For many new parents, breastfeeding is envisioned as a natural, seamless act of bonding and nourishment. Yet, the reality for countless mothers is far more complex. Despite its biological basis, breastfeeding often comes with physical discomfort, emotional strain, logistical hurdles, and societal pressures that make it unexpectedly difficult. Understanding why this happens—and how to navigate the challenges—is essential for both maternal well-being and infant health.
The World Health Organization recommends exclusive breastfeeding for the first six months of life, yet global initiation rates remain inconsistent, and early discontinuation is common. The gap between intention and experience often stems not from lack of desire, but from unmet support, misinformation, or underestimated difficulties. This article examines the most frequent obstacles in breastfeeding, offers evidence-based solutions, and provides practical guidance for those navigating this deeply personal journey.
Physical Challenges and Their Causes
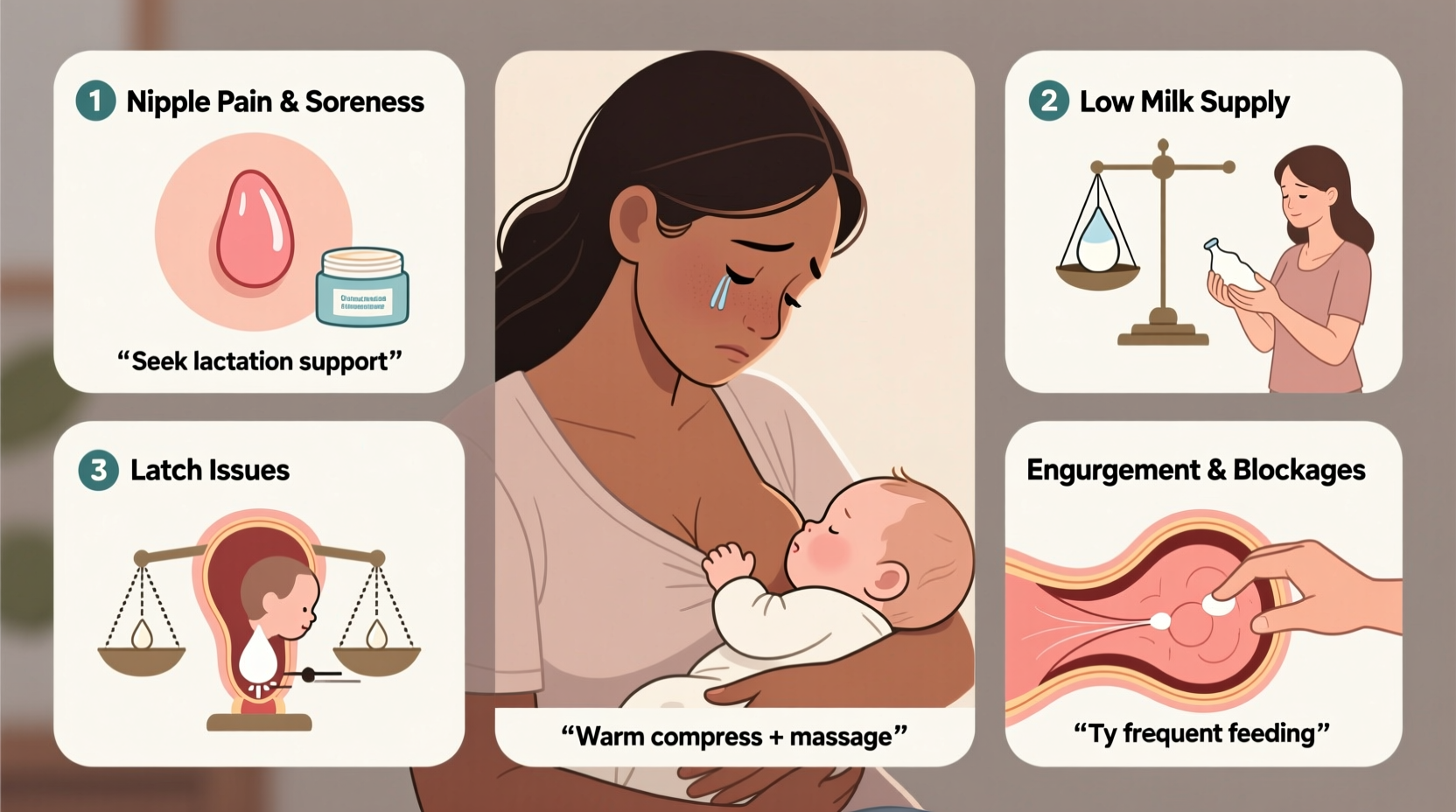
One of the primary reasons breastfeeding feels difficult is the range of physical discomforts that can arise, especially in the early weeks. These are often dismissed as “normal,” but when unmanaged, they can lead to pain, frustration, and early weaning.
- Nipple Pain and Cracking: Often caused by improper latch, where the baby doesn’t take enough breast tissue into their mouth. This leads to friction and trauma on sensitive skin.
- Engorgement: Occurs when breasts become overly full with milk, typically in the first few days postpartum. This can make latching difficult and painful.
