Waking up with a tingling cheek, feeling a sudden loss of sensation near your lips, or noticing one side of your face feels “off” can be unsettling. Facial numbness isn’t always a sign of something serious, but it should never be ignored. It’s your body’s way of signaling that nerves in your face may be compromised—whether due to pressure, inflammation, or an underlying medical condition. Understanding the root cause is essential to determining the right course of action.
Understanding Facial Numbness: What It Really Means
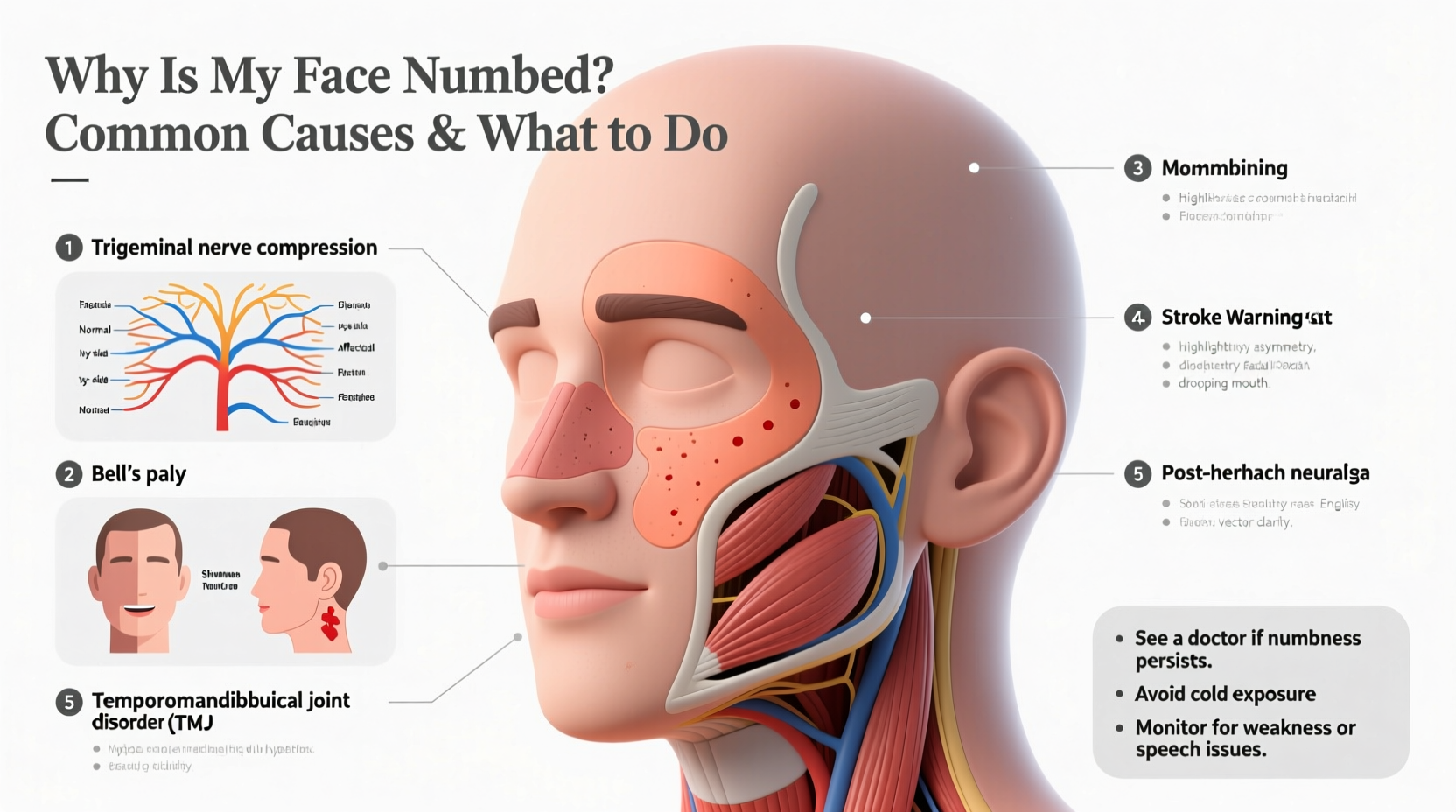
Facial numbness refers to a loss of sensation or a “pins and needles” feeling in any part of the face—cheeks, chin, forehead, nose, or around the mouth. Medically, this is often described as paresthesia, which occurs when the trigeminal nerve (the main sensory nerve of the face) is disrupted. Unlike muscle weakness or paralysis, numbness specifically affects sensation, not movement—though both can occur together in certain conditions.
The trigeminal nerve has three branches: ophthalmic (forehead and eyes), maxillary (cheeks and upper lip), and mandibular (jaw and lower lip). Depending on which branch is affected, the location of numbness varies. For example, dental procedures often impact the mandibular branch, while sinus infections may irritate the maxillary portion.
“Facial numbness is a neurological red flag. Even if temporary, it warrants attention to rule out progressive or systemic issues.” — Dr. Lena Torres, Neurologist at Boston General Hospital
Common Causes of Facial Numbness
Several factors can interfere with normal nerve function in the face. Some are benign and short-lived; others require immediate medical evaluation.
- Dental Procedures: Root canals, tooth extractions, or injections can temporarily damage or compress facial nerves, especially the inferior alveolar nerve. This type of numbness usually resolves within hours or days.
- Sinus Infections: Inflamed sinuses press against nearby nerves, particularly the maxillary branch, causing cheek and upper lip numbness. Often accompanied by congestion and facial pain.
