A persistently blocked nose affects sleep, concentration, and overall quality of life. While occasional congestion is normal during colds or seasonal changes, chronic nasal blockage signals underlying issues that require attention. Millions experience this discomfort daily, often dismissing it as a minor inconvenience. However, understanding the root causes—ranging from allergies to structural abnormalities—is essential for lasting relief. This guide explores the most common reasons behind constant nasal congestion and provides practical, science-backed solutions.
Common Causes of Chronic Nasal Congestion
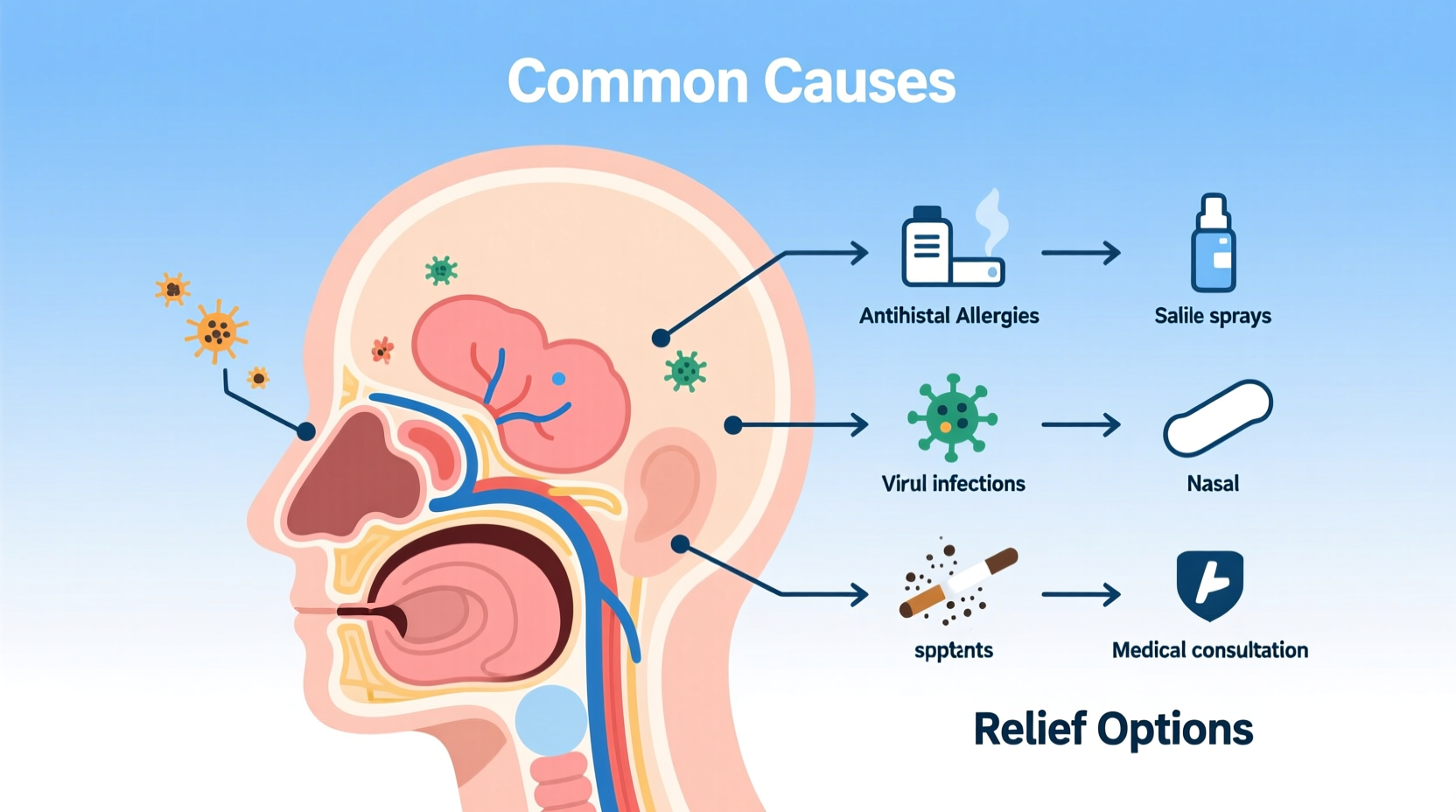
Nasal obstruction isn’t just about mucus buildup. It can stem from inflammation, physical blockages, or environmental triggers. Identifying the cause is the first step toward effective treatment.
- Allergic Rhinitis: Exposure to allergens like pollen, dust mites, or pet dander triggers immune responses that inflame nasal passages.
- Non-Allergic Rhinitis: Irritants such as smoke, strong odors, weather changes, or certain medications cause similar symptoms without an allergic reaction.
- Sinus Infections (Sinusitis): Bacterial or viral infections in the sinuses lead to swelling, mucus production, and pressure.
- Nasal Polyps: Soft, noncancerous growths in the nasal lining or sinuses obstruct airflow and reduce smell sensitivity.
- Deviated Septum: A crooked wall between the nostrils limits airflow on one or both sides, often worsening at night.
- Enlarged Adenoids or Turbinates: These tissues inside the nose may swell due to chronic irritation or infection, narrowing airways.
- Hormonal Changes: Pregnancy, menstruation, or thyroid disorders can increase blood flow to nasal membranes, causing swelling.