- Mastitis: A breast infection marked by fever, redness, swelling, and flu-like symptoms. It usually develops from blocked ducts or bacterial entry through cracked nipples.
- Low or Overactive Milk Supply: Some struggle with producing enough milk; others face forceful letdown and oversupply, which can cause gassiness and feeding refusal in babies.
Emotional and Psychological Barriers
Beyond the physical, breastfeeding impacts mental health in profound ways. Sleep deprivation, hormonal shifts, and societal expectations amplify stress, making what should be an intimate experience feel isolating.
New mothers frequently report feelings of inadequacy when comparing themselves to idealized images of effortless nursing. The pressure to “do it all” without visible struggle can silence those experiencing difficulty. Postpartum anxiety and depression may also manifest or worsen due to the relentless demands of feeding every 2–3 hours.
“We expect women to breastfeed like experts on day one, yet provide little hands-on support. The emotional toll of feeling like you’re failing your baby—even when doing everything right—can be devastating.” — Dr. Rebecca Stone, OB-GYN and Lactation Consultant
Solutions and Support Strategies
Many breastfeeding challenges are preventable or manageable with timely intervention. Here’s a breakdown of effective approaches:
1. Seek Early Lactation Support
Consulting a certified lactation consultant (IBCLC) within the first 48 hours post-birth significantly improves outcomes. They assess latch mechanics, measure milk transfer, and offer personalized plans.
2. Master Proper Positioning
Experiment with positions like the cradle hold, football hold, or side-lying to find comfort and efficiency. Proper alignment reduces strain on both mother and baby.
3. Use Tools Wisely
Pumps, nipple shields, and breast compressions can be helpful when used correctly. However, over-reliance on pumping may reduce supply if it replaces direct nursing.
4. Build a Support Network
Partner involvement, peer support groups (in-person or online), and encouragement from family members help sustain motivation during tough phases.
| Challenge | Immediate Solution | Long-Term Strategy |
|---|---|---|
| Nipple Pain | Correct latch, use lanolin | Lactation consult, positioning practice |
| Engorgement | Frequent feeding, cold packs | Establish feeding rhythm, avoid over-pumping |
| Mastitis | Rest, hydration, antibiotics if needed | Treat blocked ducts early, maintain drainage |
| Low Supply | More nursing, skin-to-skin contact | Address underlying causes (e.g., thyroid issues) |
Real-Life Example: Maria’s Journey
Maria, a first-time mother from Austin, Texas, planned to exclusively breastfeed her daughter. Within days, she developed severe nipple cracking and was told by hospital staff that “some pain is normal.” By week two, she was crying through each feed, her baby wasn’t gaining weight, and she felt like a failure.
After connecting with a local lactation specialist, Maria learned her baby had a tongue tie restricting proper latch. Once corrected with a simple procedure, and with guided repositioning techniques, feeding became manageable. She continued nursing for ten months, later saying, “I didn’t need more willpower—I needed accurate information and someone who listened.”
Step-by-Step Guide to Improving Breastfeeding Success
- Assess Latch Early: Ensure baby’s mouth covers most of the areola, not just the nipple. Chin should be touching the breast, nose clear.
- Feed On Demand: Newborns need 8–12 feeds per 24 hours. Follow hunger cues rather than strict schedules.
- Monitor Output: Track wet and dirty diapers (at least 6 wet and 3–4 stools per day by day 5).
- Address Pain Immediately: Don’t endure persistent pain. Seek help before minor issues escalate.
- Stay Hydrated and Nourished: Nursing burns 300–500 extra calories daily. Eat balanced meals and drink water consistently.
- Know When to Supplement: If medically necessary, use supplemental nursing systems or paced bottle feeding to avoid nipple confusion.
- Reevaluate Goals Regularly: Breastfeeding doesn’t have to be all-or-nothing. Partial breastfeeding still offers significant benefits.
Frequently Asked Questions
Is it normal to feel intense pain while breastfeeding?
Some tenderness in the first few days may occur, but sharp, lasting pain is not normal. It usually indicates poor latch or another issue that can be corrected with support.
Can I still breastfeed if I return to work?
Yes. Many parents successfully combine breastfeeding with employment using pumping at work, stored milk, and supportive childcare arrangements. Employers are increasingly required to provide break time and private space under U.S. law.
What if I simply can’t produce enough milk?
True low supply is less common than perceived. Factors like infrequent feeding, certain medications, or hormonal conditions (e.g., PCOS, thyroid disorders) can affect production. A lactation professional can help identify causes and explore options like galactagogues or supplemental feeding.
Conclusion: Redefining Success
Breastfeeding is neither inherently easy nor universally difficult—it is deeply human. Its challenges stem not from individual failure, but from a system that often under-supports new parents. With access to skilled care, realistic expectations, and compassionate communities, many obstacles can be overcome.
Success isn’t defined by duration or exclusivity, but by informed choice and well-being. Whether you nurse for one week or one year, every drop counts. If you’re struggling, reach out. You’re not alone, and support is available.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?