If you’ve noticed persistent red bumps, small pimples, or irritated skin forming a ring around your mouth, you're not alone. This specific type of breakout — often clustered just above, below, or surrounding the lips — can be frustrating, especially when typical acne treatments don’t help. Unlike hormonal acne or blackheads on the forehead or chin, breakouts localized around the mouth may stem from different triggers, including skincare habits, oral hygiene products, or even underlying skin conditions.
Understanding what’s really causing this irritation is the first step toward clearing it up. The good news? Most cases respond well to targeted changes in routine and product use. Whether it's perioral dermatitis, folliculitis, or contact dermatitis, identifying the root cause allows for smarter, gentler interventions that restore skin balance without over-drying or worsening inflammation.
Common Causes of Breakouts Around the Mouth
The area around the mouth is particularly sensitive due to its high concentration of sebaceous glands and frequent exposure to irritants. Several factors can trigger or worsen breakouts here:
- Perioral Dermatitis: A common inflammatory condition characterized by clusters of tiny red papules or pustules around the mouth, often sparing the skin directly adjacent to the lips. It’s frequently linked to long-term use of topical steroids, heavy moisturizers, or fluoridated toothpaste.
- Irritating Skincare or Cosmetic Products: Heavy oils, silicones, or fragranced lotions applied near the mouth can clog pores or provoke irritation, especially if they migrate during talking or eating.
- Fluoride in Toothpaste: Sodium fluoride and flavoring agents (like mint or cinnamon) in many conventional toothpastes are known to trigger perioral dermatitis in sensitive individuals.
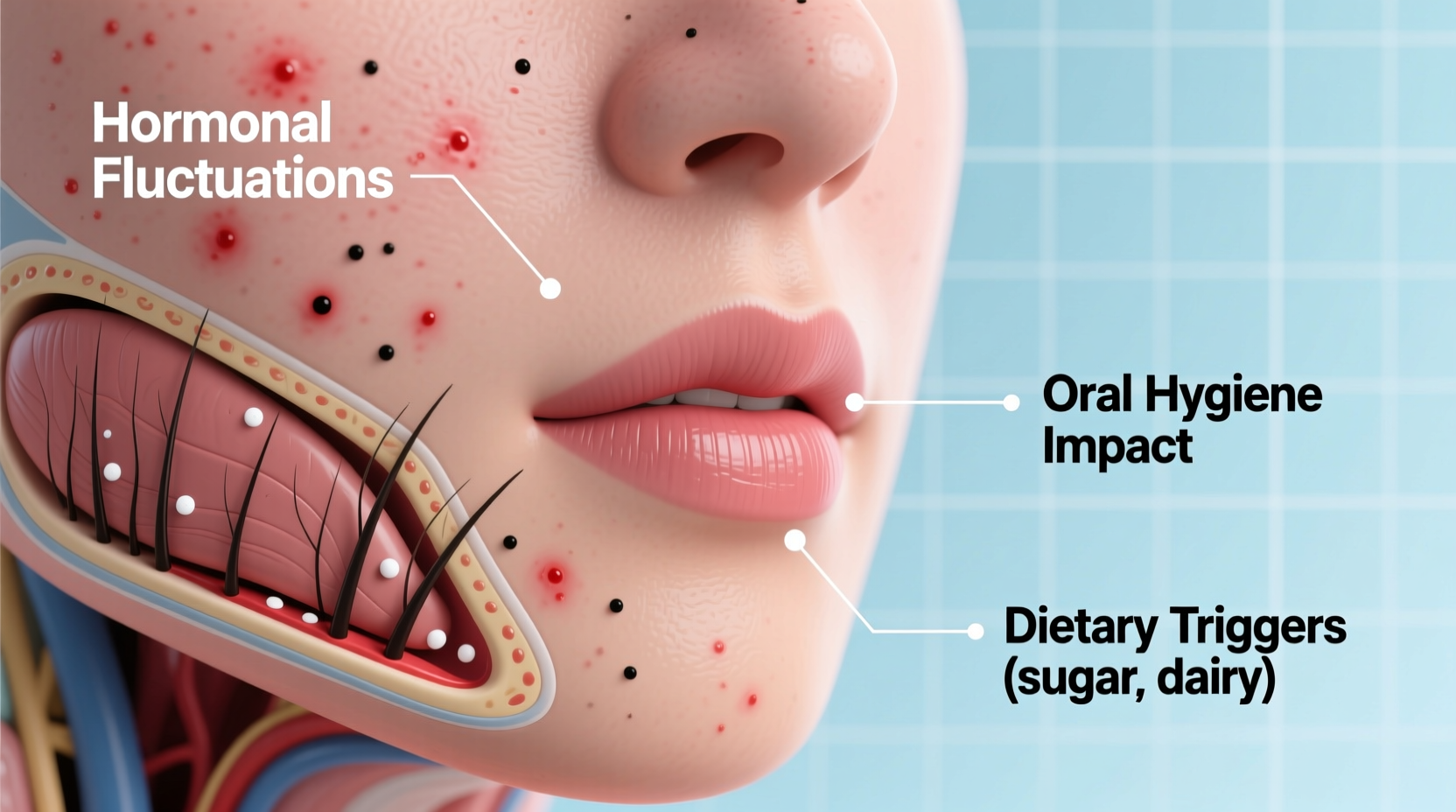
- Hormonal Fluctuations: While more commonly associated with jawline acne, hormonal shifts during menstruation, pregnancy, or PCOS can also manifest as breakouts near the mouth.