- Medication Side Effects: Drugs like beta-blockers, some antidepressants, and overuse of nasal decongestant sprays can exacerbate congestion.
When to See a Doctor
Occasional stuffiness resolves with rest or OTC remedies. But persistent blockage lasting more than 10–14 days warrants medical evaluation. Seek professional help if you experience:
- Facial pain or pressure lasting over a week
- Thick yellow-green nasal discharge with fever
- Limited sense of smell or taste
- Snoring or sleep apnea symptoms
- Bleeding from the nose unrelated to dryness
- No improvement after using antihistamines or saline rinses
“Chronic nasal obstruction should never be ignored. Long-term mouth breathing increases risks for dry mouth, dental issues, and even cardiovascular strain.” — Dr. Lena Patel, ENT Specialist, Massachusetts Eye and Ear
Effective Relief Strategies and Treatments
Relief depends on accurate diagnosis. Below are evidence-based approaches tailored to different causes.
Allergy-Related Congestion
Antihistamines (e.g., loratadine, cetirizine) reduce histamine release, while nasal corticosteroid sprays (fluticasone, mometasone) decrease inflammation. Allergy testing helps pinpoint specific triggers, enabling avoidance or immunotherapy.
Infections and Sinusitis
Viral infections resolve in 7–10 days. Bacterial sinusitis may require antibiotics. Saline irrigation flushes out pathogens and thins mucus. Steam inhalation with eucalyptus oil offers temporary relief.
Anatomical Issues
For deviated septums or large polyps, surgery may be necessary. Septoplasty corrects structural deviations, while endoscopic sinus surgery removes obstructions. These procedures significantly improve airflow and reduce recurrence of infections.
Medication-Induced Rhinitis
Known as rhinitis medicamentosa, this occurs from overusing topical decongestant sprays (like oxymetazoline) beyond 3–5 days. The rebound effect worsens congestion. Discontinuation under medical supervision, combined with steroid sprays, helps restore normal function.
| Condition | Primary Treatment | Time to Relief |
|---|---|---|
| Allergic Rhinitis | Nasal steroids + antihistamines | 3–7 days |
| Acute Sinusitis | Saline rinses + decongestants | 7–14 days |
| Deviated Septum | Surgical correction | Weeks post-op |
| Rhinitis Medicamentosa | Stop spray, use steroid alternative | Gradual over 1–2 weeks |
Step-by-Step Guide to Daily Nasal Care
Implementing a routine can prevent flare-ups and maintain clear breathing. Follow this daily protocol:
- Morning: Rinse and Protect
Use a neti pot or saline spray to clear overnight buildup. Apply a thin layer of petroleum jelly inside nostrils if air is dry. - Daytime: Avoid Triggers
Keep windows closed during high pollen seasons. Wear a mask in dusty environments. Stay hydrated to keep mucus thin. - Evening: Reduce Inflammation
Use prescribed nasal spray (if applicable) at the same time each night. Elevate your head while sleeping to reduce congestion. - Weekly: Clean Environment
Wash bedding in hot water weekly. Replace HVAC filters monthly. Vacuum carpets and upholstery regularly. - Monthly: Review Symptoms
Note any pattern changes. Adjust treatments or consult a doctor if new symptoms arise.
Real-Life Example: Managing Year-Round Congestion
Sarah, a 34-year-old teacher, struggled with constant nasal blockage for over two years. She assumed it was seasonal allergies and used OTC decongestants frequently. Over time, her symptoms worsened, especially at night. After visiting an ENT specialist, she was diagnosed with both allergic rhinitis and a mild deviated septum. Skin testing revealed sensitivities to dust mites and mold. Her treatment plan included nightly fluticasone spray, biweekly saline rinses, replacing her mattress and pillows with allergen-proof covers, and eventually undergoing septoplasty. Within three months, her breathing improved dramatically, and she no longer relied on medication daily.
Checklist: What You Can Do Today
- ✔️ Try a saline nasal rinse tonight
- ✔️ Discard any nasal spray used for more than five consecutive days
- ✔️ Check your bedroom for dust accumulators (carpets, blinds, stuffed toys)
- ✔️ Hydrate with at least 8 glasses of water
- ✔️ Schedule an appointment with an allergist or ENT if symptoms persist
Frequently Asked Questions
Can stress cause a blocked nose?
Yes. Stress activates the autonomic nervous system, which can trigger vasomotor rhinitis—an imbalance in nasal blood flow leading to swelling and congestion. Managing stress through mindfulness or exercise may reduce episodes.
Is it safe to use a neti pot every day?
Yes, if done correctly. Always use distilled, sterile, or previously boiled water. Clean the device thoroughly after each use to prevent bacterial contamination. Daily use is generally safe for those with chronic conditions under medical guidance.
Why is my nose more blocked at night?
Lying down increases blood flow to the nasal area, worsening swelling. Dry bedroom air, dust mites in bedding, or acid reflux can also contribute. Elevating your head and using a humidifier often helps.
Take Control of Your Breathing
Living with a constantly blocked nose doesn’t have to be your normal. Whether the cause is environmental, physiological, or lifestyle-related, effective solutions exist. From simple daily habits like saline rinsing to targeted medical interventions, relief is within reach. Don’t settle for temporary fixes—address the root issue and reclaim comfortable, natural breathing.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?