For women navigating menopause, hormone replacement therapy (HRT) can offer significant relief from symptoms like hot flashes, night sweats, mood swings, and vaginal dryness. One widely prescribed option is the Combipatch—a transdermal patch that delivers both estrogen and progestin. While effective, many patients are shocked by its high cost, often paying hundreds of dollars per month without insurance. Understanding why Combipatch is so expensive, how coverage varies, and what alternatives exist can help patients make informed, budget-conscious decisions.
Why Is Combipatch So Expensive?
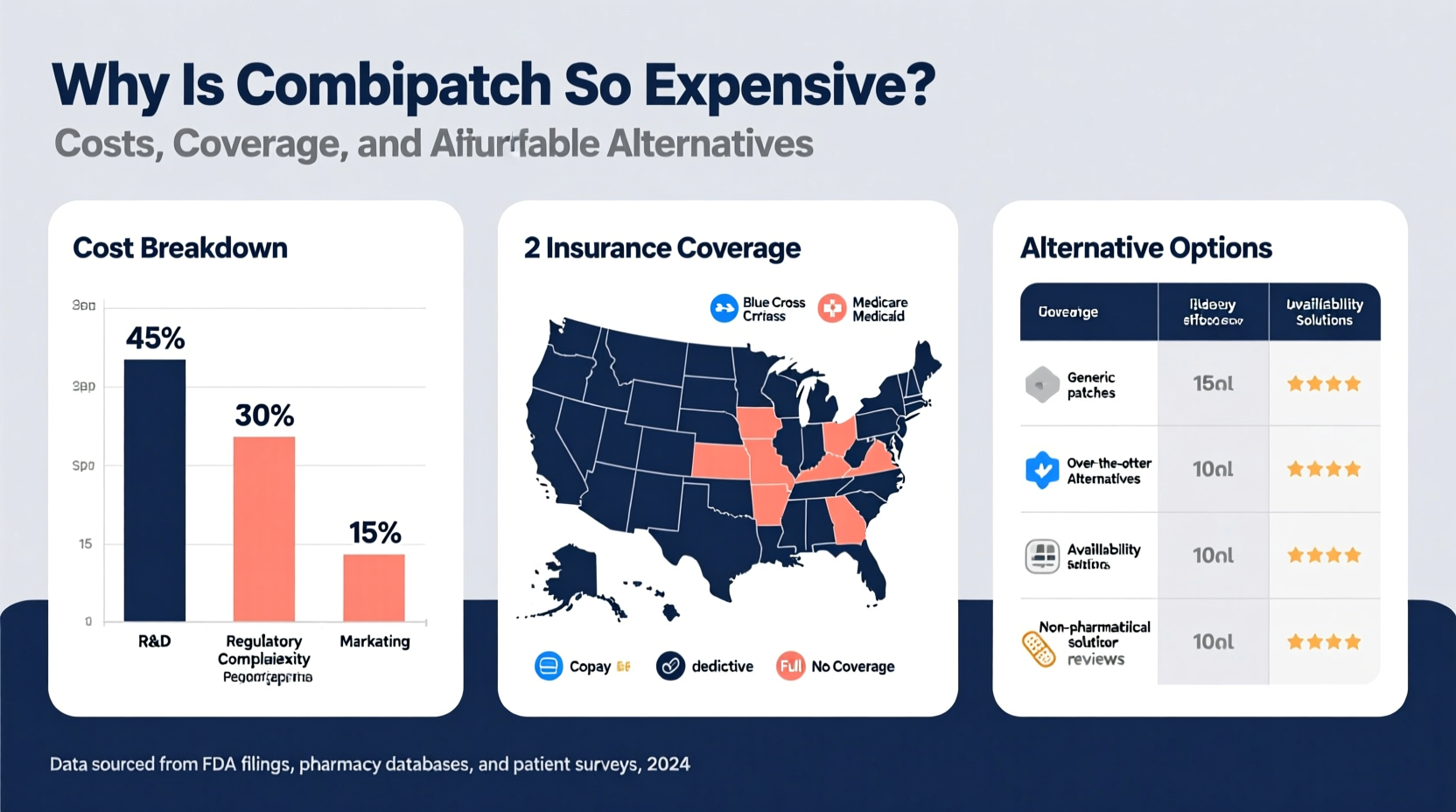
The sticker shock of a $300–$500 monthly prescription for Combipatch isn’t uncommon. Several interrelated factors contribute to its high price:
- Brand-name monopoly: Combipatch is manufactured by Noven Pharmaceuticals and remains under patent protection in the U.S., limiting generic competition.
- Transdermal delivery system: The patch uses advanced adhesive and controlled-release technology, which increases manufacturing complexity and cost.
- Regulatory hurdles: FDA approval for combination hormone patches requires extensive clinical data, raising development costs passed on to consumers.
- Pharmacy benefit manager (PBM) markups: Intermediaries between insurers and pharmacies often inflate prices through rebates and spread pricing.
- Limited insurance negotiation power: Smaller patient populations for HRT compared to chronic disease drugs reduce pressure on manufacturers to lower prices.
