Waking up with puffy eyes, noticing tight rings that no longer slide easily over your fingers, or feeling heaviness in your legs by the end of the day can be unsettling. Swelling in the body—commonly known as edema—is more than just a cosmetic concern. It’s often a signal from your body that something is off-balance. While mild swelling can result from prolonged sitting or salty meals, persistent or widespread edema may point to underlying health conditions. Understanding the mechanisms behind fluid retention, recognizing the warning signs, and knowing when to act are essential steps toward better health.
What Is Edema and How Does It Work?
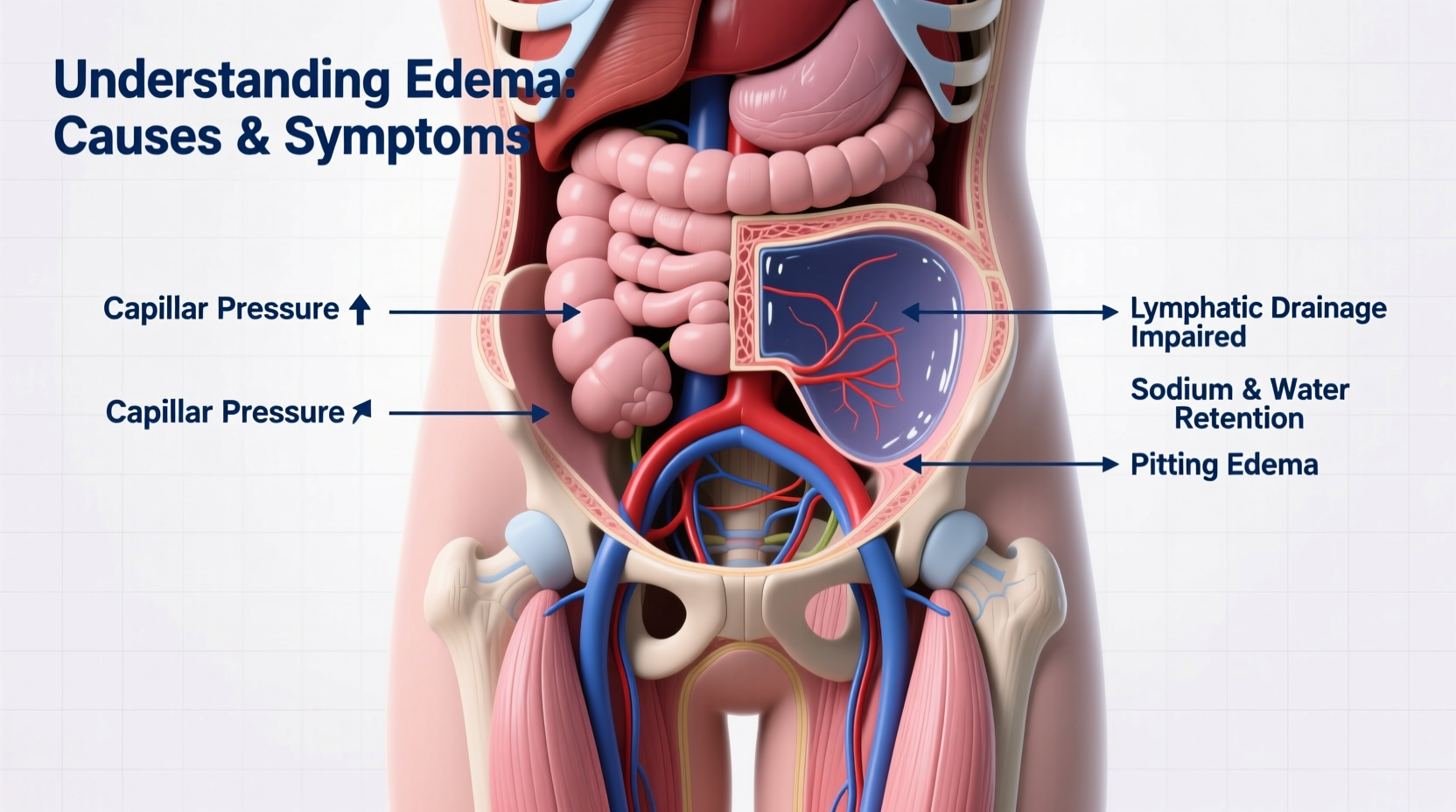
Edema occurs when excess fluid becomes trapped in the body's tissues, leading to visible swelling. This fluid typically leaks out of small blood vessels into surrounding tissues due to imbalances in hydrostatic pressure, osmotic pressure, or capillary permeability. The most common areas affected include the feet, ankles, legs, hands, and face, though edema can occur anywhere in the body—even internally, such as in the lungs (pulmonary edema) or abdomen (ascites).
The human circulatory system maintains a delicate equilibrium between fluid pushed out of blood vessels and fluid reabsorbed back into them. When this balance is disrupted—by heart failure, kidney disease, liver dysfunction, or inflammation—the result is fluid accumulation. Inflammation-induced edema, for example, involves increased capillary permeability, allowing proteins and fluids to leak into tissues, causing localized swelling after injury or infection.
Common Causes of Body Swelling
Edema isn’t a standalone illness but rather a symptom of various physiological disruptions. Identifying the root cause is crucial for effective treatment. Below are some of the most frequent contributors:
- Heart Failure: When the heart can't pump efficiently, blood backs up in the veins, increasing pressure and forcing fluid into tissues—especially in the lower extremities.
- Kidney Disease: Impaired kidney function reduces the body’s ability to eliminate sodium and water, leading to generalized swelling, particularly around the eyes and legs.
