A tracheostomy is a surgical procedure that involves creating an opening in the neck to access the windpipe (trachea), allowing air to bypass the upper airway and enter the lungs directly. While it may sound intense, this intervention can be life-saving or significantly improve quality of life for patients with certain respiratory conditions. Understanding why a tracheostomy is performed requires examining both acute emergencies and chronic medical needs. From prolonged mechanical ventilation to airway obstruction, the reasons are diverse but always rooted in restoring or maintaining effective breathing.
What Is a Tracheostomy?
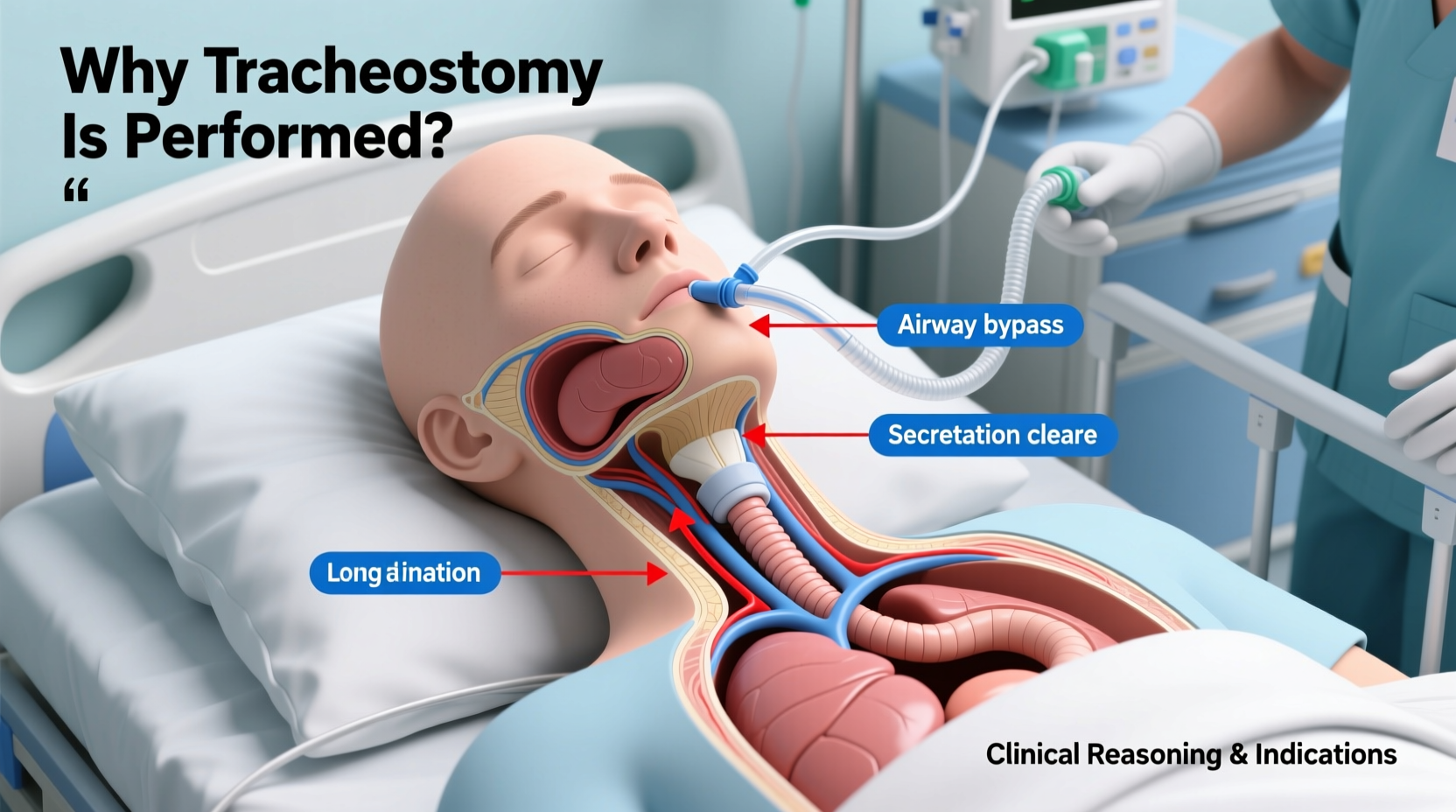
A tracheostomy involves making a small incision in the front of the neck, just below the vocal cords, and inserting a tube called a tracheostomy tube into the trachea. This tube serves as a direct pathway for airflow, enabling patients to breathe without relying on their nose or mouth. The procedure can be temporary or permanent, depending on the underlying condition.
The tracheostomy tube allows for easier suctioning of secretions, reduces the work of breathing, and provides a more stable airway than prolonged intubation through the mouth. It's commonly used in intensive care units, long-term care facilities, and at home under proper medical supervision.
Medical Reasons Why a Tracheostomy Is Performed
There are several primary medical indications for performing a tracheostomy. These fall broadly into two categories: urgent/emergency situations and planned/long-term management.
Airway Obstruction
One of the most critical reasons for a tracheostomy is when the upper airway becomes blocked. Causes include:
- Tumors in the larynx or throat
- Severe swelling from infections like epiglottitis or anaphylaxis
- Facial trauma or burns affecting the airway
- Congenital abnormalities in children
In these cases, immediate access to the trachea ensures oxygen delivery while the underlying issue is treated.
