The gallbladder, a small pear-shaped organ beneath the liver, plays a role in storing and concentrating bile—a digestive fluid produced by the liver. While not essential for survival, issues affecting the gallbladder can lead to significant discomfort and health risks. In many cases, surgical removal—known as cholecystectomy—becomes the most effective treatment. Understanding why gallbladder removal is necessary, the conditions that prompt it, and what to expect can help patients make informed decisions about their care.
Common Medical Reasons for Gallbladder Removal
Gallbladder removal is one of the most frequently performed abdominal surgeries worldwide. It is typically recommended when the gallbladder causes recurring pain or complications due to disease. The most common reasons include:
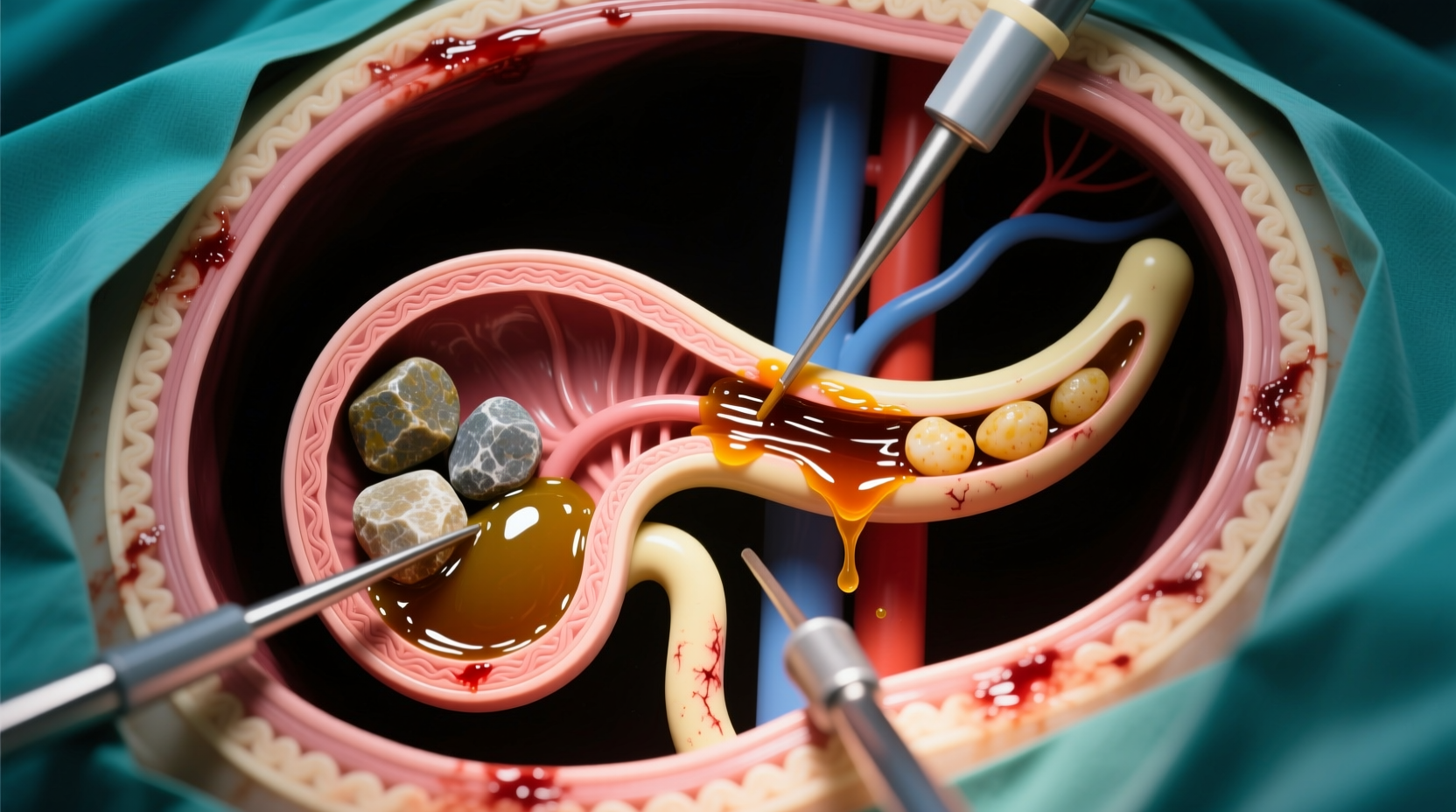
- Gallstones (Cholelithiasis): Hardened deposits of digestive fluid that form in the gallbladder. They can block bile ducts, leading to inflammation, infection, or pancreatitis.
- Cholecystitis: Inflammation of the gallbladder, often caused by gallstones blocking the cystic duct. Acute cholecystitis requires urgent medical attention.
- Biliary colic: Episodes of severe upper abdominal pain caused by temporary blockage of the bile duct by a stone.
- Pancreatitis: Inflammation of the pancreas, often triggered when a gallstone migrates and blocks the pancreatic duct.
- Gallbladder polyps or tumors: Growths within the gallbladder wall that may be precancerous or cancerous, especially if larger than 10 mm.
