Since its emergence in the 1980s, HIV has claimed over 40 million lives worldwide. While antiretroviral therapy (ART) has transformed HIV from a fatal diagnosis into a manageable chronic condition, a true cure remains elusive. Millions live with the virus under control but not eradicated. The question persists: why, after decades of research and billions in funding, is HIV still incurable? The answer lies in the virus’s unique biology, its ability to hide, and the limitations of current medical science.
The Nature of HIV: A Master of Evasion
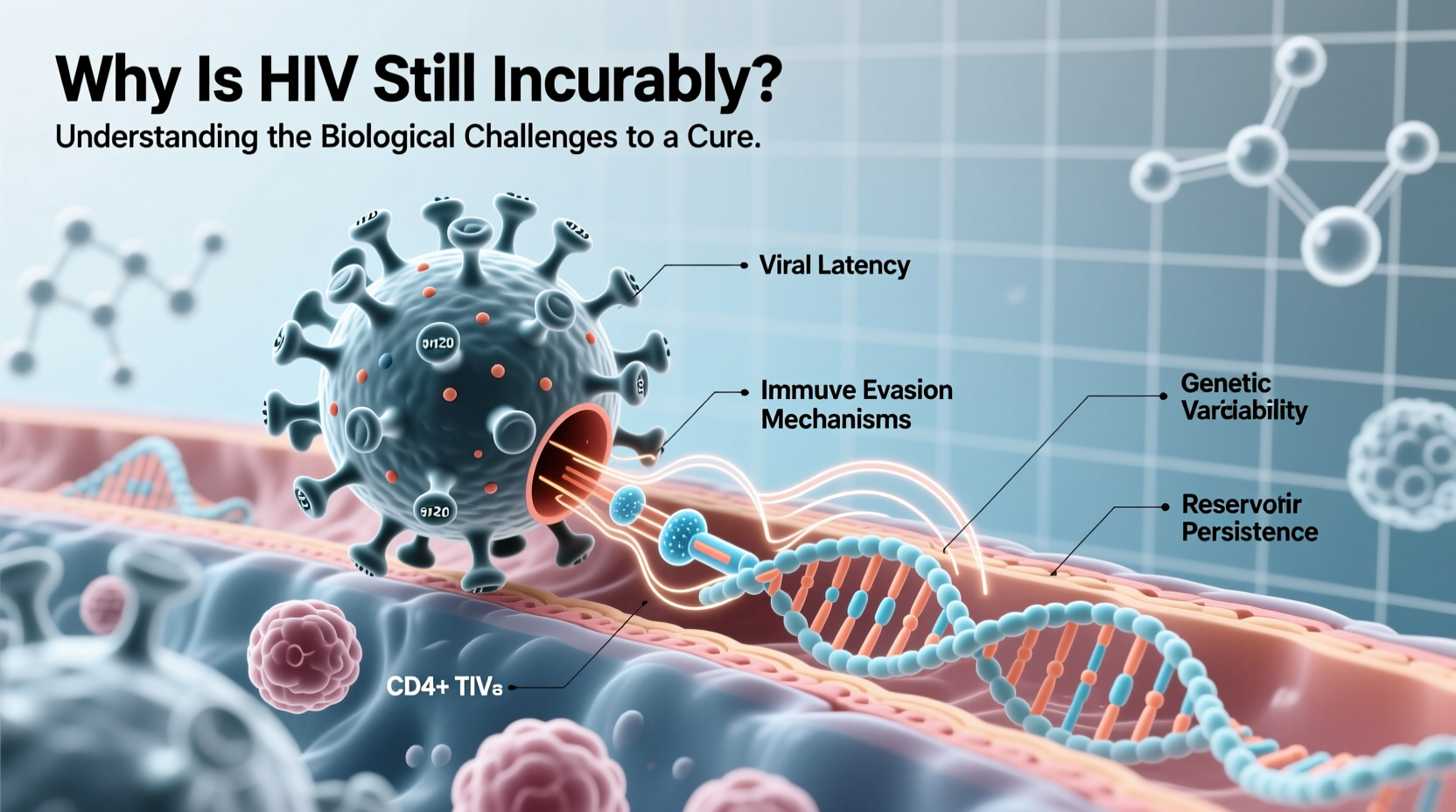
HIV, or human immunodeficiency virus, targets the very cells designed to defend the body—CD4+ T cells, crucial components of the immune system. Once inside these cells, HIV integrates its genetic material into the host’s DNA, turning the cell into a factory for new viral particles. This integration is central to why HIV is so difficult to eliminate.
Unlike many viruses that remain extracellular or replicate independently, HIV becomes part of the human genome. When antiretroviral drugs suppress active replication, they do not touch this integrated proviral DNA. As long as it remains hidden within long-lived immune cells, the virus can reactivate at any time if treatment stops.
“HIV doesn’t just infect the immune system—it becomes part of it. That’s what makes a sterilizing cure so challenging.” — Dr. Anthony Fauci, Former Director, National Institute of Allergy and Infectious Diseases
Viral Reservoirs: The Hidden Sanctuaries
One of the biggest barriers to curing HIV is the existence of viral reservoirs—pockets of cells where the virus lies dormant, invisible to both the immune system and antiretroviral drugs. These reservoirs form early in infection, often within days of exposure.
The most well-studied reservoirs include memory CD4+ T cells, which are designed to persist for years to provide long-term immunity. Unfortunately, when HIV hijacks these cells, it gains a long-term hiding place. Other potential reservoirs exist in the brain, gut-associated lymphoid tissue, and bone marrow, making them difficult to access even with advanced therapies.