Prolonged Mechanical Ventilation
Patients in the ICU who require ventilator support for more than 7–10 days are often considered for a tracheostomy. Endotracheal intubation (through the mouth) increases risks such as vocal cord damage, sinus infections, and difficulty weaning off the ventilator. A tracheostomy offers:
- Greater patient comfort
- Lower risk of lung infections (ventilator-associated pneumonia)
- Easier oral care and potential for speaking with special valves
- Improved ability to wean from the ventilator gradually
Neurological Conditions Affecting Breathing
Patients with neurological impairments—such as spinal cord injuries, amyotrophic lateral sclerosis (ALS), stroke, or brainstem tumors—may lose the ability to control their airway or cough effectively. A tracheostomy helps manage secretions and supports breathing when the brain’s signals to respiratory muscles are disrupted.
“Tracheostomy can be a bridge to recovery or a vital component of long-term care. The decision balances clinical necessity with quality-of-life considerations.” — Dr. Lena Patel, Pulmonologist and Critical Care Specialist
Emergency vs. Elective Tracheostomy: Key Differences
Not all tracheostomies are performed under the same circumstances. Timing and urgency play major roles in how the procedure is conducted and what outcomes are expected.
| Aspect | Emergency Tracheostomy | Elective Tracheostomy |
|---|---|---|
| Timing | Immediate, life-threatening situation | Planned, often after days in ICU |
| Setting | Operating room or bedside in ICU | Operating room with full anesthesia |
| Risks | Higher due to urgency and limited visibility | Lower, with better preparation |
| Common Causes | Airway blockage, trauma, acute swelling | Prolonged ventilation, neuromuscular disease |
| Recovery Outlook | Depends on resolving the emergency | Often part of long-term care plan |
While emergency tracheostomies are rare thanks to advanced intubation techniques, they remain a crucial skill in trauma centers. Elective procedures, on the other hand, are increasingly common in patients recovering from severe illness, especially post-COVID-19 cases requiring extended ventilatory support.
Step-by-Step: How a Tracheostomy Is Performed
Understanding the process demystifies the procedure and reassures patients and caregivers. Here's a standard sequence for an elective surgical tracheostomy:
- Anesthesia Administration: General anesthesia is given to ensure the patient feels no pain.
- Incision: A horizontal or vertical cut is made in the lower front of the neck, just above the sternum.
- Exposure of Trachea: Muscles and tissues are gently moved aside to expose the tracheal rings.
- Opening the Trachea: A small hole is created between the second and third tracheal rings.
- Tube Insertion: A tracheostomy tube is inserted and secured with sutures or ties around the neck.
- Verification: Breathing is confirmed via the tube, and placement is checked with capnography or bronchoscopy.
- Dressing and Monitoring: The site is cleaned, dressed, and continuously monitored for bleeding or displacement.
Alternative methods, such as percutaneous tracheostomy (using a needle and dilators rather than a scalpel), are often used in ICU settings and take less time with comparable safety when performed by experienced clinicians.
Living With a Tracheostomy: Real-Life Considerations
For many, a tracheostomy is not just a medical intervention—it’s a new way of living. Daily routines change, and adaptation is essential.
Mini Case Study: Recovery After a Severe Stroke
James, a 62-year-old man, suffered a massive ischemic stroke that left him unable to swallow or protect his airway. After being intubated in the ER, he remained on a ventilator for 14 days. His care team decided an elective tracheostomy would improve comfort and aid rehabilitation. Over the next six weeks, James transitioned to a speaking valve, began physical therapy, and eventually learned to communicate and eat again with support. Though he later had the tracheostomy removed, those early weeks were critical to his recovery.
This case illustrates how a tracheostomy isn’t just about survival—it’s about enabling healing and regaining function.
Do’s and Don’ts for Tracheostomy Care
Proper maintenance of the tracheostomy site and tube is vital to prevent complications like infection, blockage, or dislodgement.
| Do’s | Don’ts |
|---|---|
| Wash hands before touching the tube | Ignore signs of redness or swelling |
| Clean the stoma site daily with saline | Allow water to enter the tube during showers without protection |
| Keep spare tubes and cleaning tools handy | Use cotton swabs near the stoma (fibers can enter airway) |
| Humidify inhaled air, especially in dry climates | Smoke or allow others to smoke nearby |
| Attend regular follow-ups with ENT or pulmonology | Force the tube back in if dislodged—call emergency services |
FAQ: Common Questions About Tracheostomy
Can you speak with a tracheostomy?
Yes, many patients can speak using a speaking valve (like a Passy-Muir valve), which redirects air through the vocal cords. However, speaking may be softer or hoarse, and some patients require speech therapy to adapt.
Is a tracheostomy permanent?
Not always. If the underlying condition improves—such as recovery from a severe illness or removal of an airway tumor—the tracheostomy tube can be removed, and the opening usually closes on its own within days. Some patients, especially those with progressive neurological diseases, may need it permanently.
What are the risks of a tracheostomy?
Complications include infection at the site, bleeding, damage to nearby structures (like the esophagus), tube blockage from mucus, or accidental decannulation (tube coming out). Long-term use may lead to tracheal narrowing or collapse, though these are less common with proper care.
Conclusion: A Lifesaving Intervention With Lasting Impact
A tracheostomy is far more than a surgical procedure—it’s a gateway to sustained breathing, recovery, and sometimes, a return to meaningful communication and independence. Whether performed in an emergency to save a life or placed electively to support long-term ventilation, its purpose is always centered on preserving respiratory function and improving patient outcomes. Advances in technique and post-operative care have made tracheostomies safer and more manageable than ever before.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?