obstructed or insufficient. While it may sound intense, this intervention can be life-saving and is performed for a variety of medical conditions affecting breathing. Understanding why a tracheostomy is needed involves examining both acute emergencies and long-term health challenges. From airway obstruction to prolonged mechanical ventilation, this procedure serves critical roles across different clinical settings.
Understanding the Tracheostomy Procedure
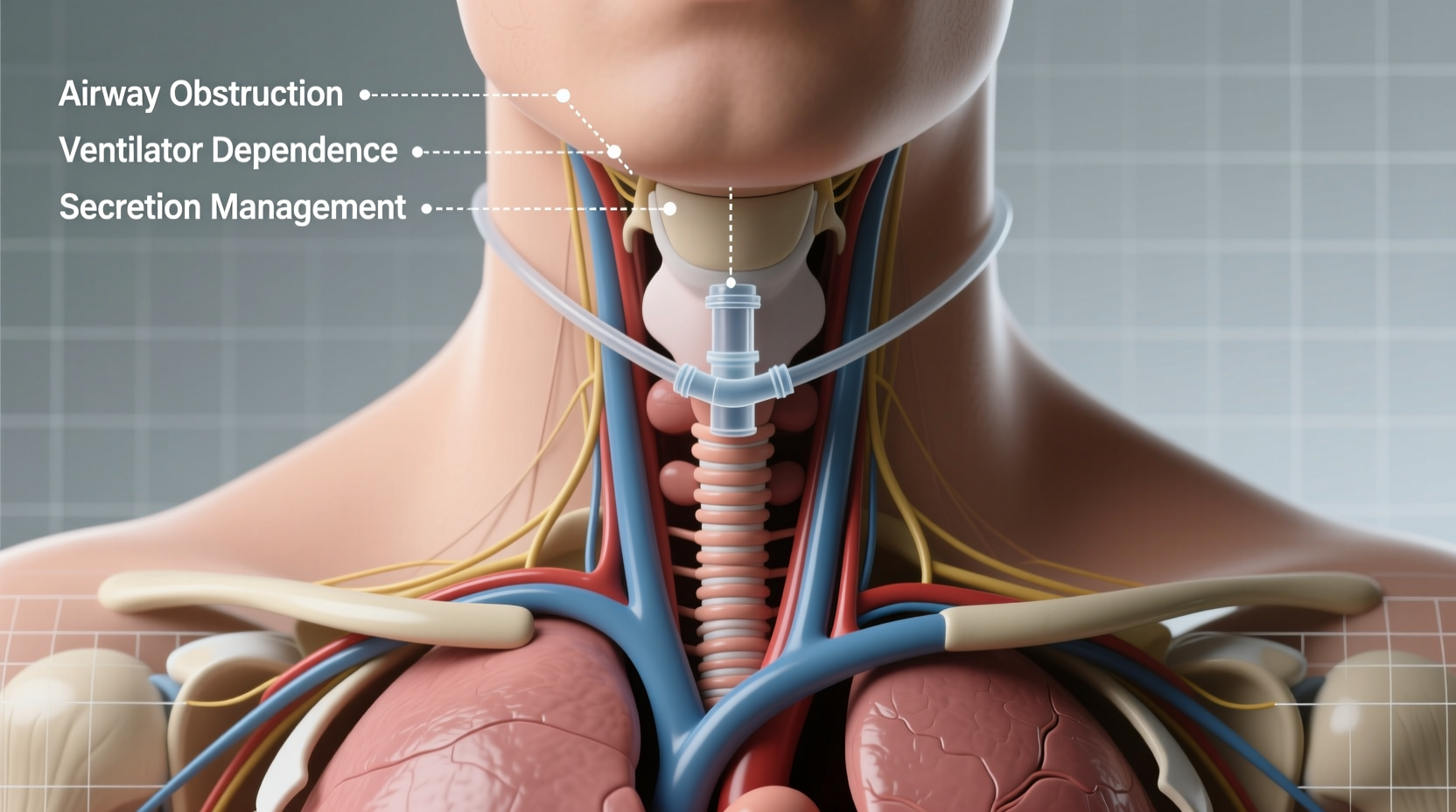
The human respiratory system relies on unobstructed airflow from the nose and mouth down through the larynx and into the trachea. When this pathway is compromised—due to swelling, trauma, tumors, or neurological impairment—breathing becomes difficult or impossible. A tracheostomy bypasses the upper airway by inserting a tube directly into the trachea through a small incision in the front of the neck.
This tube allows air to enter the lungs directly, either on its own or connected to a ventilator. The procedure can be temporary or permanent, depending on the underlying condition. It's typically performed under general anesthesia in an operating room, though emergency tracheotomies may be done at the bedside in intensive care units.
Medical Reasons Why a Tracheostomy Is Needed
There are several well-established clinical indications for performing a tracheostomy. These fall broadly into three categories: airway obstruction, prolonged ventilation needs, and facilitation of secretion management.
