As women move through their 30s, 40s, and beyond, many notice subtle—but sometimes significant—changes in their menstrual cycles. One of the most common shifts is a gradual lightening of menstrual flow. While this can be a natural part of aging, especially as reproductive hormones fluctuate, it’s important to understand what’s normal and what might signal an underlying condition.
Periods that become lighter over time are often linked to hormonal shifts, lifestyle factors, or the early stages of perimenopause. However, sudden or extreme changes in flow, accompanied by other symptoms, may require medical evaluation. This article explores the science behind changing periods with age, identifies key warning signs, and provides practical guidance on when to seek help.
The Natural Shift: Why Periods Lighten with Age
Menstrual patterns evolve throughout a woman’s life due to hormonal fluctuations, reproductive milestones, and overall physiological changes. In the childbearing years, regular ovulatory cycles produce consistent estrogen and progesterone levels, leading to predictable and typically moderate-to-heavy flows.
Starting in the mid-to-late 30s, ovarian function begins to decline gradually. The number of available follicles decreases, and ovulation becomes less regular. This leads to lower progesterone production and sometimes reduced estrogen peaks, which directly affect the thickness of the uterine lining (endometrium). A thinner endometrium means less tissue to shed during menstruation—resulting in lighter periods.
Dr. Lena Patel, a board-certified gynecologist specializing in midlife women’s health, explains:
“By the time most women reach their early 40s, it's common to see shorter cycles, lighter bleeding, or even skipped periods. These are often early signs of perimenopause—the transition phase leading up to menopause.”
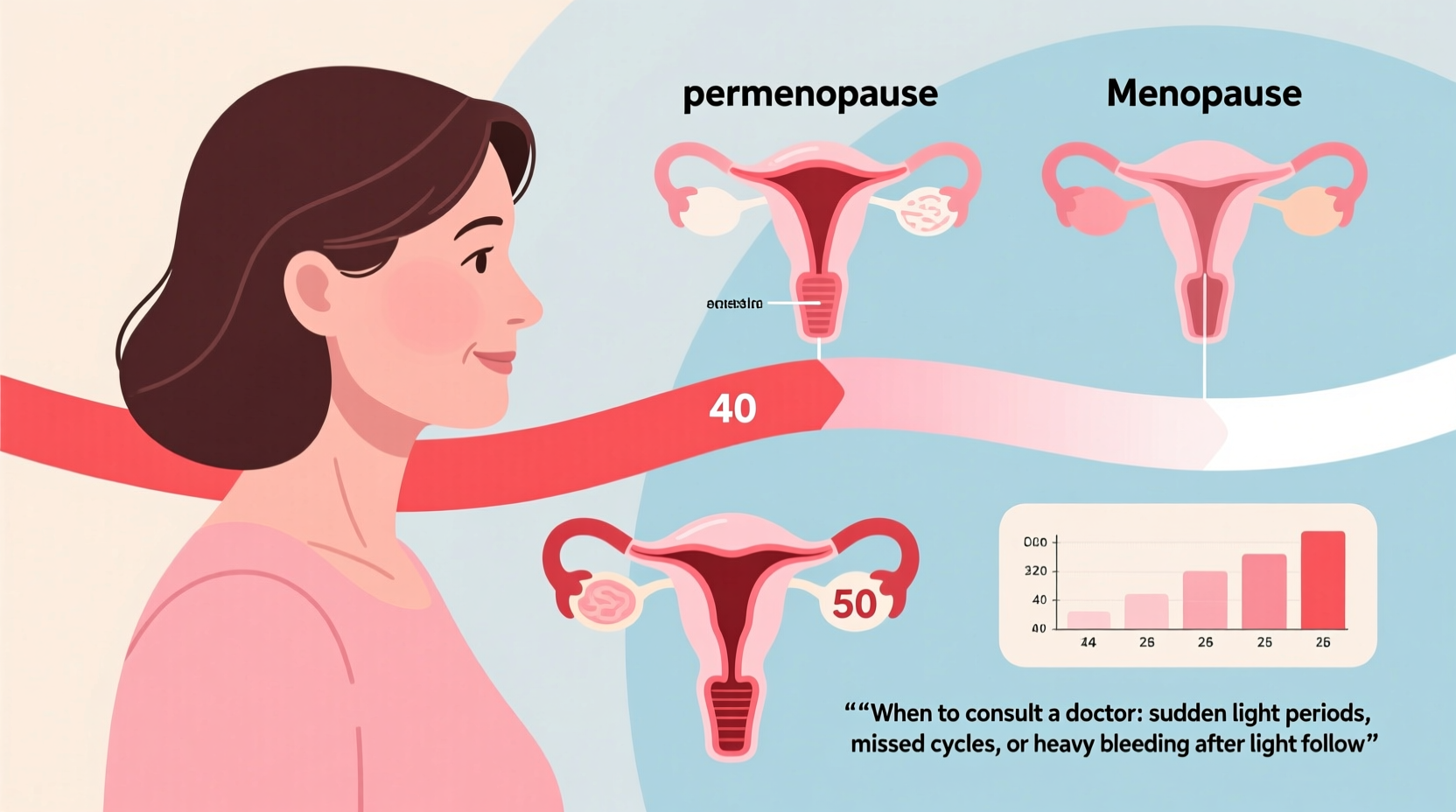
This transition can last anywhere from 2 to 10 years and usually begins between ages 40 and 55. During this time, hormonal variability causes irregularities in both cycle length and flow intensity.
Common Causes of Lighter Periods After 35
Not all lighter periods are due to aging. Several interrelated factors contribute to reduced menstrual flow as women grow older. Understanding these can help differentiate between normal progression and potential concerns.
- Hormonal Changes: Declining ovarian reserve reduces estrogen and progesterone output, affecting endometrial buildup.
