A constantly runny nose can be more than just a minor annoyance—it can interfere with daily life, disrupt sleep, and affect concentration. Whether it happens seasonally or persists year-round, understanding the root cause is essential for effective treatment and long-term relief. Nasal discharge, medically known as rhinorrhea, results from inflammation or irritation of the nasal tissues. While often harmless, chronic symptoms may point to underlying health conditions that require attention.
Common Causes of a Runny Nose
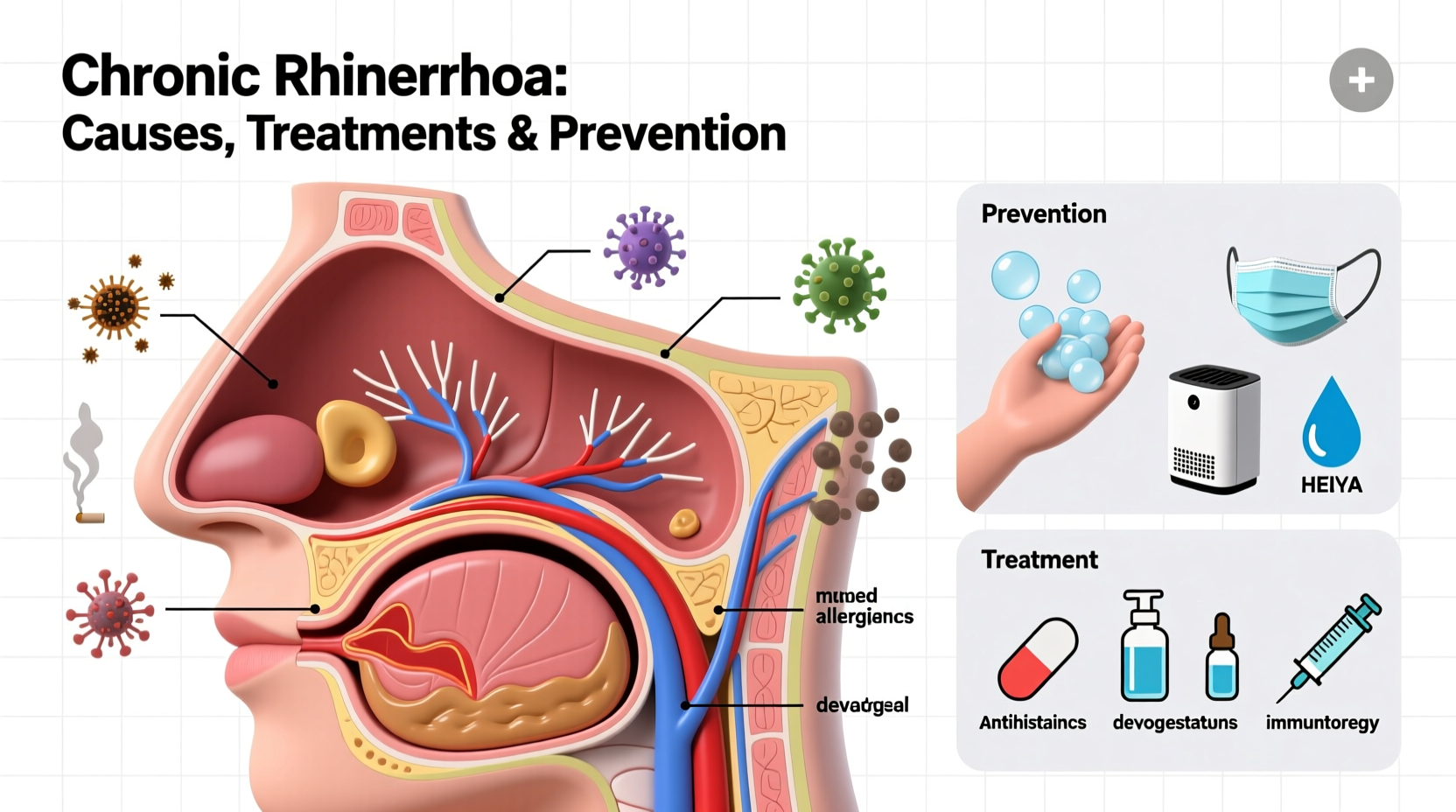
The most frequent triggers of persistent nasal discharge include allergies, infections, environmental irritants, and structural issues in the nasal passages. Identifying which factor applies to you is the first step toward targeted relief.
- Allergic Rhinitis: Also known as hay fever, this immune response to allergens like pollen, dust mites, pet dander, or mold causes sneezing, itching, and a watery nasal discharge.
- Viral Infections: The common cold or flu viruses inflame the nasal lining, leading to increased mucus production that typically lasts 7–10 days.
- Non-Allergic Rhinitis: This condition mimics allergy symptoms but isn’t caused by an immune response. Triggers include weather changes, strong odors, smoke, spicy foods, or hormonal fluctuations.
- Sinusitis: When sinuses become infected or inflamed, thick yellow or green mucus may accompany facial pressure, headache, and congestion—though clear drainage can also occur.
- Medications: Certain blood pressure drugs (like ACE inhibitors), antidepressants, and overuse of nasal decongestant sprays can lead to chronic rhinorrhea.
- Anatomical Issues: A deviated septum or nasal polyps can obstruct normal airflow and drainage, contributing to persistent symptoms.
Treatment Options Based on Cause
Effective treatment depends entirely on the underlying cause. Self-treatment without diagnosis may provide temporary relief but can delay proper management.
