Nasal congestion—commonly known as a stuffy nose—is one of the most frequent complaints during cold season, allergy flare-ups, or even in dry environments. It’s not just uncomfortable; it can disrupt sleep, impair concentration, and make daily activities more difficult. While occasional congestion is normal, persistent or severe blockage may signal an underlying condition. Understanding the root causes, recognizing associated symptoms, and applying targeted relief strategies are essential for regaining comfort and restoring normal breathing.
Common Causes of Nasal Congestion
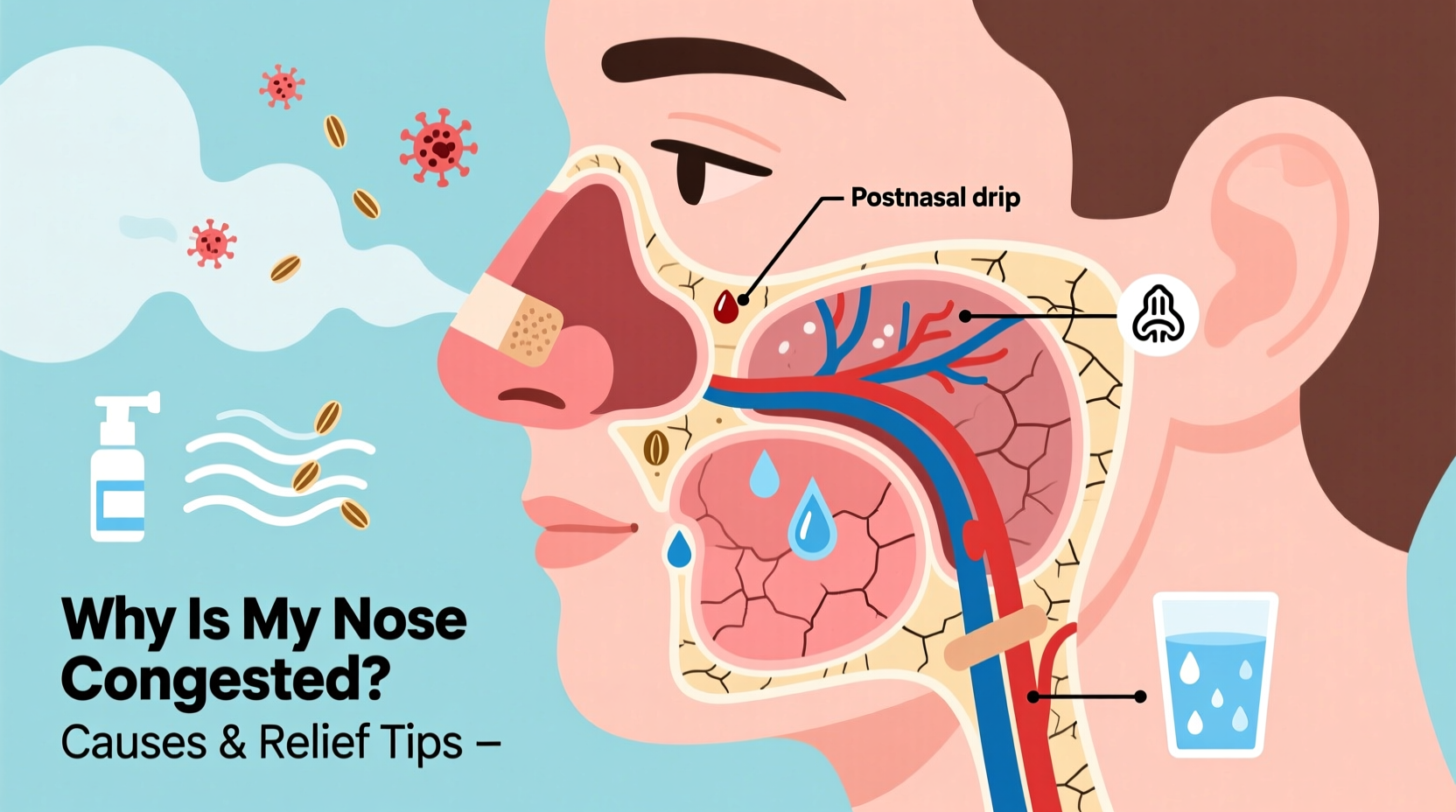
Nasal congestion occurs when the tissues lining the nasal passages become inflamed and swollen. This swelling restricts airflow, leading to that familiar feeling of blockage. Several factors can trigger this inflammation:
- Viral infections: The common cold and influenza are leading causes. Viruses irritate the nasal lining, increasing mucus production and causing swelling.
- Allergies: Seasonal allergens like pollen, mold, or indoor triggers such as dust mites and pet dander provoke immune responses that result in nasal congestion.
- Sinusitis: Bacterial or viral infection of the sinuses leads to thick mucus buildup and pressure, often accompanied by facial pain.
- Deviated septum: A structural issue where the nasal septum (the wall between nostrils) is off-center, restricting airflow on one side.
- Environmental irritants: Smoke, strong perfumes, air pollution, and dry air can inflame nasal membranes.
