For many couples, starting a family feels like a natural next step. Yet for some, conception doesn’t happen as quickly as expected. While occasional delays are normal, persistent difficulty can signal underlying fertility challenges. Understanding why it’s hard to get pregnant—biologically, emotionally, and medically—is the first step toward effective solutions. This article explores the most common causes of infertility, signs that warrant medical evaluation, and practical actions you can take to improve your chances.
How Long Does It Usually Take to Get Pregnant?
About 85% of couples conceive within one year of trying, with roughly half succeeding within the first three months. Timing intercourse around ovulation significantly increases odds, but even under ideal conditions, pregnancy isn't guaranteed each cycle. Factors like age, overall health, and reproductive history influence timelines.
Fertility declines gradually after age 30 and more sharply after 35. For women under 35, doctors typically recommend waiting a full year before investigating fertility issues. For those over 35, that window shortens to six months due to declining egg quality and quantity.
Common Medical Causes of Infertility
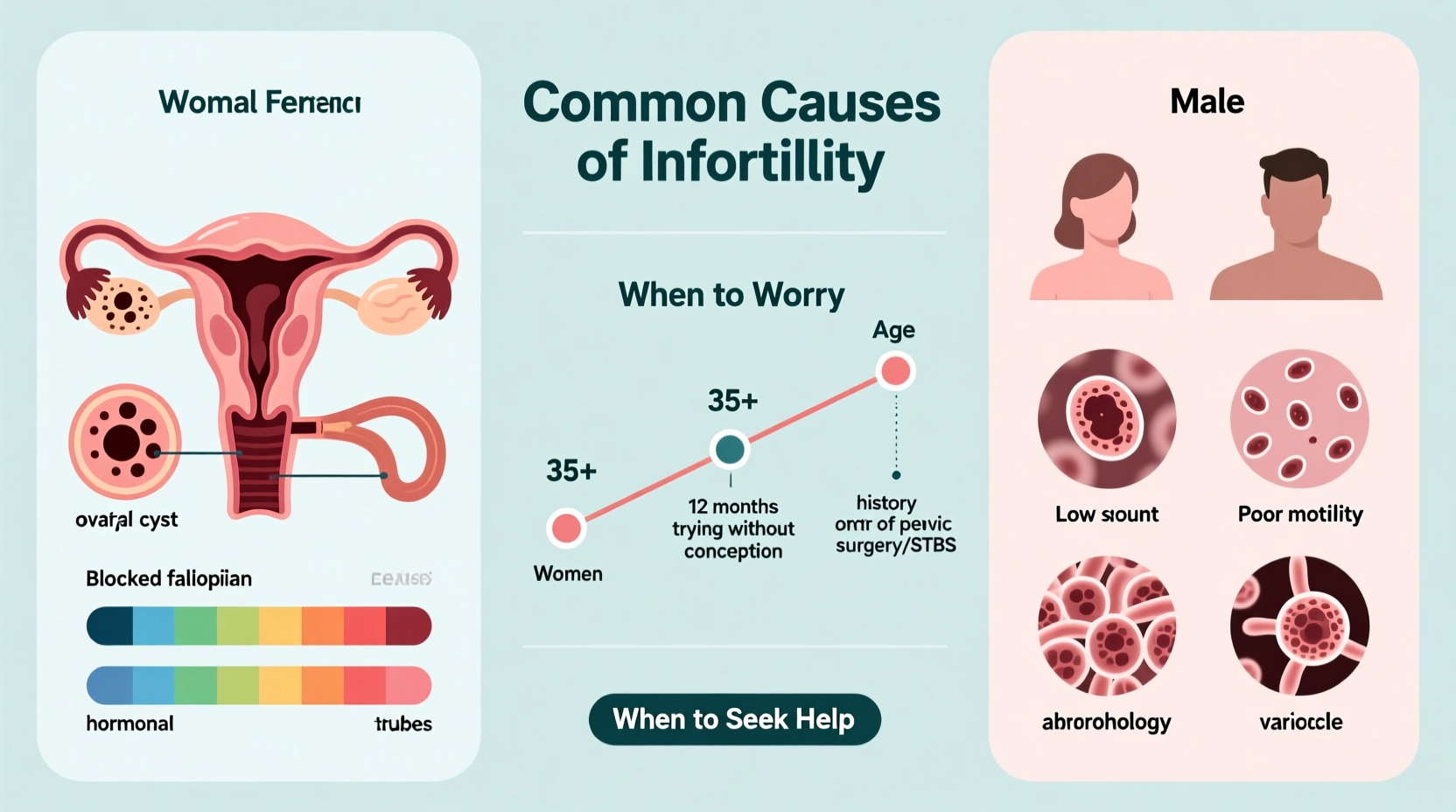
Infertility is defined as the inability to conceive after one year of regular, unprotected sex (or six months if over 35). It affects about 1 in 6 couples globally. Causes can stem from male factors, female factors, or a combination of both.
Female Factor Infertility
- Ovulatory disorders: Polycystic ovary syndrome (PCOS), hypothalamic dysfunction, and premature ovarian insufficiency disrupt regular egg release.
