Stool color is more than just a bathroom curiosity—it can be a direct window into your digestive and overall health. While brown is the standard hue due to bile pigments, stool that appears pale, clay-colored, or almost white is a red flag worth investigating. This change often points to issues with the liver, gallbladder, or pancreas, particularly involving bile production or flow. Ignoring it could delay diagnosis of serious conditions like bile duct obstruction or liver disease.
This article breaks down the science behind white or near-white stools, identifies common and rare causes, explains when to take action, and outlines what medical professionals typically assess during evaluation.
What Makes Stool Brown—and Why It Might Not Be
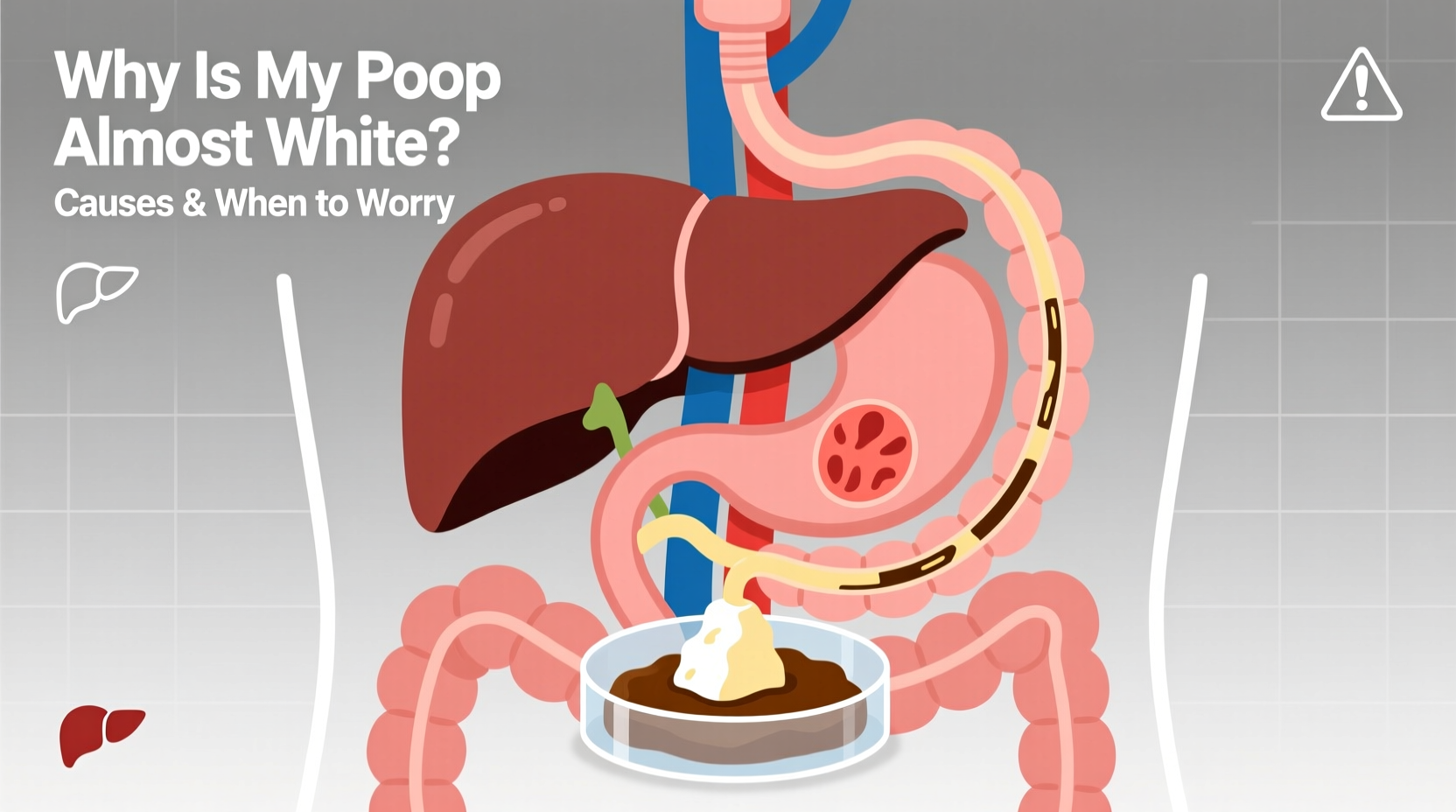
The typical brown color of human stool comes from bilirubin, a pigment formed when the liver breaks down old red blood cells. Bilirubin is processed into bile, stored in the gallbladder, and released into the small intestine during digestion. As bacteria in the gut act on bile, stercobilin—a byproduct—gives feces its characteristic brown tint.
When bile isn’t reaching the intestines, this coloring process doesn’t occur. The result? Pale, putty-like, or chalky white stools. This absence of bile suggests a blockage, malfunction, or disruption somewhere along the biliary system.
“Clay-colored stools are one of the most telling signs of biliary obstruction. When I see this in a patient, we immediately investigate liver function and duct integrity.” — Dr. Lena Torres, Gastroenterologist at Boston Digestive Institute
Common Causes of White or Pale Stools
Several underlying conditions can interfere with bile delivery. The most frequent culprits include:
- Gallstones: These hard deposits can block the bile ducts, preventing bile from entering the intestines. Episodes may come with sharp pain in the upper right abdomen, nausea, and jaundice.