- Perimenopause: Characterized by erratic ovulation, this phase often includes lighter, shorter, or missed periods.
- Thyroid Disorders: Both hypothyroidism and hyperthyroidism can disrupt menstrual regularity and reduce flow.
- Weight Loss or Low Body Fat: Significant weight loss, excessive exercise, or eating disorders can suppress reproductive hormones.
- Birth Control Use: Long-term use of hormonal contraceptives, particularly IUDs like Mirena, often leads to very light or absent periods.
- Stress and Sleep Disruption: Chronic stress elevates cortisol, which interferes with the hypothalamic-pituitary-ovarian axis.
- Uterine Scarring (Asherman’s Syndrome): Rare but possible after procedures like D&C; can cause diminished or absent periods.
It's not uncommon for women in their late 30s and 40s to go from needing super-absorbency tampons to barely requiring a liner. If this change occurs gradually and without discomfort, it's likely part of the natural reproductive aging process.
When to Be Concerned: Red Flags That Warrant Evaluation
A slow transition toward lighter periods is generally not alarming. However, certain patterns suggest the need for medical assessment. Sudden onset, extreme reduction, or accompanying symptoms could indicate hormonal imbalances, structural issues, or systemic conditions.
| Symptom Pattern | Likely Significance | Recommended Action |
|---|---|---|
| Gradual lightening over several years | Normal aging / perimenopause | Monitor; no immediate concern |
| Sudden drop in flow or missed periods (under 40) | Possible hormonal imbalance, PCOS, thyroid issue | See gynecologist for hormone testing |
| Spotting only, lasting less than 1 day | Low estrogen, anovulatory cycle, or birth control effect | Evaluate if persistent or new |
| Light periods + hot flashes, night sweats, insomnia | Early perimenopause | Discuss symptom management with provider |
| Very light or absent periods after stopping birth control | Potential post-pill amenorrhea or underlying dysfunction | Seek evaluation if lasting >3 months |
| Light bleeding + pelvic pain or pressure | Possible fibroids, polyps, or adenomyosis | Ultrasound recommended |
If you're under 40 and experience consistently light or absent periods without a clear cause (like contraceptive use), it's wise to consult a healthcare provider. Primary ovarian insufficiency (POI), once known as premature menopause, affects about 1% of women under 40 and can present with diminishing flow before full cessation.