- Trigeminal Neuralgia: A chronic condition causing sharp, electric-like facial pain and sometimes numbness due to nerve compression, often by a blood vessel.
- Multiple Sclerosis (MS): MS damages the protective sheath around nerves, including the trigeminal nerve. Facial numbness may be one of the first signs.
- Stroke or TIA (Transient Ischemic Attack): Sudden numbness, especially on one side of the face, along with slurred speech or arm weakness, requires emergency care.
- Diabetes: Long-term high blood sugar can lead to peripheral neuropathy, which occasionally affects facial nerves.
- Tumors: Benign or malignant growths in the brain or along the nerve pathway can compress nerves and disrupt sensation.
- Vitamin Deficiencies: Low levels of B12, B6, or E can impair nerve health and lead to numbness anywhere, including the face.
When to Seek Medical Help
Not all facial numbness is urgent, but knowing when to act can be life-saving. Persistent, worsening, or unilateral (one-sided) numbness should prompt a visit to a healthcare provider. Immediate evaluation is crucial if numbness is accompanied by:
- Slurred speech or difficulty understanding speech
- Weakness in arms or legs
- Sudden vision changes
- Loss of balance or coordination
- Severe headache
In such cases, time is critical. A transient ischemic attack (mini-stroke) or full-blown stroke must be ruled out within the first few hours for effective treatment.
Diagnostic Process: What to Expect
A doctor will likely perform a neurological exam to assess sensation, muscle strength, and reflexes. Imaging tests such as MRI or CT scans help detect structural issues like tumors, MS lesions, or stroke damage. Blood work may check for diabetes, vitamin deficiencies, or autoimmune markers.
| Symptom Pattern | Possible Cause | Action Required |
|---|---|---|
| Sudden onset, one side, with speech issues | Stroke/TIA | Emergency care |
| Gradual numbness after dental work | Nerve trauma | Monitor; follow up if persistent |
| Recurrent facial pain and numbness | Trigeminal neuralgia | Neurology referral |
| Numbness with fatigue, vision issues | Multiple sclerosis | MRI and specialist evaluation |
| Burning sensation, history of diabetes | Diabetic neuropathy | Blood sugar control + neuro check |
Step-by-Step: What to Do If Your Face Goes Numb
Reacting calmly and methodically increases your chances of accurate diagnosis and timely treatment.
- Assess for Emergency Signs: Check for facial drooping, slurred speech, or limb weakness. Use the FAST test: Face drooping? Arm weakness? Speech difficulty? Time to call emergency services.
- Note Onset and Duration: Was it sudden or gradual? Does it come and go? Keep a symptom journal.
- Review Recent Events: Did you have dental work, a head injury, or illness recently?
- Check for Other Symptoms: Headaches, vision changes, tingling in limbs, or balance issues add important context.
- Contact Your Doctor: Even if symptoms fade, schedule an appointment to investigate potential causes.
- Prepare for Evaluation: Bring a list of medications, medical history, and symptom notes to your appointment.
Real-Life Example: Recognizing the Warning Signs
Sarah, a 48-year-old teacher, noticed her left cheek felt “asleep” during a staff meeting. She dismissed it at first, thinking she’d slept awkwardly. But by lunchtime, her left hand was tingling too, and her words came out slightly slurred. A colleague urged her to call 911. At the hospital, a CT scan revealed a small clot in the right side of her brain—a TIA. Thanks to quick action, she received anticoagulant therapy and began lifestyle changes that prevented a full stroke. Her neurologist emphasized that facial numbness was the key early clue.
“Many patients wait too long because they assume facial numbness is stress or fatigue. But in neurology, new-onset numbness demands investigation.” — Dr. Raj Mehta, Stroke Specialist
Prevention and Long-Term Management
While not all causes of facial numbness are preventable, managing risk factors reduces the likelihood of serious conditions.
- Maintain healthy blood pressure and cholesterol to reduce stroke risk.
- Control blood sugar if you have diabetes.
- Get regular neurological checkups if you have a family history of MS or neuropathy.
- Ensure adequate intake of B vitamins through diet or supplements.
- Use protective gear during sports to avoid facial trauma.
Frequently Asked Questions
Can stress cause facial numbness?
Stress alone doesn’t directly damage nerves, but severe anxiety or panic attacks can cause hyperventilation, leading to temporary tingling or numbness in the face and extremities. This is due to altered carbon dioxide levels in the blood. While uncomfortable, it’s usually not dangerous—but should still be differentiated from neurological causes.
How long does facial numbness last after dental work?
Most post-dental numbness resolves within 1–4 hours as anesthesia wears off. If sensation doesn’t return after 24 hours, or if you experience prolonged tingling or pain, contact your dentist. Permanent nerve injury is rare but possible, especially with wisdom tooth extraction.
Is facial numbness a sign of a brain tumor?
It can be, though it’s uncommon. Slow-growing tumors near the trigeminal nerve or brainstem may cause gradual numbness, often with other symptoms like headaches, vision problems, or balance issues. Imaging is needed for confirmation. Most cases of facial numbness are not tumor-related.
Take Control of Your Health
Your body communicates through symptoms, and facial numbness is a message worth listening to. Whether it's a minor nerve irritation or a signal of a deeper issue, taking prompt, informed action protects your long-term well-being. Don’t downplay unusual sensations—especially if they’re new, persistent, or worsening. With early detection and proper care, many underlying causes are treatable or manageable.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?