- Liver disease: Conditions like hepatitis (viral, alcoholic, or autoimmune) impair the liver’s ability to produce bile. Cirrhosis can also disrupt bile flow over time.
- Pancreatic disorders: Chronic pancreatitis or pancreatic cancer may compress the bile duct, especially when tumors grow near the head of the pancreas.
- Bile duct strictures or tumors: Narrowing or growths in the bile ducts obstruct flow. These may develop after surgery, inflammation, or malignancy.
- Medications: Certain antacids containing aluminum hydroxide or anti-diarrheal drugs like bismuth subsalicylate (Pepto-Bismol) can temporarily lighten stool color, though not usually to pure white.
When to Worry: Red Flags That Demand Medical Attention
Occasional light-colored stool may not be alarming, especially if tied to diet or short-term medication use. However, persistent white or clay-colored poop lasting more than 1–2 days—especially when paired with other symptoms—requires prompt evaluation.
Seek immediate medical attention if pale stools are accompanied by any of the following:
- Yellowing of the skin or eyes (jaundice)
- Dark urine (like tea or cola)
- Pain in the upper right abdomen
- Nausea, vomiting, or unexplained weight loss
- Fever or chills
- Fatigue or loss of appetite
These combinations suggest a significant disruption in bile flow and could indicate acute cholangitis, gallstone impaction, or malignancy.
Timeline: What Happens After You Report Pale Stools?
If you raise concerns about white stools with your physician, here’s what typically follows:
- Medical history review: Your doctor will ask about medications, alcohol use, recent illnesses, and family history of liver or gallbladder disease.
- Physical exam: Focus on abdominal tenderness, liver enlargement, or jaundice.
- Blood tests: Liver function tests (LFTs), bilirubin levels, alkaline phosphatase, and pancreatic enzymes (amylase, lipase) are checked.
- Imaging: Abdominal ultrasound is usually first. If blockage is suspected, MRCP (Magnetic Resonance Cholangiopancreatography) or endoscopic ultrasound may follow.
- Specialist referral: A gastroenterologist may perform an ERCP (Endoscopic Retrograde Cholangiopancreatography) to both diagnose and treat duct obstructions.
Diagnostic Table: Causes vs. Symptoms and Tests
| Cause | Key Symptoms | Diagnostic Test | Treatment Approach |
|---|---|---|---|
| Gallstones | Right upper quadrant pain, nausea, fever | Abdominal ultrasound | Laparoscopic cholecystectomy or ERCP |
| Hepatitis | Fatigue, dark urine, jaundice | Liver panel, viral serology | Antivirals, lifestyle changes, monitoring |
| Pancreatic cancer | Weight loss, back pain, jaundice | CT scan, EUS, CA19-9 marker | Surgery, chemotherapy, stenting |
| Bile duct stricture | Chronic pale stools, itching | MRCP or ERCP | Stent placement, surgical repair |
| Medication effect | No other symptoms, recent drug use | Clinical history | Discontinuation or substitution |
Real-Life Example: Recognizing the Warning Signs
Mark, a 58-year-old teacher, noticed his stools had turned pale over three days. At first, he dismissed it as something he ate. But when his urine darkened and he began feeling fatigued, he consulted his doctor. Blood work showed elevated bilirubin and alkaline phosphatase. An ultrasound revealed a dilated bile duct, and an MRCP confirmed a stone lodged in the common bile duct. Through an ERCP procedure, the stone was removed, and Mark recovered fully within weeks.
His case underscores the importance of acting early. Had he waited, he risked developing cholangitis—an infection of the bile duct that can become life-threatening.
Prevention and Monitoring Checklist
While not all causes of pale stools are preventable, certain lifestyle choices reduce risk. Use this checklist to support biliary and liver health:
- ✅ Limit alcohol consumption to moderate levels or avoid it entirely
- ✅ Maintain a balanced diet low in saturated fats to reduce gallstone risk
- ✅ Stay hydrated and exercise regularly to support metabolic health
- ✅ Avoid rapid weight loss diets, which increase gallstone formation
- ✅ Get vaccinated against Hepatitis A and B if recommended
- ✅ Review medications annually with your doctor for potential liver impact
- ✅ Schedule routine physical exams, including liver enzyme screening
Frequently Asked Questions
Can dehydration cause white poop?
No, dehydration typically leads to darker, harder stools due to reduced water content. White or clay-colored stools are linked to bile deficiency, not fluid balance.
Is it dangerous if white stool only happens once?
A single instance is usually not concerning, especially if no other symptoms are present. However, recurrence or persistence beyond 48 hours warrants medical review.
Can children have white poop? What should parents do?
Yes, though rare. In infants, pale stools can signal biliary atresia—a serious condition requiring surgery within the first few months of life. Parents should report consistently light-colored stools in babies to a pediatrician immediately.
Conclusion: Don’t Ignore the Signal
White or nearly white stool is not normal and should never be ignored. It’s a physiological warning sign that something is interfering with bile—a critical component of digestion and detoxification. Whether due to a gallstone, liver inflammation, or a more serious condition like pancreatic cancer, timely investigation improves outcomes dramatically.
Your digestive system communicates through subtle cues. Pale stool is one of the loudest. Pay attention, act promptly, and consult a healthcare provider if something feels off. Early diagnosis can mean the difference between a quick fix and a long-term health challenge.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?