Airway Obstruction
One of the most urgent reasons for a tracheostomy is blockage of the upper airway. Causes include:
- Tumors in the throat or larynx
- Severe swelling from infections like epiglottitis
- Facial or neck trauma causing structural damage
- Foreign body impaction not removable via intubation
- Birth defects such as laryngomalacia or subglottic stenosis in infants
In these cases, a tracheostomy provides a secure, alternative route for breathing when endotracheal intubation isn't possible or sustainable.
Prolonged Mechanical Ventilation
Patients in intensive care who require ventilator support for more than 7–10 days are often considered for a tracheostomy. Long-term intubation through the mouth increases risks such as vocal cord injury, sinus infections, and difficulty weaning off the ventilator.
A tracheostomy offers several advantages in this context:
- Greater patient comfort compared to oral tubes
- Easier oral hygiene and reduced risk of pneumonia
- Potential for earlier mobilization and rehabilitation
- Improved ability to speak (with special valves)
“After ten days of intubation, transitioning to a tracheostomy improves survival and quality of care in critically ill patients.” — Dr. Lena Patel, Critical Care Specialist
Impaired Secretion Clearance
Some patients lose the ability to cough effectively due to neuromuscular diseases such as ALS, spinal cord injuries, or advanced Parkinson’s disease. This leads to mucus buildup in the lungs, increasing the risk of aspiration and pneumonia.
A tracheostomy allows direct access to the airway for suctioning, helping clear secretions and maintain lung function. It also reduces the work of breathing in individuals with weak respiratory muscles.
Comparing Tracheostomy vs. Endotracheal Intubation
| Factor | Endotracheal Intubation | Tracheostomy |
|---|---|---|
| Duration Suitability | Short-term (up to 7–10 days) | Long-term or permanent |
| Patient Comfort | Low – tube causes discomfort, limits swallowing | Higher – less invasive once healed |
| Risk of Vocal Cord Damage | High with prolonged use | Lower |
| Ability to Speak | Very limited | Possible with speaking valve |
| Infection Risk | Moderate (ventilator-associated pneumonia) | Lower after initial healing |
| Care Setting | Hospital ICU | ICU, home, long-term care facilities |
Real-Life Scenario: A Case of Prolonged Ventilation
John, a 58-year-old man, was admitted to the ICU with severe pneumonia complicated by sepsis. He required immediate intubation and mechanical ventilation. After two weeks, his doctors determined he wouldn’t be able to come off the ventilator soon due to weakened respiratory muscles and ongoing infection.
To improve his chances of recovery, the care team recommended a tracheostomy. Within days of the procedure, John showed signs of improvement: he was more comfortable, easier to suction, and eventually began working with a speech therapist using a Passy-Muir speaking valve. Six weeks later, he was transferred to a rehabilitation center, where he continued progressing toward independence.
This case illustrates how a timely tracheostomy can shift the trajectory of care from survival mode to active recovery.
Step-by-Step: What Happens During and After a Tracheostomy
- Preoperative Assessment: Imaging and blood tests confirm anatomy and rule out contraindications.
- Surgery: Under anesthesia, a surgeon makes a small incision below the thyroid cartilage and opens the trachea.
- Tubing Insertion: A tracheostomy tube is placed and secured with ties or a strap.
- Initial Monitoring: Patient stays in ICU for close observation of oxygen levels and tube placement.
- Healing & Training: Over days to weeks, the stoma (opening) stabilizes; caregivers learn suctioning and cleaning techniques.
- Rehabilitation: Speech therapy begins if voice restoration is desired; weaning from the ventilator starts when appropriate.
Common Concerns and Frequently Asked Questions
Can you talk after a tracheostomy?
Yes, many patients can speak with the help of a speaking valve, which redirects air through the vocal cords. However, this depends on the individual’s condition and whether the upper airway is functional.
Is a tracheostomy painful?
During healing, there may be mild discomfort, but pain is usually manageable with medication. Once healed, most people adapt well and report improved comfort over long-term intubation.
Can a tracheostomy be reversed?
In many cases, yes. If the underlying condition resolves—such as recovery from illness or removal of an airway tumor—the tube can be removed and the stoma will often close on its own. Some patients require minor surgery to close it completely.
Checklist for Patients and Caregivers
- ✔ Learn proper suctioning techniques from a nurse or respiratory therapist
- ✔ Keep spare tracheostomy tubes and cleaning supplies on hand
- ✔ Monitor for signs of infection: redness, swelling, pus, or fever
- ✔ Ensure humidified air is used, especially in dry environments
- ✔ Attend follow-up appointments with ENT or pulmonology specialists
- ✔ Practice communication strategies (writing board, apps, speaking valve training)
Conclusion: Taking Control Through Informed Care
A tracheostomy is not just a last-resort intervention—it's a strategic medical decision that enhances safety, comfort, and long-term outcomes for patients with complex respiratory needs. Whether due to trauma, chronic illness, or critical care requirements, understanding the purpose and process empowers patients and families to participate actively in recovery.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?