The Gram stain remains one of the most pivotal techniques in microbiology, serving as the first step in identifying bacterial pathogens. Developed by Danish physician Hans Christian Gram in 1884, this staining method differentiates bacteria into two broad categories—Gram-positive and Gram-negative—based on structural differences in their cell walls. Its classification power lies not in mere coloration, but in its ability to reveal critical biological distinctions that inform clinical decisions. Understanding why the Gram stain is considered a differential stain requires examining both its mechanism and its practical impact on diagnostics and treatment.
What Makes a Stain “Differential”?
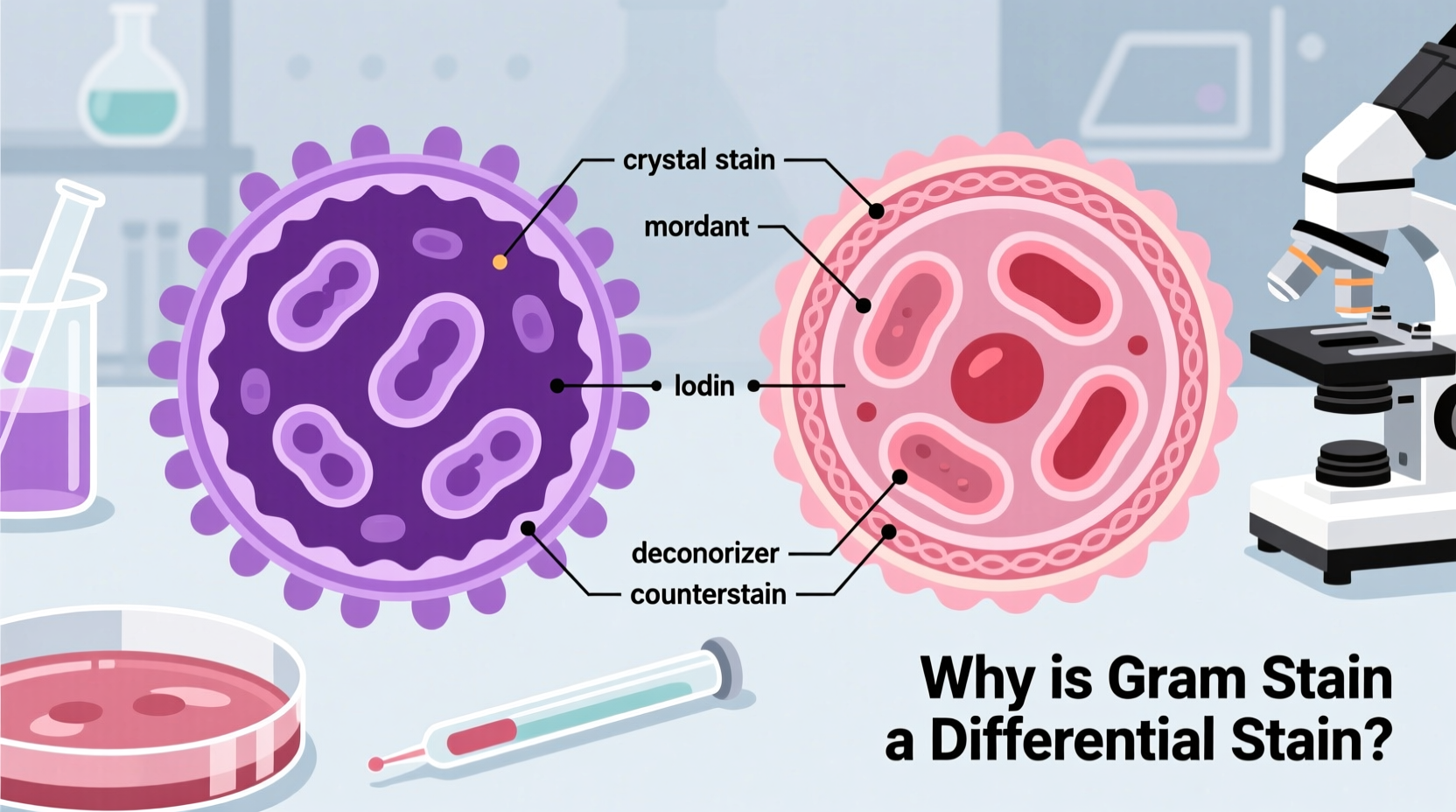
A differential stain allows microbiologists to distinguish between different types of microorganisms or cellular components within a sample. Unlike simple stains that color all cells uniformly, differential stains use multiple dyes and controlled decolorization steps to highlight biochemical or structural variations.
