Ebola virus disease (EVD), once considered a rare and geographically confined illness, has emerged as one of the most feared infectious diseases in modern history. With fatality rates reaching up to 90% in some outbreaks, Ebola stands out not only for its high mortality but also for the speed and severity with which it can devastate individuals and communities. Understanding why Ebola is so deadly requires examining its biology, immune evasion tactics, transmission patterns, and the challenges in treatment and containment.
The Nature of the Ebola Virus
Ebola belongs to the *Filoviridae* family, named for its thread-like structure visible under electron microscopy. First identified in 1976 near the Ebola River in the Democratic Republic of Congo, the virus exists in several strains—Zaire, Sudan, Bundibugyo, Taï Forest, and Reston—with the Zaire strain being the most lethal.
Unlike many viruses that target specific organs or systems, Ebola is systemic. It enters the body through mucous membranes, breaks in the skin, or contact with infected bodily fluids. Once inside, it rapidly infects dendritic cells, macrophages, and liver cells—key components of the immune system and metabolism. This early targeting cripples the body’s ability to mount an effective defense, allowing the virus to replicate unchecked.
How Ebola Attacks the Body
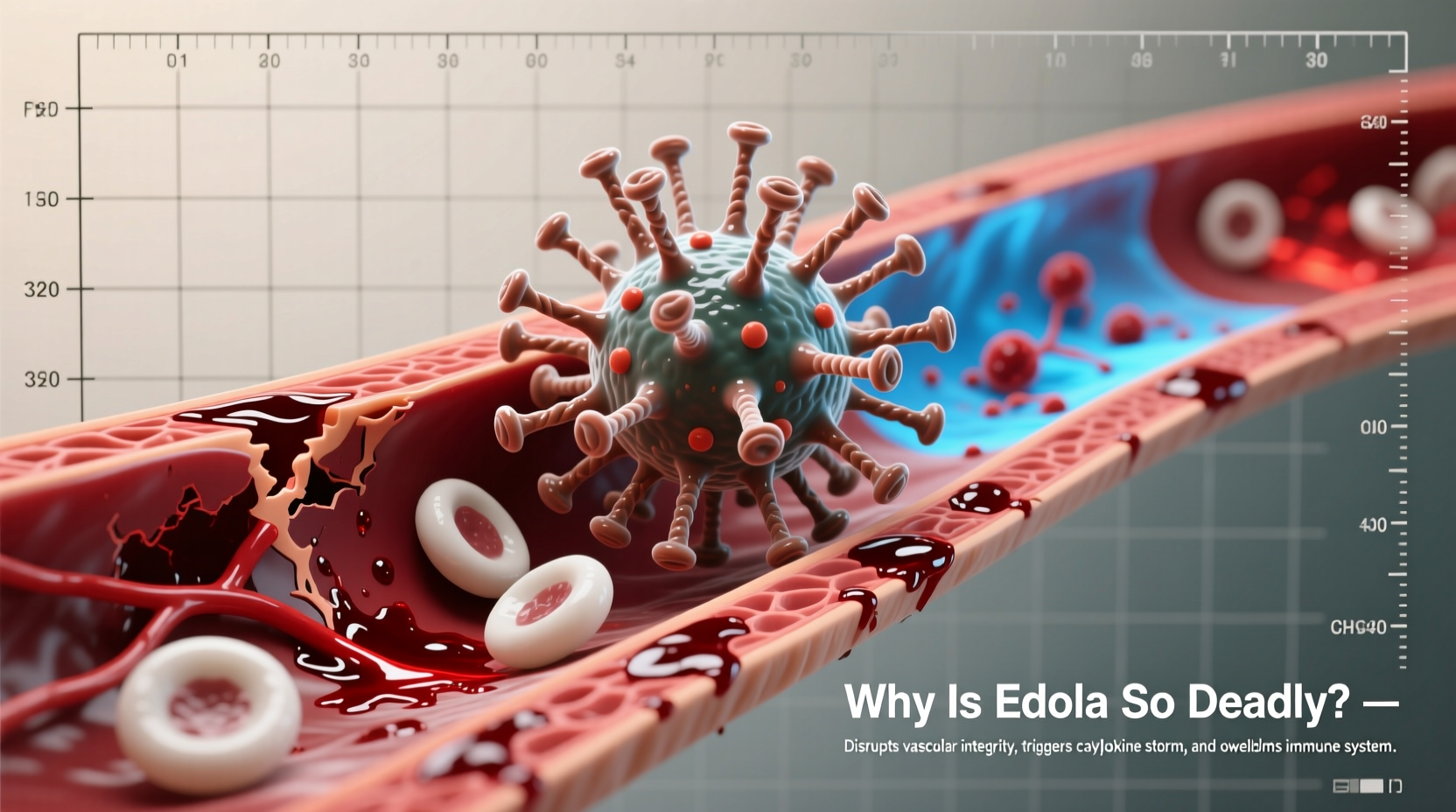
Ebola’s deadliness stems from its multifaceted assault on human physiology. After entering host cells, the virus hijacks cellular machinery to produce thousands of copies of itself. As infected cells burst, they release viral particles into the bloodstream, spreading the infection throughout the body.
One of the most devastating effects occurs in the vascular system. Ebola damages endothelial cells lining blood vessels, causing them to become leaky. This leads to internal bleeding, hypotension, and shock—hallmarks of severe EVD. Additionally, the virus triggers a “cytokine storm,” an overreaction of the immune system that causes widespread inflammation, organ failure, and tissue damage.