- Drooling or Lip Licking: Habitual lip licking moistens the area with saliva, which contains digestive enzymes that can irritate facial skin. Nighttime drooling can have a similar effect.
- Nasal Spray or Inhaler Use: Topical steroid sprays used for allergies or asthma may drip down into the facial creases and contribute to perioral dermatitis when not followed by proper cleansing.
- Bacterial or Fungal Folliculitis: Inflammation of hair follicles caused by bacteria (like *Staphylococcus*) or yeast (*Malassezia*) can appear as pimple-like lesions, especially after shaving or using contaminated makeup tools.
How to Identify What Type of Breakout You Have
Not all bumps around the mouth are the same. Accurate identification helps determine whether you need medical treatment or lifestyle adjustments.
| Type of Condition | Symptoms | Key Clues |
|---|---|---|
| Perioral Dermatitis | Small red bumps or pustules; dry, flaky skin; burning or itching | Spares the vermillion border (skin right next to lips); worsens with steroid creams |
| Folliculitis | Pimple-like bumps centered on hair follicles; sometimes painful | Often follows shaving; may improve with antiseptic washes |
| Contact Dermatitis | Redness, swelling, blistering, or peeling | Occurs shortly after using a new product; linked to fragrance or preservatives |
| Acne Mechanica | Comedones (blackheads/whiteheads), mild inflammation | Caused by friction (e.g., mask-wearing, phone use) |
| Cold Sores (Herpes Simplex) | Clusters of fluid-filled blisters; tingling before outbreak | Recurrent; typically on lip edge, not around it |
“Many patients come in thinking they have stubborn acne, but once we eliminate potential irritants like fluoridated toothpaste or heavy facial oils, their symptoms resolve within weeks.” — Dr. Lena Patel, Board-Certified Dermatologist
Simple Fixes and Lifestyle Adjustments That Work
Before reaching for prescription medication, try making these evidence-based changes. Many people see significant improvement within two to four weeks.
Switch to Fluoride-Free Toothpaste
Fluoride is a known trigger for perioral dermatitis. Try switching to a natural, fluoride-free toothpaste for at least three weeks. Look for brands free of sodium lauryl sulfate (SLS), artificial flavors, and dyes. Monitor any reduction in redness or new bump formation.
Revise Your Skincare Routine
Heavy moisturizers, sunscreen, or lip balm containing petroleum, beeswax, or lanolin can accumulate in the folds around the mouth. Replace them with lightweight, non-comedogenic alternatives. Avoid applying products too close to the mouth corners.
Stop Using Topical Steroid Creams
If you've been using hydrocortisone or other steroid creams on facial breakouts—even occasionally—discontinue use immediately. These can worsen perioral dermatitis over time, leading to rebound flare-ups.
Keep the Area Dry and Clean
Wipe away excess saliva after meals or workouts. If you wear masks frequently, change them regularly and cleanse your face afterward. Moisture buildup promotes bacterial growth and irritation.
Change Pillowcases Frequently
Use clean cotton pillowcases every 2–3 days. Oils, bacteria, and residual toothpaste from nighttime drooling can transfer back onto your skin while you sleep.