Allergy-Related Runny Nose
Antihistamines such as loratadine (Claritin), cetirizine (Zyrtec), or fexofenadine (Allegra) help block histamine release. Intranasal corticosteroid sprays like fluticasone (Flonase) reduce inflammation when used consistently. For severe cases, immunotherapy (allergy shots or sublingual tablets) may gradually desensitize the immune system.
Infection-Induced Rhinorrhea
Viral infections resolve on their own. Supportive care includes hydration, rest, saline rinses, and steam inhalation. If bacterial sinusitis is diagnosed—typically after symptoms persist beyond 10 days—antibiotics may be prescribed.
Non-Allergic Rhinitis
Ipratropium bromide nasal spray specifically targets excessive watery discharge. Avoiding known irritants and using barrier methods (e.g., face masks during cleaning) can significantly reduce flare-ups.
Medication-Induced Symptoms
If you suspect a medication is causing your runny nose, consult your doctor before making changes. Alternatives may be available, especially for blood pressure medications linked to rhinitis.
“Persistent nasal symptoms shouldn’t be dismissed as ‘just allergies.’ Accurate diagnosis ensures appropriate therapy and prevents unnecessary suffering.” — Dr. Lena Torres, Board-Certified Otolaryngologist
Prevention Strategies That Work
While not all causes are preventable, many risk factors can be managed through lifestyle adjustments and environmental control.
Environmental Control Measures
- Use HEPA air purifiers to reduce airborne allergens indoors.
- Wash bedding weekly in hot water to eliminate dust mites.
- Keep windows closed during high pollen seasons.
- Avoid smoking and secondhand smoke exposure.
- Limit use of strong perfumes, aerosols, and chemical cleaners.
Diet and Hydration
Staying well-hydrated thins mucus, making it easier to clear. Some individuals report symptom improvement after reducing dairy intake, though scientific evidence remains limited. Spicy foods may temporarily increase drainage due to capsaicin stimulation.
Nasal Health Maintenance
Regular saline irrigation using a neti pot or squeeze bottle helps flush out irritants and excess mucus. Use distilled, sterile, or previously boiled water to avoid infection risks.
Step-by-Step Guide to Managing Chronic Rhinorrhea
Follow this practical sequence to gain control over persistent nasal symptoms:
- Track Your Symptoms: Keep a journal noting when your nose runs, potential triggers (food, environment, activity), and associated symptoms like sneezing or post-nasal drip.
- Eliminate Obvious Irritants: Remove scented candles, switch to fragrance-free laundry products, and vacuum regularly with a HEPA filter.
- Start Conservative Treatments: Begin with daily saline nasal rinses and an oral antihistamine if allergies are suspected.
- Evaluate Response After One Week: If symptoms improve, continue treatment. If unchanged, consider adding a steroid nasal spray (available over-the-counter).
- Consult a Specialist: If no improvement occurs within two weeks, see an ENT (ear, nose, and throat doctor) or allergist for testing and advanced diagnostics.
Do’s and Don’ts: Quick Reference Table
| Do’s | Don’ts |
|---|---|
| Use saline sprays regularly to moisturize nasal passages | Overuse decongestant nasal sprays (limit to 3 days) |
| Shower before bed to wash off pollen from hair and skin | Ignore worsening symptoms like facial pain or discolored mucus lasting over 10 days |
| Invest in hypoallergenic pillow covers and mattress protectors | Blow your nose too hard—this increases sinus pressure and risk of ear pain |
| Stay hydrated to keep mucus thin and easy to drain | Assume every runny nose is an allergy—non-allergic causes are common |
Real-Life Example: Sarah’s Seasonal Struggle
Sarah, a 34-year-old teacher, experienced a runny nose every spring for years. She assumed it was just “bad allergies” and relied on over-the-counter antihistamines with inconsistent results. After her symptoms began affecting her voice and sleep, she consulted an allergist. Skin testing revealed sensitivity to tree pollen and mold spores. With a personalized plan including preseason steroid spray use, air purifier installation at home, and timed outdoor activities, her symptoms decreased by over 80% within one year. Her case highlights how proper diagnosis transforms ineffective coping into proactive management.
Frequently Asked Questions
Can stress make my nose run?
Yes. Stress activates the autonomic nervous system, which can stimulate nasal glands and increase mucus production, especially in people with non-allergic rhinitis. Managing stress through mindfulness or exercise may help reduce episodes.
Is it normal for my nose to run only on one side?
Occasional unilateral discharge can occur due to positional drainage or localized irritation. However, persistent one-sided rhinorrhea—especially if clear and watery—should be evaluated by a doctor, as it could indicate a cerebrospinal fluid leak or nasal tumor.
When should I see a doctor about a runny nose?
Seek medical advice if symptoms last longer than 10 days, worsen after initial improvement, include high fever, facial swelling, or bloody/discolored discharge, or significantly impact quality of life. Children with persistent nasal symptoms should also be assessed for adenoid enlargement or chronic sinus issues.
Take Control of Your Nasal Health
A constantly runny nose doesn’t have to be a permanent part of your life. By identifying the cause—whether allergic, infectious, environmental, or structural—you can apply targeted treatments and meaningful prevention strategies. Small daily habits, like using saline rinses and controlling indoor allergens, often yield significant improvements. Don’t hesitate to seek professional evaluation if self-care isn’t enough. Long-term relief is possible with the right approach.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?