- Acalculous gallbladder disease: Chronic gallbladder dysfunction without stones, diagnosed when symptoms mimic biliary pain but imaging shows no stones.
When Surgery Becomes Necessary: Clinical Indicators
Not everyone with gallstones requires surgery. Many are asymptomatic and never develop complications. However, once symptoms arise, the likelihood of recurrence is high. Doctors assess several factors before recommending removal:
- Recurrent biliary pain: Pain lasting more than a few hours, typically in the upper right or central abdomen, often radiating to the back or shoulder.
- Evidence of complications: Imaging or lab tests showing signs of infection, obstruction, or inflammation.
- Immunocompromised status: Patients with weakened immune systems may undergo preventive removal due to higher risk of severe complications.
- Poor gallbladder function: A HIDA scan may reveal low ejection fraction (<35%), indicating the organ isn’t emptying properly.
“Once symptomatic gallstones are confirmed, cholecystectomy is the definitive treatment. Delaying surgery increases the risk of emergency intervention.” — Dr. Alan Reyes, Gastrointestinal Surgeon
Types of Gallbladder Surgery and Recovery Timeline
Most gallbladder removals today are performed laparoscopically, using small incisions and a camera-guided system. In complex cases, an open procedure may be required.
| Surgery Type | Procedure Duration | Recovery Time | Hospital Stay |
|---|---|---|---|
| Laparoscopic Cholecystectomy | 60–90 minutes | 1–2 weeks | Same day or overnight |
| Open Cholecystectomy | 90–120 minutes | 4–6 weeks | 3–5 days |
Step-by-Step Surgical Process
- Preoperative Evaluation: Blood work, ultrasound, and possibly CT or MRI to confirm diagnosis.
- Anesthesia: General anesthesia is administered.
- Incisions: Four small cuts for laparoscopic surgery; one large abdominal incision for open surgery.
- Gallbladder Removal: The organ is detached from the liver and bile ducts and removed.
- Closure: Incisions are sutured and bandaged.
- Recovery Monitoring: Patients are observed for several hours before discharge.
Real-World Case: Delayed Surgery Leads to Complications
Sarah, a 42-year-old teacher, experienced intermittent upper abdominal pain for six months. She dismissed it as indigestion until she developed fever, jaundice, and severe pain. An ER visit revealed acute cholecystitis with a blocked bile duct. Imaging showed multiple gallstones, and her white blood cell count was elevated—indicating infection.
She underwent emergency laparoscopic cholecystectomy after being stabilized with IV antibiotics. Her recovery took longer than average due to the inflammation. Her surgeon noted that earlier elective surgery could have prevented the crisis.
This case illustrates how delaying treatment for symptomatic gallstones can escalate into serious complications, including abscess formation, sepsis, or the need for more invasive procedures.
Risks and Considerations Before Surgery
While cholecystectomy is generally safe, all surgeries carry some risks. Potential complications include:
- Bile leakage into the abdomen
- Infection at incision sites
- Damage to the bile ducts (rare but serious)
- Bleeding or adverse reaction to anesthesia
- Post-cholecystectomy syndrome (persistent digestive symptoms in 5–40% of patients)
Patient selection is critical. Those with heart or lung conditions may face higher surgical risks. A thorough preoperative assessment helps minimize these dangers. Additionally, patients should disclose all medications, especially blood thinners, which may need to be adjusted.
Do’s and Don’ts After Diagnosis
| Do | Don't |
|---|---|
| Follow up with your doctor if you have recurrent abdominal pain | Ignore persistent nausea or vomiting with pain |
| Maintain a balanced, low-fat diet | Consume greasy or fried foods regularly |
| Stay hydrated and active post-surgery | Lift heavy objects during early recovery |
| Attend all follow-up appointments | Delay surgery if symptoms are worsening |
Frequently Asked Questions
Can you live normally without a gallbladder?
Yes. The liver continues to produce bile, which flows directly into the small intestine. Most people adjust within weeks and resume normal diets, though some may experience temporary diarrhea or bloating with fatty meals.
Is gallbladder removal always necessary for gallstones?
No. Asymptomatic gallstones usually don’t require surgery. However, if stones cause pain, inflammation, or complications, removal is strongly advised to prevent future emergencies.
What happens if gallbladder problems are left untreated?
Untreated gallbladder disease can lead to severe complications such as gangrene, perforation, bile duct infections (cholangitis), or pancreatitis—all of which can be life-threatening and require urgent intervention.
Conclusion: Taking Action for Long-Term Health
Gallbladder removal becomes necessary when the organ poses a threat to health through chronic pain, infection, or risk of systemic complications. With modern surgical techniques, the procedure is highly effective and carries a low complication rate. Recognizing symptoms early, seeking timely evaluation, and following medical advice can prevent avoidable crises.
If you or a loved one are experiencing symptoms suggestive of gallbladder disease, don’t wait for a medical emergency. Consult a healthcare provider to discuss your options. Proactive management leads to better outcomes, faster recovery, and improved quality of life.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?