“Even with insurance, patients are often surprised by out-of-pocket costs because hormone therapies like Combipatch aren’t always prioritized on formularies.” — Dr. Linda Park, Endocrinologist and Women’s Health Specialist
Insurance Coverage: What to Expect
Insurance coverage for Combipatch varies significantly by plan. Medicare Part D and most private insurers cover it, but often place it on higher-tier formularies, resulting in elevated co-pays.
Typical coverage tiers include:
| Tier | Description | Estimated Co-Pay |
|---|---|---|
| Tier 1 | Preferred generics | $5–$10 |
| Tier 2 | Preferred brand-name drugs | $30–$60 |
| Tier 3 | Non-preferred brands | $80–$150 |
| Tier 4 | Specialty medications | 25%–33% of total cost (often $200+) |
Combipatch typically falls into Tier 3 or 4. Some insurers require prior authorization or step therapy—meaning you must try cheaper alternatives first before approving Combipatch.
How to Maximize Insurance Benefits
- Review your plan’s drug formulary online or call customer service.
- Ask your doctor to submit a prior authorization if required.
- Use manufacturer savings programs—if available (Noven offers limited assistance).
- Consider using a pharmacy not tied to your insurer’s network if cash price is lower.
Affordable Alternatives to Combipatch
For those facing high costs, several effective and more affordable alternatives exist. These options deliver similar hormonal benefits with potentially lower price tags.
Generic Transdermal Patches
Few direct generics exist for Combipatch due to its dual-hormone formulation, but some pharmacists can compound custom patches. More commonly, patients use separate estrogen patches (like Estraderm or generic estradiol patches) combined with oral progesterone.
Oral Hormone Therapy
Combination pills such as Prempro (conjugated estrogens + medroxyprogesterone) are often significantly cheaper, especially in generic form. A 30-day supply can cost as little as $10–$40 with insurance or through discount programs like GoodRx.
Bioidentical Hormones
Compounded bioidentical hormones—custom-mixed by specialty pharmacies—offer tailored dosing. While not FDA-approved and often not covered by insurance, they may provide symptom relief at competitive cash prices ($50–$100/month).
Other Delivery Methods
- Vaginal rings (e.g., Femring): Delivers low-dose estrogen locally; useful for urogenital symptoms.
- Gels and sprays: Estrogen-based topical applications with flexible dosing.
- Progestin-only options: For women who need progesterone support but cannot tolerate systemic estrogen.
“Switching from a branded patch to an oral generic reduced my monthly HRT cost from $420 to $35. My symptoms improved just as much.” — Susan M., 54, patient advocate
Step-by-Step Guide to Reducing Your HRT Costs
If Combipatch is financially out of reach, follow this practical timeline to find a sustainable alternative:
- Month 1: Audit Your Current Prescription
Check your insurance explanation of benefits (EOB) and pharmacy receipt. Note the retail price, insurance payment, and your co-pay. - Month 1: Consult Your Doctor
Discuss cost concerns openly. Ask about equivalent therapies and whether switching formulations would suit your health profile. - Month 1: Explore Pharmacy Options
Compare prices at major chains (CVS, Walgreens), warehouse clubs (Costco), and online pharmacies (Phil International, Canada Pharmacy Online). - Month 2: Try a Lower-Cost Alternative
Begin a trial of a generic oral HRT under medical supervision. Track symptoms weekly. - Month 3: Evaluate and Adjust
Return to your provider to assess effectiveness and side effects. Refine dosage or delivery method as needed.
Real-World Example: Managing Costs Without Sacrificing Care
Martha, a 57-year-old teacher from Ohio, was prescribed Combipatch for severe night sweats. Her insurance required a $180 monthly co-pay—unaffordable on a fixed income. After discussing options with her OB-GYN, she switched to generic estradiol patches (applied twice weekly) and oral micronized progesterone. Her new regimen cost $65/month with insurance and provided comparable symptom relief. She also enrolled in a patient assistance program through her pharmacy, reducing the cost further during a temporary coverage gap.
This case highlights that while Combipatch may be clinically appropriate, it’s not the only path to symptom management. Open dialogue with healthcare providers and proactive cost research are key.
Frequently Asked Questions
Is there a generic version of Combipatch?
No true generic exists yet due to patent protections. However, equivalent hormone combinations are available via separate estrogen patches and oral progestins, often at a fraction of the cost.
Why is the patch more expensive than pills?
Patches involve complex delivery systems, lower production volume, and less generic competition. Pills, especially older formulations, benefit from decades of market competition and streamlined manufacturing.
Can I buy Combipatch from international pharmacies?
Yes, but proceed with caution. Pharmacies in Canada or the UK may offer lower prices, but ensure they are accredited (look for CIPA or VIPPS certification). Importing medication carries legal and safety risks if not done properly.
Conclusion: Take Control of Your Treatment and Budget
The high cost of Combipatch reflects broader issues in pharmaceutical pricing, particularly for niche, patented therapies. But patients aren’t powerless. By understanding insurance dynamics, exploring equally effective alternatives, and advocating for transparent pricing, it’s possible to manage menopausal symptoms without financial strain. Hormone therapy should enhance quality of life—not jeopardize financial stability. Talk to your doctor, compare options, and insist on solutions that work for both your body and your budget.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?