- Hormonal changes: Pregnancy, menstruation, or thyroid issues can affect blood flow to nasal tissues, causing temporary congestion.
- Medication overuse: Nasal decongestant sprays used for more than 3–5 days can lead to rebound congestion (rhinitis medicamentosa).
Symptoms That Often Accompany Nasal Blockage
Congestion rarely occurs in isolation. Recognizing accompanying symptoms helps pinpoint the cause and determine appropriate treatment:
- Runny nose with clear, yellow, or green discharge
- Postnasal drip causing cough or sore throat
- Facial pressure or pain, especially around cheeks and eyes
- Reduced sense of smell or taste
- Sneezing and itchy eyes (common in allergies)
- Fatigue due to disrupted sleep
- Mild fever (in infections)
Persistent congestion lasting more than 10 days, high fever, or severe headache warrants medical evaluation to rule out bacterial sinusitis or other complications.
Effective Relief Tips and Home Remedies
Most cases of nasal congestion resolve on their own within a week. However, several practical measures can speed recovery and improve comfort:
- Use saline nasal irrigation: Rinsing nasal passages with a saline solution using a neti pot or squeeze bottle clears mucus and allergens. Use distilled or previously boiled water to avoid infection risk.
- Stay hydrated: Drinking plenty of fluids thins mucus, making it easier to expel. Warm liquids like herbal tea or broth provide additional soothing effects.
- Elevate your head while sleeping: Propping up with extra pillows reduces blood flow to nasal tissues, minimizing nighttime congestion.
- Employ a humidifier: Adding moisture to dry indoor air prevents nasal membranes from drying out and becoming irritated.
- Apply warm compresses: Placing a warm, damp cloth over the nose and forehead eases sinus pressure and promotes drainage.
- Avoid irritants: Steer clear of cigarette smoke, strong scents, and dusty environments that worsen inflammation.
“Saline irrigation is one of the safest and most effective ways to manage chronic nasal congestion, especially for those with allergies.” — Dr. Lena Patel, Otolaryngologist
Do’s and Don’ts When Managing Nasal Congestion
| Do’s | Don’ts |
|---|---|
| Use saline sprays regularly | Overuse nasal decongestant sprays (>3 days) |
| Drink warm fluids frequently | Blow your nose too hard (can increase pressure and cause ear pain) |
| Take steam inhalations (e.g., hot shower) | Ignore signs of infection like persistent green mucus and fever |
| Keep bedroom air moist with a humidifier | Smoke or expose yourself to secondhand smoke |
| Wash hands often to prevent virus spread | Self-prescribe antibiotics (they don’t work on viruses) |
When to See a Doctor: A Step-by-Step Guide
While most congestion resolves with self-care, certain red flags require professional assessment. Follow this timeline to determine if medical intervention is needed:
- Days 1–3: Monitor symptoms. Begin hydration, saline rinses, and rest. Use OTC pain relievers if needed.
- Days 4–7: If symptoms persist but are improving slowly, continue home care. Note any worsening signs.
- Day 8 and beyond: Seek medical advice if congestion lasts longer than 10 days, especially with thick yellow-green mucus, facial pain, or fever above 101°F (38.3°C).
- Immediate consultation: Required for severe headache, vision changes, swelling around the eyes, or difficulty breathing.
- Chronic congestion: If you experience stuffiness most days, consider seeing an ENT specialist to evaluate for structural issues or chronic rhinitis.
Real-Life Example: Managing Allergy-Induced Congestion
Sarah, a 34-year-old teacher, noticed her nose became increasingly blocked every spring. She initially dismissed it as frequent colds, but the pattern repeated annually. After tracking her symptoms and noticing they worsened outdoors on high-pollen days, she consulted an allergist. Skin testing confirmed sensitivity to tree pollen. With prescribed antihistamines and a daily saline rinse routine, Sarah reduced her congestion significantly. She also began using an air purifier at home and changed clothes after being outside—simple changes that made a major difference.
FAQ: Frequently Asked Questions
Can dehydration cause a stuffy nose?
Yes. Dehydration thickens mucus, making it harder to drain and contributing to nasal blockage. Staying well-hydrated helps keep secretions thin and easier to clear.
Is it safe to use nasal spray every day?
It depends on the type. Saline sprays are safe for daily use. However, decongestant sprays like oxymetazoline should not be used for more than 3 consecutive days to avoid rebound congestion.
Why is my nose more congested at night?
Lying down increases blood flow to the head and nasal area, exacerbating swelling. Dry bedroom air and allergens in bedding (like dust mites) can also contribute to nighttime stuffiness.
Conclusion: Take Control of Your Breathing
Nasal congestion, though common, doesn’t have to derail your life. By identifying the underlying cause—whether it's a cold, allergies, or environmental factors—you can apply targeted, effective relief strategies. Simple habits like staying hydrated, using saline rinses, and optimizing your sleep environment can make a noticeable difference. For persistent or recurring issues, don’t hesitate to seek medical guidance. Breathing freely isn’t a luxury—it’s a necessity for rest, focus, and overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?