Difficulty passing stool is a surprisingly common issue that affects millions of people worldwide. While occasional constipation is normal, persistent trouble with bowel movements can disrupt daily life and signal underlying health concerns. The sensation of incomplete evacuation, straining, or infrequent bowel movements often leads to discomfort and frustration. Understanding the root causes—and knowing what steps to take—can make a significant difference in restoring digestive comfort and regularity.
Understanding Bowel Function and Constipation
The human digestive system relies on coordinated muscle contractions, adequate hydration, and dietary fiber to move waste through the colon efficiently. When this process slows down, stool becomes dry and hard, making it difficult to pass. Medically, constipation is typically defined as having fewer than three bowel movements per week, though individual patterns vary. What matters most is consistency and ease—not just frequency.
Chronic difficulty with defecation may stem from lifestyle habits, medical conditions, medications, or even psychological factors. Ignoring the urge to go, insufficient water intake, or a low-fiber diet are among the most common culprits. Over time, these behaviors can weaken the body’s natural signals and lead to a cycle of worsening symptoms.
Common Causes of Difficulty Pooping
Several interrelated factors contribute to the struggle of passing stool. Identifying which apply can help tailor an effective solution.
- Dietary Deficiencies: A lack of fiber from fruits, vegetables, whole grains, and legumes reduces stool bulk and slows transit time.
- Dehydration: Insufficient fluid intake causes the colon to absorb more water from stool, resulting in hard, dry feces.
- Sedentary Lifestyle: Physical inactivity slows intestinal motility, reducing the efficiency of digestion.
- Medications: Opioids, certain antidepressants, antacids containing aluminum or calcium, and iron supplements are known to cause constipation.
- Irritable Bowel Syndrome (IBS): IBS-C (constipation-predominant) involves abdominal pain and altered bowel habits due to gut-brain axis dysfunction.
- Pelvic Floor Dysfunction: Incoordination of pelvic muscles during defecation can block stool passage despite normal motility.
- Hormonal Imbalances: Conditions like hypothyroidism, diabetes, and pregnancy affect nerve signaling and muscle contractions in the gut.
“Many patients come in frustrated, thinking they’re doing everything right—but small overlooked habits like chronic delaying or inadequate water intake can be the real issue.” — Dr. Lena Torres, Gastroenterologist
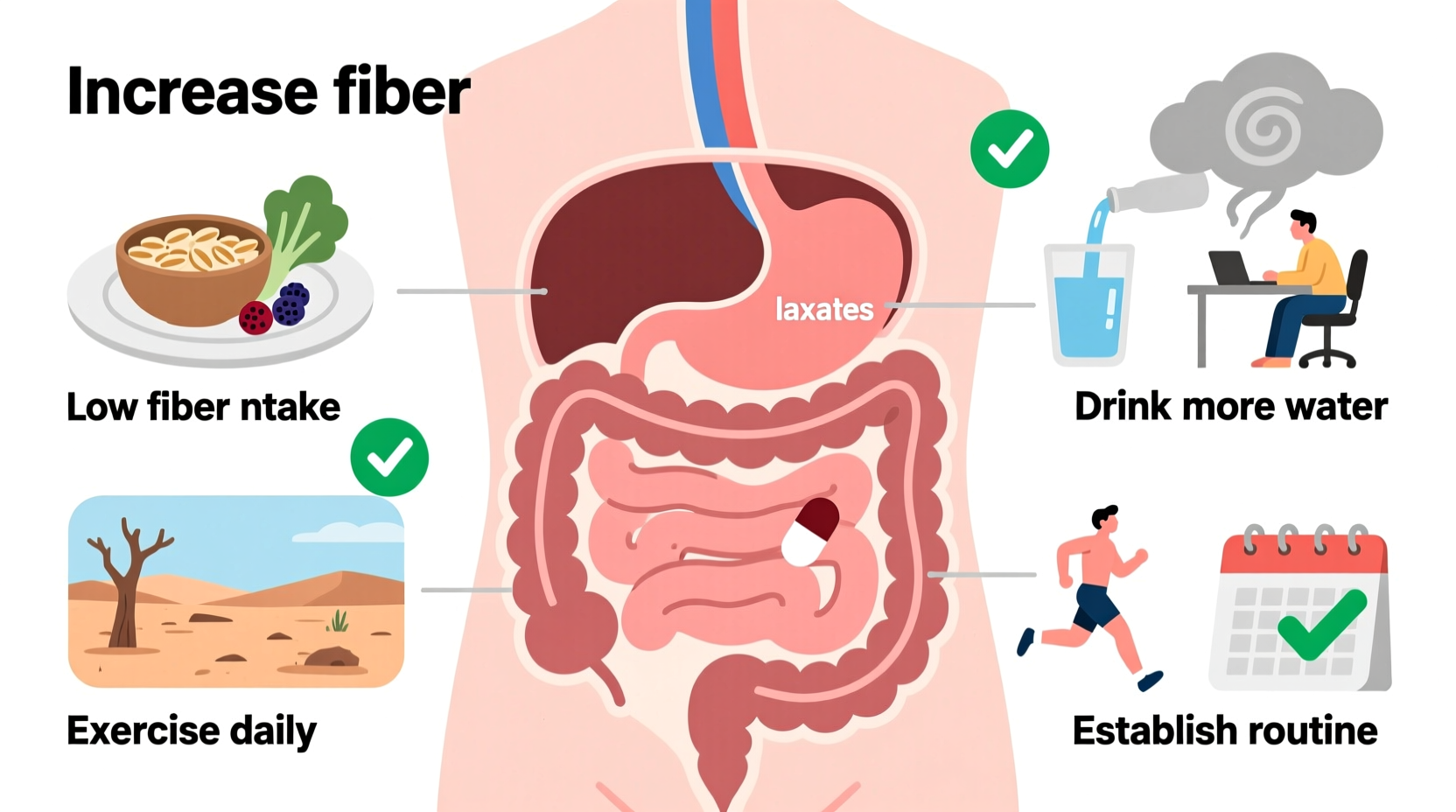
Practical Relief Tips for Easier Bowel Movements
Addressing constipation effectively requires both immediate relief strategies and long-term habit changes. Most cases improve significantly with consistent lifestyle adjustments.