- Liver Cirrhosis: Low albumin production due to liver damage decreases oncotic pressure, promoting fluid leakage into the abdominal cavity (ascites) and limbs.
- Pregnancy: Hormonal changes and increased blood volume can cause mild edema, especially in the third trimester. However, sudden swelling may indicate preeclampsia.
- Medications: Certain drugs—including NSAIDs, calcium channel blockers, steroids, and some diabetes medications—can trigger fluid retention.
- Chronic Venous Insufficiency: Damaged valves in leg veins hinder blood flow back to the heart, resulting in pooling and leg swelling.
- Lymphedema: Blockage or removal of lymph nodes (often after cancer treatment) impairs lymphatic drainage, causing chronic limb swelling.
“Persistent edema should never be ignored. It’s the body’s way of signaling deeper issues—sometimes silent ones like early heart or kidney disease.” — Dr. Alan Reyes, Nephrologist and Internal Medicine Specialist
Symptoms and Warning Signs to Watch For
Swelling itself is the primary sign of edema, but accompanying symptoms provide critical clues about its origin and severity. Mild edema may only cause puffiness and a feeling of tightness, while severe cases can impair mobility and lead to skin changes.
| Symptom | Possible Cause | When to Seek Help |
|---|---|---|
| Pitting edema (skin retains indentation when pressed) | Systemic fluid overload (heart, kidney, liver) | If persistent beyond 24 hours or worsening |
| Sudden facial or eye swelling | Allergic reaction, kidney issues | Immediate attention if breathing is affected |
| Shortness of breath with leg swelling | Heart failure, pulmonary edema | Emergency care required |
| Unilateral leg swelling + pain | Deep vein thrombosis (DVT) | Urgent evaluation needed |
| Tight, shiny skin or ulcers | Chronic venous insufficiency or lymphedema | See vascular specialist |
Mini Case Study: Recognizing Silent Heart Failure
Susan, a 62-year-old office worker, began noticing her shoes felt tighter by midday. She dismissed it as weight gain until she developed shortness of breath climbing stairs. A routine check-up revealed mild ankle edema and elevated jugular venous pressure. Further testing confirmed early-stage heart failure. With medication and lifestyle adjustments—including reduced salt intake and daily walking—Susan’s swelling improved significantly within weeks. Her case illustrates how subtle edema can be an early red flag for serious cardiovascular issues.
Diagnosis and Medical Evaluation
Doctors assess edema through physical exams, patient history, and diagnostic tests. During evaluation, they determine whether the edema is pitting or non-pitting, unilateral or bilateral, and localized or systemic. Blood tests (e.g., BNP, creatinine, liver enzymes), urine analysis, chest X-rays, echocardiograms, and ultrasound scans help pinpoint underlying causes.
A stepwise approach is often used:
- History and Physical Exam: Assess duration, pattern, associated symptoms, medications, and comorbidities.
- Laboratory Testing: Check kidney, liver, and heart function.
- Imaging: Echocardiogram for heart function; Doppler ultrasound for DVT.
- Differentiation: Rule out life-threatening causes like pulmonary edema or DVT before managing chronic cases.
Practical Steps to Manage and Reduce Swelling
While treating the underlying condition is paramount, several lifestyle strategies can help manage mild to moderate edema:
- Reduce dietary sodium intake—aim for less than 2,300 mg per day (ideally 1,500 mg for those with heart or kidney concerns).
- Stay physically active—movement promotes circulation and lymphatic drainage.
- Avoid prolonged standing or sitting; take breaks to stretch or elevate your legs.
- Wear compression stockings if recommended for venous insufficiency or lymphedema.
- Limit alcohol and avoid smoking, both of which impair circulation and organ function.
Checklist: Daily Habits to Reduce Fluid Retention
- ✅ Weigh yourself daily at the same time to track sudden increases (more than 2 lbs overnight may signal fluid gain).
- ✅ Drink adequate water—dehydration can worsen fluid retention.
- ✅ Avoid processed foods high in hidden sodium.
- ✅ Perform gentle ankle circles and leg lifts throughout the day.
- ✅ Monitor blood pressure regularly if you have a history of hypertension or heart disease.
Frequently Asked Questions
Is it normal to have swollen feet after flying?
Yes, temporary swelling in the feet and ankles during or after long flights is common due to immobility and low cabin pressure. Walking every hour, staying hydrated, and wearing compression socks can minimize this. However, if swelling persists for days or is accompanied by pain or redness, consult a doctor to rule out deep vein thrombosis.
Can allergies cause body swelling?
Absolutely. Allergic reactions—especially to food, insect stings, or medications—can trigger angioedema, a type of rapid-onset swelling beneath the skin, often affecting the face, lips, and tongue. Unlike typical edema, angioedema is usually firm and non-pitting. Severe cases can obstruct airways and require emergency treatment with epinephrine.
Does drinking more water help reduce edema?
Counterintuitively, yes. When the body senses dehydration, it holds onto fluid. Consistent hydration supports kidney function and helps flush excess sodium, reducing overall fluid retention. Aim for clear to light-yellow urine as a sign of proper hydration.
Take Action Before Swelling Becomes Serious
Edema is more than just puffiness—it’s a physiological message worth listening to. While occasional swelling may resolve on its own, recurring or unexplained fluid retention demands attention. Early intervention can prevent complications like skin breakdown, infections, or progression of heart, kidney, or liver disease. Don’t wait for swelling to become severe. Track your symptoms, adjust your habits, and consult a healthcare provider if you’re unsure. Your body is speaking; the wisest response is to listen carefully and act with care.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?