Step-by-Step Recovery Plan (4-Week Timeline)
Follow this structured plan to reduce inflammation and prevent recurrence:
- Week 1: Eliminate Triggers
Switch to fluoride-free toothpaste. Stop using heavy creams, lip balms, or steroid ointments. Wash face twice daily with a gentle, fragrance-free cleanser. - Week 2: Simplify Skincare
Use only a mild cleanser and a light, oil-free moisturizer (if needed). Avoid exfoliants, retinoids, or acids near the mouth. Pat skin dry—don’t rub. - Week 3: Monitor Progress
Take daily notes or photos. If redness decreases and no new bumps form, continue the regimen. If irritation persists, consider an over-the-counter antifungal cream (like clotrimazole) if yeast is suspected. - Week 4: Reintroduce Cautiously (Optional)
If healed, slowly reintroduce one product at a time—wait 5–7 days between additions. Watch for reactions. Never return to steroid creams unless prescribed by a doctor.
“A minimalist approach often works best. I tell my patients: less is more when treating perioral breakouts.” — Dr. Marcus Tran, Clinical Dermatology Advisor
When to See a Doctor
While many cases improve with self-care, some require professional diagnosis and treatment. Seek medical advice if:
- The rash spreads to the nose, eyes, or cheeks.
- There’s intense burning, pain, or oozing.
- Over-the-counter changes show no improvement after 4 weeks.
- You experience recurrent episodes despite preventive measures.
A dermatologist may prescribe oral antibiotics (such as doxycycline or tetracycline), topical metronidazole, or azelaic acid depending on the diagnosis. For fungal involvement, antifungals like ketoconazole may be recommended.
Mini Case Study: Sarah’s Perioral Dermatitis Journey
Sarah, a 29-year-old teacher, struggled with recurring red bumps around her mouth for nearly six months. She assumed it was adult acne and used salicylic acid cleansers and spot treatments, which only increased dryness and stinging. After visiting a dermatologist, she learned she had perioral dermatitis likely triggered by her mint-flavored, fluoridated toothpaste and nightly application of a rich night cream that migrated toward her lips.
Following a simplified routine—switching to fluoride-free toothpaste, discontinuing the night cream, and using only a gentle cleanser and light moisturizer—her skin began improving within 10 days. By week 3, the bumps had cleared significantly. She now maintains clear skin by avoiding heavy products and checking ingredient labels carefully.
Checklist: How to Prevent Future Breakouts Around the Mouth
Use this checklist to maintain healthy skin in the perioral area:
- ✅ Switch to fluoride-free, SLS-free toothpaste
- ✅ Avoid heavy lip balms and oily skincare products near the mouth
- ✅ Wash face after meals if food residue accumulates
- ✅ Change pillowcases every 2–3 days
- ✅ Don’t use steroid creams on facial breakouts unless directed by a doctor
- ✅ Keep hands away from face; avoid resting phone against cheek
- ✅ Stay hydrated and support gut-skin health with balanced nutrition
Frequently Asked Questions
Can stress cause breakouts around the mouth?
Yes. Stress can disrupt hormone levels and weaken the skin barrier, making it more vulnerable to inflammation and infection. While stress alone may not initiate perioral dermatitis, it can exacerbate existing conditions.
Is it safe to pop the bumps around my mouth?
No. Popping increases the risk of scarring, infection, and spreading inflammation. These lesions are often not traditional whitehead pimples but rather inflamed follicles or dermatitis, which won’t “drain” like acne.
Can makeup worsen breakouts around the mouth?
Absolutely. Foundations, concealers, and lip products containing oils, waxes, or fragrances can clog pores or irritate sensitive skin. Always remove makeup thoroughly and sanitize applicators weekly.
Final Thoughts and Next Steps
Breakouts around the mouth are rarely just about poor hygiene or diet—they’re often the result of subtle, repeated exposures to irritants that accumulate over time. The solution isn’t harsh treatments but thoughtful elimination and simplification. By identifying personal triggers and adopting a gentle, consistent routine, most people can achieve lasting clarity.
Start today: check your toothpaste label, reassess your skincare application habits, and commit to a minimal routine for at least three weeks. Healing takes patience, but the results—a calm, balanced complexion—are worth it.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?