Challenges in Targeting Latent Virus
Latency is HIV’s most effective survival strategy. In latent infection, the virus does not produce proteins or new particles, rendering it invisible to immune surveillance and unaffected by drugs that target active replication.
Researchers have explored the “shock and kill” strategy: using latency-reversing agents (LRAs) to “wake up” the dormant virus so it can be eliminated by the immune system or antiretrovirals. However, clinical trials have shown limited success. Many LRAs fail to activate all reservoirs, and some trigger dangerous levels of inflammation without clearing significant virus.
Another issue is specificity. Activating HIV in reservoirs without triggering widespread immune activation or damaging healthy cells remains a major hurdle. Moreover, not all proviruses are capable of producing infectious virus—many are defective—but they still complicate detection and clearance efforts.
Immune System Exhaustion and Escape
Even if the virus is exposed, the immune system often fails to eliminate it. Chronic HIV infection leads to T-cell exhaustion, where immune cells become dysfunctional and less responsive. Additionally, HIV mutates rapidly, allowing it to escape recognition by antibodies and cytotoxic T cells.
Vaccine development has been stymied by this variability. Unlike viruses such as measles or polio, which have stable surface proteins, HIV’s envelope glycoprotein (gp160) is highly mutable and shielded by sugar molecules, making it a moving target for vaccines and immune responses.
Natural immunity rarely controls HIV without medication. Only a tiny fraction of people—called elite controllers—can suppress the virus naturally, usually due to specific genetic factors like the HLA-B*57 mutation. Understanding these individuals offers clues, but replicating their immune response therapeutically has proven difficult.
| Factor | Impact on Cure Efforts |
|---|---|
| Genomic Integration | Makes virus permanent in host DNA; hard to excise safely |
| Latent Reservoirs | Hide virus from drugs and immune system |
| Rapid Mutation | Enables immune escape and drug resistance |
| Early Reservoir Seeding | Reservoirs form before diagnosis in most cases |
| Lack of Biomarkers | No reliable way to measure reservoir size or activity |
Promising Research and Alternative Strategies
Despite setbacks, several innovative approaches are being tested:
- Gene Editing: Technologies like CRISPR-Cas9 aim to cut HIV DNA out of infected cells. Early animal studies show promise, but off-target effects and delivery challenges remain.
- Therapeutic Vaccines: Designed to boost immune control of HIV, potentially allowing patients to stay off ART.
- Broadly Neutralizing Antibodies (bNAbs): These lab-engineered antibodies target conserved regions of HIV and have shown ability to suppress the virus in some trials.
- Stem Cell Transplants: The only documented cures—such as the “Berlin” and “London” patients—involved stem cell transplants from donors with a CCR5-delta32 mutation, which blocks HIV entry. However, this approach is too risky and impractical for widespread use.
A functional cure—one where HIV remains in the body but is controlled without daily medication—is now considered more achievable than a sterilizing cure (complete eradication). Achieving sustained remission, even without eliminating every viral fragment, could transform how we manage HIV.
Mini Case Study: The London Patient
In 2019, Adam Castillejo, known as the “London patient,” became the second person ever declared cured of HIV. He received a stem cell transplant to treat Hodgkin’s lymphoma from a donor with the rare CCR5-delta32 mutation. After stopping ART, no active virus was detected for over five years. His case confirmed that curing HIV is possible—but also highlighted the limitations: the procedure carries high mortality risk and is unsuitable for otherwise healthy individuals. Still, his recovery fuels research into gene therapies that mimic this natural resistance.
Step-by-Step: The Scientific Path Toward a Cure
- Identify and quantify reservoirs using sensitive assays to understand where and how much virus persists.
- Reactivate latent virus with safe and effective latency-reversing agents.
- Enhance immune clearance through vaccines, bNAbs, or engineered T cells.
- Prevent reseeding of reservoirs during therapy with potent antivirals.
- Monitor long-term remission after treatment interruption to confirm durability.
Frequently Asked Questions
Can ART cure HIV?
No. Antiretroviral therapy suppresses HIV replication and reduces viral load to undetectable levels, but it does not eliminate the integrated provirus in reservoirs. If treatment stops, the virus typically rebounds within weeks.
Why can’t the immune system clear HIV on its own?
HIV directly attacks CD4+ T cells, weakens immune coordination, and rapidly mutates to evade detection. It also establishes latency, hiding from immune surveillance. Over time, chronic activation exhausts immune responses, making clearance impossible without intervention.
Are there any people who naturally cure themselves of HIV?
There are no confirmed cases of natural sterilizing cure. However, about 0.5% of people are “elite controllers” who maintain undetectable viral loads without medication due to favorable genetics. Researchers are studying them to inform cure strategies.
Checklist: What’s Needed for an HIV Cure?
- ✔️ Safe methods to eliminate or silence viral reservoirs
- ✔️ Therapies that enhance immune recognition of HIV
- ✔️ Gene-editing tools with high precision and low off-target risk
- ✔️ Biomarkers to measure reservoir activity and cure progress
- ✔️ Global access strategies to ensure equitable distribution of any future cure
Conclusion: The Road Ahead
While HIV remains incurable for the vast majority, scientific progress continues to chip away at the barriers. The complexity of the virus demands equally sophisticated solutions—combining gene therapy, immunology, and pharmacology. The few documented cures prove that eradication is biologically possible, offering hope for scalable alternatives.
A cure may not come in the form of a single breakthrough, but through incremental advances that one day allow people with HIV to live free of medication, stigma, and fear of transmission. Until then, expanding access to treatment, prevention, and education remains critical. The pursuit of a cure isn’t just a scientific mission—it’s a global health imperative.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?