The Gram stain qualifies as differential because it separates bacteria into distinct groups based on how their cell walls retain or lose the primary stain (crystal violet) during a decolorization step. This outcome isn’t random—it reflects fundamental differences in cell wall composition:
- Gram-positive bacteria have a thick layer of peptidoglycan that traps the crystal violet-iodine complex, resisting decolorization.
- Gram-negative bacteria possess a thinner peptidoglycan layer and an outer lipid membrane, which allows the crystal violet to be washed away during decolorization.
This binary result—purple (Gram-positive) or pink/red (Gram-negative)—provides immediate, actionable information about the organism’s identity and potential resistance mechanisms.
The Step-by-Step Process of Gram Staining
The reliability of the Gram stain hinges on precise execution. Each stage plays a specific role in creating the final contrast between bacterial types. Here's the standard sequence used in clinical and research laboratories:
- Primary Stain: Apply crystal violet to the heat-fixed bacterial smear for 1 minute. All cells absorb this purple dye.
- Mordant: Add Gram’s iodine, which forms a large crystal violet-iodine complex inside the cells, anchoring the dye.
- Decolorization: Introduce ethanol or acetone-alcohol for 10–15 seconds. This is the critical step: it dissolves the outer membrane of Gram-negative bacteria and washes out the stain, while Gram-positive cells retain the complex due to their dense peptidoglycan.
- Counterstain: Use safranin (a red dye) for 30–60 seconds. It stains the now-colorless Gram-negative cells, making them visible under the microscope.
After each step, the slide is gently rinsed with water to remove excess reagent without disturbing the specimen. The final result is examined under oil immersion at 1000x magnification.
Why Decolorization Is the Make-or-Break Step
No other step influences accuracy more than decolorization. Under-decolorizing leaves both types of bacteria purple, leading to misclassification of Gram-negative organisms. Over-decolorizing may strip even Gram-positive cells of the stain, causing false negatives.
Experienced technicians adjust timing based on smear thickness and bacterial load. Automated staining systems help reduce variability, but manual oversight remains essential in complex cases.
“Accurate Gram staining can guide antibiotic selection before culture results are available. It’s often the first clue in fighting sepsis.” — Dr. Linda Harper, Clinical Microbiologist
Applications in Medicine and Research
The Gram stain is far more than a classroom demonstration—it has real-world implications across healthcare and science.
Clinical Diagnosis
In emergency departments and microbiology labs, a rapid Gram stain from a blood culture, sputum, or cerebrospinal fluid can determine whether an infection is likely caused by Gram-positive cocci (e.g., Staphylococcus aureus) or Gram-negative rods (e.g., Escherichia coli). This distinction informs initial empiric therapy.
For example, meningitis suspected to be bacterial may prompt immediate administration of ceftriaxone and vancomycin—one targeting Gram-negatives, the other covering resistant Gram-positives—based solely on preliminary Gram stain findings.
Antibiotic Selection
Gram status correlates with antibiotic susceptibility. Beta-lactam antibiotics like penicillin are generally more effective against Gram-positive bacteria due to easier access to their exposed peptidoglycan. In contrast, Gram-negative bacteria are inherently more resistant due to their outer membrane, which blocks many drugs.
Thus, knowing the Gram reaction helps clinicians narrow down appropriate treatments faster, improving patient outcomes and reducing unnecessary broad-spectrum use.