Step-by-Step Guide: Evaluating Your Changing Cycle
If you're unsure whether your lighter periods are normal, follow this structured approach to gather information and determine next steps:
- Track Your Cycles for 3 Months: Record start date, duration, flow level (light/medium/heavy), clotting, and symptoms like cramps or fatigue.
- Assess Lifestyle Factors: Consider recent weight changes, stress levels, sleep quality, and exercise intensity.
- Review Medications: Identify any hormonal treatments, including IUDs, birth control pills, or medications for mental health or thyroid.
- Check for Other Symptoms: Note hot flashes, vaginal dryness, mood changes, or irregular ovulation signs (e.g., lack of cervical mucus).
- Schedule a Clinical Visit: Bring your tracking data to discuss with your OB-GYN or primary care provider.
- Request Key Tests: Ask for blood work including FSH, LH, estradiol, TSH, and AMH (anti-Müllerian hormone) to assess ovarian reserve and rule out thyroid disease.
- Consider Imaging: If structural concerns exist, a transvaginal ultrasound can evaluate the uterus and ovaries.
This systematic evaluation helps distinguish between expected age-related changes and conditions requiring intervention.
Real-Life Example: Navigating Perimenopausal Changes
Sarah, a 44-year-old teacher, noticed her periods had changed significantly over two years. Once heavy and five-day affairs, they became two-day events with minimal flow. At first, she assumed it was stress-related, as her job had grown more demanding. But when she began experiencing night sweats and difficulty sleeping, she scheduled a visit with her gynecologist.
After reviewing Sarah’s cycle diary and ordering blood tests, her doctor found elevated FSH levels and low AMH—indicative of declining ovarian function. Thyroid tests were normal. Sarah was diagnosed with early perimenopause. With guidance, she started managing symptoms through lifestyle adjustments, low-dose hormone therapy, and mindfulness practices for sleep support.
“I didn’t realize how much I was dismissing my body’s signals,” Sarah shared. “Once I got answers, I felt empowered—not anxious—about the changes.”
Her case highlights the importance of proactive monitoring and professional input when menstrual patterns shift unexpectedly.
Do’s and Don’ts: Managing Light Periods Wisely
To maintain reproductive health during midlife transitions, consider the following best practices.
| Do’s | Don’ts |
|---|---|
| Track your cycle regularly | Ignore sudden or dramatic changes |
| Maintain a healthy weight and balanced diet | Engage in extreme dieting or over-exercising |
| Stay hydrated and manage stress | Self-diagnose based on internet searches |
| Discuss concerns with your healthcare provider | Assume all changes are “just aging” without evaluation |
| Consider bone density and heart health as estrogen declines | Neglect preventive screenings like mammograms and Pap smears |
Frequently Asked Questions
Can lighter periods mean I’m infertile?
Lighter periods don’t necessarily mean infertility, but they can indicate irregular or absent ovulation, which affects fertility. As ovarian reserve declines with age, conception becomes more challenging—even with regular cycles. If you’re trying to conceive and notice cycle changes, consult a reproductive endocrinologist early.
Is it normal to have a 1-day period at age 45?
Yes, short periods are increasingly common in the perimenopausal window. A one- or two-day bleed with light flow is typical as hormone levels fluctuate and ovulation becomes sporadic. However, if this is a sudden change from your usual pattern, it’s worth discussing with your doctor.
Should I worry if my period stops before age 45?
Menopause before 45 is considered early; before 40 is premature. While some variation is normal, early cessation of periods may increase risks for osteoporosis, cardiovascular disease, and cognitive decline due to prolonged estrogen deficiency. Evaluation and possibly hormone therapy are often recommended.
Conclusion: Listen to Your Body, Take Informed Action
Lighter periods with age are frequently a normal reflection of shifting hormones and the natural path toward menopause. But your menstrual cycle is more than just a monthly event—it’s a vital sign of your overall health. Paying attention to its rhythm, volume, and associated symptoms allows you to respond proactively rather than reactively.
There’s no single “right” way to experience perimenopause, but knowledge and awareness make a meaningful difference. Whether your changes are subtle or pronounced, keeping records, understanding your options, and partnering with a trusted healthcare provider ensures you’re supported through every stage.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?