Hydration and Diet Optimization
Increase daily water intake—aim for at least 1.5 to 2 liters unless restricted by a medical condition. Pair this with a high-fiber diet rich in oats, beans, berries, leafy greens, and chia seeds. Gradually increase fiber to avoid bloating.
Physical Activity
Regular movement—such as walking, cycling, or yoga—encourages intestinal contractions. Even 20 minutes of moderate exercise daily can enhance bowel regularity.
Bowel Positioning
Modern toilets force a near-upright posture that can kink the rectum. Using a small footstool to elevate your knees above your hips mimics a squatting position, straightening the anorectal angle and easing stool passage.
| Tactic | How It Helps | Recommended Frequency |
|---|---|---|
| High-fiber diet | Adds bulk and softness to stool | Daily (25–30g fiber) |
| Adequate hydration | Prevents stool dehydration | 6–8 glasses/day |
| Walking after meals | Stimulates digestive motility | 15–30 minutes, 1–2x daily |
| Morning routine | Leverages natural circadian bowel rhythm | Same time each day |
Step-by-Step Guide to Restoring Regularity
Follow this five-day plan to reset your digestive rhythm:
- Day 1: Assess current habits—track food, water, and bathroom attempts. Note delays in responding to urges.
- Day 2: Increase water intake and add one high-fiber meal (e.g., oatmeal with fruit).
- Day 3: Begin a daily 20-minute walk, preferably after breakfast.
- Day 4: Introduce a footstool when using the toilet to improve positioning.
- Day 5: Establish a set time each morning to sit on the toilet for 5–10 minutes, even without urgency, to train the body.
Consistency over weeks yields better results than short-term fixes. If no improvement occurs within two weeks, consider professional evaluation.
When to Seek Medical Help
While most constipation responds to lifestyle changes, some signs warrant prompt medical attention:
- New-onset constipation lasting more than three weeks
- Unintentional weight loss
- Blood in stool
- Severe abdominal pain or bloating
- Family history of colon cancer or inflammatory bowel disease
A healthcare provider may perform tests such as blood work, thyroid function panels, or imaging studies. For suspected pelvic floor dysfunction, biofeedback therapy has shown strong efficacy in retraining muscle coordination.
Real-Life Example: Sarah’s Experience
Sarah, a 38-year-old office worker, struggled with infrequent and painful bowel movements for months. She drank little water, ate mostly processed foods, and routinely ignored the urge to go while at work. After consulting her doctor, she implemented simple changes: carrying a reusable water bottle, eating a fiber-rich breakfast, and using a footstool at home. Within ten days, her bowel movements became more regular and less strained. “I didn’t realize how much my desk job was affecting my digestion,” she said. “Now I schedule bathroom breaks like meetings—it’s made all the difference.”
Frequently Asked Questions
Can stress really affect my ability to poop?
Yes. Stress activates the sympathetic nervous system, which slows digestion and can suppress the urge to defecate. Chronic stress may contribute to functional gastrointestinal disorders like IBS.
Are laxatives safe for long-term use?
Not all laxatives are meant for extended use. Bulk-forming types (like psyllium) are generally safe daily. Stimulant laxatives (e.g., senna) should be limited to short-term use to avoid dependency. Always consult a doctor before prolonged use.
Is it normal to strain occasionally?
Minor straining now and then is not unusual, especially after large meals. However, regular or excessive straining may indicate constipation, pelvic floor issues, or hemorrhoids and should be evaluated.
Final Thoughts and Action Steps
Difficulty pooping is rarely due to a single cause—it's usually the result of multiple overlapping habits and conditions. The good news is that most people can find relief through mindful changes to diet, hydration, movement, and bathroom routines. Prevention is far more effective than crisis management. Start small: drink more water today, eat a piece of fruit with lunch, or try sitting on a footstool tomorrow morning. These incremental steps build momentum toward lasting digestive wellness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?