Research and Quality Control
Beyond medicine, researchers use the Gram stain to verify bacterial cultures, assess contamination, or characterize newly isolated strains. In food safety and environmental testing, it helps screen for pathogenic bacteria in samples.
| Feature | Gram-Positive Bacteria | Gram-Negative Bacteria |
|---|---|---|
| Cell Wall Thickness | Thick peptidoglycan (20–80 nm) | Thin peptidoglycan (2–7 nm) |
| Outer Membrane | Absent | Present (lipopolysaccharides) |
| Crystal Violet Retention | Yes (appears purple) | No (appears pink after counterstain) |
| Common Examples | Staphylococcus, Streptococcus | E. coli, Pseudomonas |
| Endotoxin Production | No | Yes (LPS causes fever, shock) |
Limitations and Common Pitfalls
Despite its utility, the Gram stain has limitations that must be recognized to avoid diagnostic errors.
- Age of culture: Older bacterial cultures may lose cell wall integrity, leading to inconsistent staining (e.g., Gram-variable results).
- Technical error: Poor smear preparation or incorrect timing can distort results.
- Atypical organisms: Some bacteria, like mycobacteria or mycoplasmas, do not stain reliably with the Gram method due to unique cell wall structures.
- Mixed infections: Samples containing both Gram-positive and Gram-negative species require careful interpretation to avoid overlooking one population.
Mini Case Study: A Misdiagnosed Urinary Tract Infection
A 68-year-old woman presented with dysuria and urgency. A urine dipstick showed leukocyte esterase and nitrites. A Gram stain of the uncentrifuged sample revealed numerous white blood cells and many Gram-negative rods, suggesting E. coli. However, the lab technician noted occasional Gram-positive cocci in clusters. Suspecting contamination or mixed infection, they flagged the result.
Culture later confirmed both E. coli and Staphylococcus saprophyticus. Because the Gram stain was carefully interpreted—not assumed—the clinician treated with an agent effective against both organisms, preventing recurrence. This case underscores how attention to detail in staining can alter treatment pathways.
Frequently Asked Questions
Can the Gram stain identify bacteria to the species level?
No, the Gram stain only provides morphological and staining characteristics (e.g., Gram-positive cocci in chains). Species-level identification requires culture, biochemical testing, or molecular methods like PCR or MALDI-TOF.
Why do some bacteria stain Gram-variable?
Some species, like Actinomyces or Bacillus in older cultures, show inconsistent staining due to uneven cell wall degradation or incomplete peptidoglycan cross-linking. This leads to mixed purple and pink cells in the same field.
Is the Gram stain still relevant in the age of rapid diagnostics?
Absolutely. While technologies like PCR and antigen tests offer speed, the Gram stain remains low-cost, widely accessible, and immediately informative. It continues to be a frontline tool in resource-limited and high-acuity settings alike.
Checklist: Best Practices for Accurate Gram Staining
- Prepare a thin, even bacterial smear on a clean slide.
- Heat-fix properly to prevent washing away during staining.
- Follow reagent application times precisely—especially decolorization.
- Use fresh reagents; degraded crystal violet or safranin reduces contrast.
- Examine slides promptly under oil immersion with proper lighting.
- Correlate findings with clinical context and culture results.
- Document morphology (cocci, bacilli), arrangement (clusters, chains), and staining quality.
Conclusion: Mastering a Foundational Tool
The Gram stain endures not because it is flashy, but because it is functional. As a differential stain, it transforms invisible microbes into interpretable visual data, enabling swift decisions in both clinical and laboratory environments. Its power lies in simplicity—four reagents, four steps, and a world of insight.
Whether you're a student learning bacteriology, a clinician interpreting lab results, or a researcher characterizing isolates, mastering the Gram stain means mastering the language of microbial structure. By respecting its principles and recognizing its limits, you equip yourself with one of microbiology’s most enduring tools.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?