The liver and kidneys are particularly vulnerable. Liver dysfunction impairs clotting factor production, worsening hemorrhage. Kidney failure disrupts electrolyte balance and fluid regulation, further destabilizing vital functions. In advanced stages, patients may experience vomiting blood, bloody diarrhea, and petechial rashes—signs of coagulopathy and multi-organ collapse.
“Ebola doesn’t just kill by direct cell destruction—it orchestrates a catastrophic failure of the entire physiological network.” — Dr. Peter Piot, microbiologist and co-discoverer of the Ebola virus
Immune System Evasion Tactics
What sets Ebola apart from many other viruses is its sophisticated ability to evade and suppress the immune response. It produces proteins such as VP24 and VP35 that block interferon signaling—the body’s primary alarm system against viral invaders. Without this warning, the immune system remains blind to the infection during critical early stages.
Furthermore, Ebola disables antigen presentation, preventing T-cells from recognizing infected cells. This means even when the immune system eventually activates, it struggles to locate and destroy viral reservoirs. By the time symptoms appear, viral load is often too high for the body to recover without intensive medical support.
| Mechanism | Effect on Host | Consequence |
|---|---|---|
| VP35 protein | Inhibits interferon production | Delays immune detection |
| VP24 protein | Blocks interferon signaling | Prevents antiviral state in cells |
| Glycoprotein coating | Masks virus from antibodies | Reduces neutralization effectiveness |
| Infection of dendritic cells | Disables antigen presentation | T-cell response impaired |
Transmission and Outbreak Dynamics
Ebola spreads through direct contact with blood, secretions, or organs of infected individuals—or surfaces contaminated with these fluids. Unlike airborne viruses such as influenza or SARS-CoV-2, Ebola requires close physical interaction, which limits its spread but increases risk among caregivers, healthcare workers, and those involved in burial rituals.
During outbreaks, traditional funeral practices involving washing or touching the deceased have been major drivers of transmission. A single funeral can spark dozens of new cases. Urbanization and increased mobility have also contributed to larger, more complex outbreaks, as seen in the 2014–2016 West Africa epidemic—the largest in history, with over 28,000 cases and 11,000 deaths.
Key Factors in Rapid Spread
- Lack of public awareness about transmission routes
- Weak healthcare infrastructure in affected regions
- Delayed international response
- Stigma leading to avoidance of treatment centers
Treatment Challenges and Medical Response
For decades, Ebola had no approved antiviral treatment or vaccine. Care was limited to supportive therapy: rehydration, electrolyte management, oxygen support, and treating secondary infections. Even with optimal care, survival depended heavily on the strength of the patient’s immune response and early intervention.
This changed in recent years. Monoclonal antibody therapies like Inmazeb (a combination of three antibodies) and Ebanga (single antibody) have shown significant efficacy in neutralizing the virus. The rVSV-ZEBOV vaccine, proven effective during the 2018–2020 outbreak in the DRC, is now used in ring vaccination strategies to contain spread.
Despite these advances, access remains a challenge. Treatments require cold-chain storage and intravenous administration—difficult in remote areas with limited electricity and trained personnel. Vaccination campaigns face logistical hurdles and community mistrust, especially where misinformation about Western medicine persists.
Step-by-Step: Containing an Ebola Outbreak
- Case Identification: Detect suspected cases through symptom screening and lab confirmation.
- Isolation: Immediately isolate infected individuals to prevent further spread.
- Contact Tracing: Identify and monitor all individuals who had contact with the patient.
- Vaccination: Administer rVSV-ZEBOV vaccine to high-risk contacts (ring vaccination).
- Safe Burials: Conduct burials using protective gear and without direct contact.
- Community Engagement: Educate the public on transmission and prevention.
- Healthcare Protection: Equip clinics with PPE and infection control protocols.
Mini Case Study: The 2014 West Africa Epidemic
The 2014 Ebola outbreak began in Guinea when a two-year-old child died after contact with bats—likely the zoonotic source. The virus spread silently across borders into Liberia and Sierra Leone. Weak health systems, cross-border movement, and delayed global response allowed the outbreak to spiral.
By the time WHO declared a Public Health Emergency of International Concern in August 2014, thousands were infected. Healthcare workers were disproportionately affected; in some regions, over 50% of doctors and nurses died. International aid eventually helped build treatment units and deploy experimental treatments, but not before the virus claimed more lives than all previous outbreaks combined.
This case underscores how social, political, and infrastructural factors amplify biological lethality. Ebola is deadly not just because of its pathology, but because it exploits vulnerabilities in human systems.
Frequently Asked Questions
Can survivors still transmit Ebola after recovery?
Yes. While survivors clear the virus from their blood, Ebola can persist in immune-privileged sites like semen, eyes, and spinal fluid for months. Men are advised to abstain from sex or use condoms for at least 12 months post-recovery.
Is there a cure for Ebola?
There is no universal \"cure,\" but monoclonal antibody treatments have dramatically improved survival rates. When administered early, drugs like Inmazeb increase survival to over 90% in clinical settings.
Can Ebola be prevented?
Yes. Prevention includes avoiding contact with infected individuals or wildlife, practicing safe burial rites, wearing PPE in healthcare settings, and vaccination during outbreaks.
Conclusion: Turning Knowledge Into Action
Ebola’s lethality lies not in a single trait, but in a convergence of biological aggression, immune sabotage, and societal vulnerability. Its high fatality rate reflects both the virus’s efficiency and the fragility of health systems in the regions it affects.
Understanding why Ebola is so deadly empowers better preparedness. Investment in surveillance, rapid diagnostics, accessible treatments, and community education is essential. With continued research and global cooperation, future outbreaks can be detected earlier, contained faster, and ultimately overcome.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?