- Tubal blockages: Infections like pelvic inflammatory disease (PID) or prior surgeries can damage or block fallopian tubes.
- Endometriosis: A condition where uterine-like tissue grows outside the uterus, causing inflammation, scarring, and impaired implantation.
- Uterine or cervical abnormalities: Fibroids, polyps, or structural anomalies may interfere with embryo implantation or sperm passage.
- Age-related decline: Egg quantity and quality diminish significantly after 35, increasing miscarriage risk and lowering conception odds.
Male Factor Infertility
- Low sperm count or motility: Affects nearly 40% of infertile men. Lifestyle, genetics, and environmental exposures play roles.
- Sperm morphology: Abnormally shaped sperm have reduced fertilization capacity.
- Hormonal imbalances: Issues with testosterone, FSH, or prolactin can impair sperm production.
- Varicoceles: Enlarged veins in the scrotum increase testicular temperature, harming sperm development.
- Obstructions or genetic conditions: Blockages from infections or congenital defects like cystic fibrosis mutations prevent sperm delivery.
“Up to half of infertility cases involve a male factor, yet men are often overlooked in initial evaluations.” — Dr. Alan Copperman, Reproductive Endocrinologist
When to Worry: Red Flags That Warrant Evaluation
While patience is important, certain symptoms suggest earlier intervention. Don’t wait a full year if you experience any of the following:
- Irregular or absent periods
- Painful menstruation or intercourse (possible endometriosis)
- History of pelvic infections or sexually transmitted diseases
- Known PCOS, thyroid disorders, or other hormonal conditions
- Previous cancer treatments involving chemotherapy or radiation
- Recurrent miscarriages (two or more)
- Male partner with known low sperm count or testicular injury
Couples over 35 should consult a specialist after six months of trying—or sooner if red flags are present. Early assessment can prevent delays in treatment and preserve options, especially for women with limited ovarian reserve.
Action Plan: Steps to Improve Fertility Naturally and Medically
Whether preparing for conception or addressing diagnosed infertility, proactive steps can make a meaningful difference.
Step-by-Step Guide to Optimizing Fertility
- Track ovulation: Use basal body temperature charts, ovulation predictor kits, or fertility apps to time intercourse effectively.
- Adopt a fertility-friendly diet: Emphasize whole grains, leafy greens, lean proteins, and healthy fats. Reduce trans fats and refined sugars.
- Maintain a healthy weight: Both underweight and overweight states disrupt hormone balance and ovulation.
- Limit alcohol and avoid smoking: These reduce fertility in both partners and increase miscarriage risk.
- Reduce stress: Chronic stress alters cortisol and reproductive hormones. Mindfulness, yoga, and therapy can help.
- Get tested: Request semen analysis for men and hormonal panels, ultrasound, and HSG (hysterosalpingogram) for women when indicated.
- Seek specialist care: A reproductive endocrinologist can guide treatments like Clomid, IUI, or IVF based on diagnosis.
| Factor | Do’s | Avoid |
|---|---|---|
| Diet | Eat antioxidant-rich foods (berries, nuts, spinach) | Excess caffeine (>300mg/day), processed foods |
| Exercise | Moderate activity (30 min/day, most days) | Extreme endurance training |
| Sexual Frequency | Every 2–3 days during fertile window | Infrequent or excessive intercourse |
| Environmental Exposure | Use BPA-free containers, natural cleaning products | Pesticides, plastics, heavy metals |
Real Example: Navigating Unexplained Infertility
Sarah and James tried for 14 months without success. Both were healthy, nonsmokers, and had regular cycles. Initial tests showed normal hormone levels and open fallopian tubes. A semen analysis revealed slightly low motility, but not enough to explain the delay. Their diagnosis: unexplained infertility.
Their doctor recommended timed intercourse with Clomid and intrauterine insemination (IUI). After two cycles, Sarah became pregnant and gave birth to a healthy baby boy. Their story highlights that even without a clear cause, structured interventions can lead to success.
Frequently Asked Questions
Can stress really prevent pregnancy?
While everyday stress is unlikely to cause infertility, chronic, severe stress may disrupt ovulation and sexual function. Managing emotional health supports overall reproductive wellness—even if it doesn’t guarantee conception.
Does having regular periods mean I’m fertile?
Not necessarily. Regular cycles suggest ovulation is likely, but they don’t confirm egg quality, tubal patency, or sperm compatibility. Some women with regular periods struggle with endometriosis or diminished ovarian reserve.
What’s the success rate of fertility treatments?
It varies by age and treatment type. For women under 35, IVF success rates per cycle range from 40–50%. These drop to around 10–15% for women over 40. Early intervention improves outcomes across all modalities.
Conclusion: Taking Charge of Your Fertility Journey
Difficulty getting pregnant is more common than many realize—and rarely a reflection of personal failure. Biological, lifestyle, and timing factors all play roles. The key is awareness: knowing when to act, what questions to ask, and how to advocate for thorough evaluation. Whether through natural optimization or medical support, most couples find paths to parenthood with persistence and proper guidance.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?