Noticing an unexpected color in the toilet bowl can be unsettling. If you’ve recently seen orange poop and are wondering why, you’re not alone. While stool color varies naturally due to diet and hydration, a distinct orange hue often raises questions. In most cases, orange stool is harmless and linked to something you’ve eaten or a supplement you’re taking. However, it can occasionally signal underlying digestive or liver issues that require attention.
Understanding the reasons behind orange-colored feces helps distinguish between benign dietary changes and potential health concerns. This article explores the science behind stool pigmentation, identifies the most common triggers of orange poop, and provides practical guidance on when to monitor, adjust habits, or consult a healthcare provider.
Dietary Causes of Orange Stool
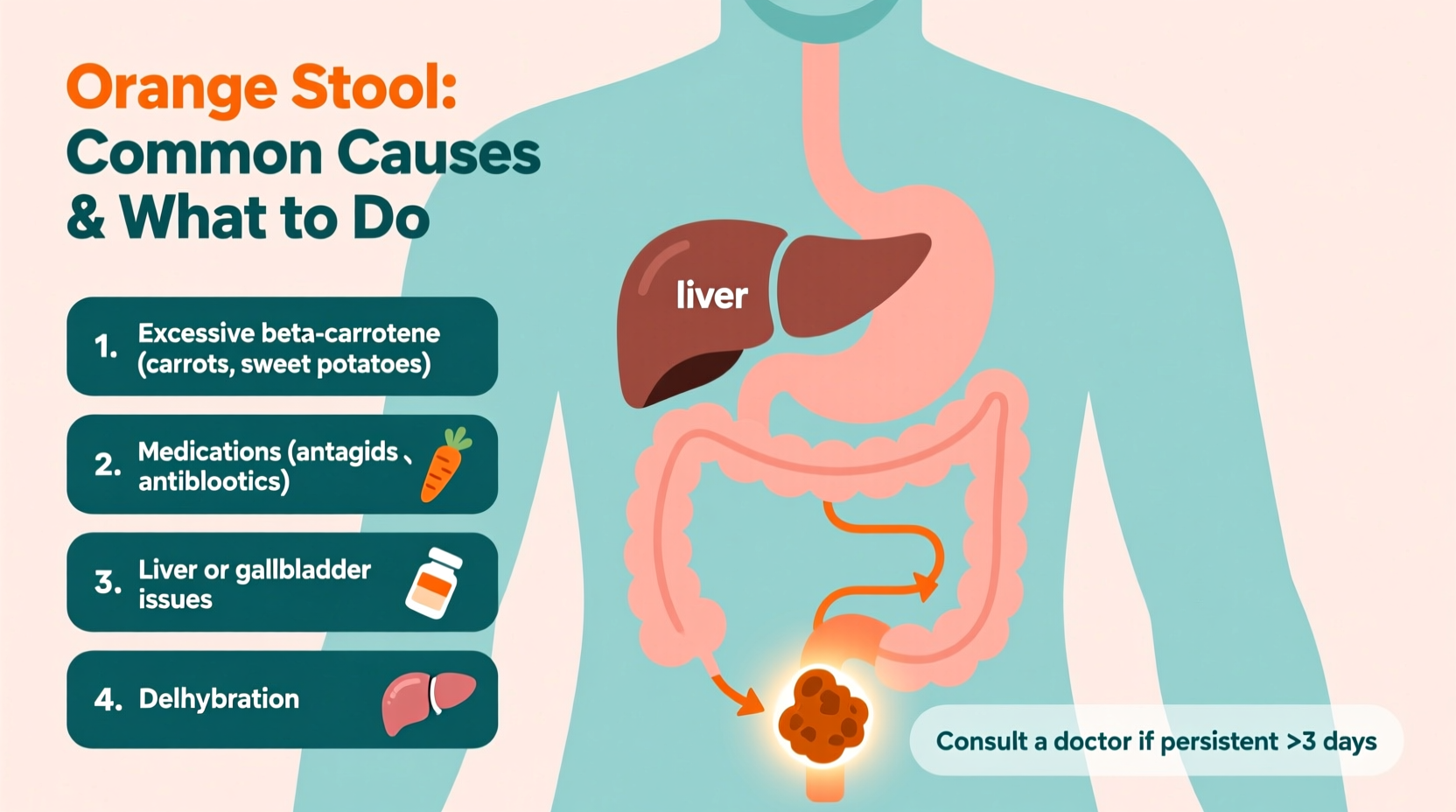
The food you eat plays the biggest role in determining stool color. Pigments from certain foods pass through your digestive tract and emerge in your bowel movements. Foods rich in beta-carotene—a natural pigment found in many orange and yellow vegetables—are the most frequent culprits behind orange poop.
Common dietary sources include:
- Carrots (especially in large quantities)
- Sweet potatoes
- Pumpkin and squash
- Mangoes and apricots
- Orange-colored breakfast cereals or snacks with artificial dyes
Beta-carotene is converted into vitamin A in the body, but excess amounts aren’t fully absorbed and are excreted through bile and stool. When consumed in high volume—such as drinking several glasses of carrot juice daily—the unmetabolized pigment can tint feces a bright or deep orange.
Supplements and Medications That Affect Stool Color
Nutritional supplements and over-the-counter medications can also alter stool appearance. Some ingredients act as strong pigments or interfere with bile processing, leading to temporary color shifts.
Common offenders include:
- Vitamin A supplements: High doses increase beta-carotene levels in the system, mimicking dietary effects.
- Iron supplements with additives: While iron typically turns stool dark or black, some formulations contain coloring agents that may contribute to unusual hues.
- Antacids and antibiotics: These can disrupt gut flora and bile metabolism, indirectly affecting color.
- Medications with dyes: Liquid or chewable forms often use FD&C Yellow or Red dyes that combine to produce an orange tint.
If you started a new supplement or medication within the past 2–3 days, review the ingredient list for artificial colors or carotenoids. Discontinuation (under medical supervision) may resolve the issue.
Liver and Gallbladder Function: The Bile Connection
Your liver produces bile, a greenish fluid stored in the gallbladder and released into the small intestine to help digest fats. As bile moves through the digestive tract, bacteria break down its components, turning it from green to brown. Any disruption in this process can result in abnormal stool colors—including orange.
When bile flow is reduced or altered, undigested bile pigments may remain more yellow-orange than usual. Conditions that affect bile production or release include:
- Gallstones blocking the bile duct
- Hepatitis or liver inflammation
- Biliary stenosis (narrowing of bile ducts)
- Fatty liver disease
In these cases, orange stool may be accompanied by other symptoms such as abdominal pain (especially in the upper right quadrant), jaundice (yellowing of skin or eyes), nausea, or pale stools alternating with orange ones.
“Stool color is a window into digestive health. Persistent orange or clay-colored stools warrant evaluation for biliary or hepatic dysfunction.” — Dr. Lena Patel, Gastroenterologist
Do’s and Don’ts: Managing Orange Stool at Home
Before jumping to conclusions, assess lifestyle factors. Use this table to evaluate possible causes and appropriate responses.
| Scenario | Do | Don't |
|---|---|---|
| You ate a lot of carrots or sweet potatoes yesterday | Monitor for 1–2 days; reduce intake temporarily | Don’t panic or stop eating vegetables entirely |
| Taking a multivitamin with high vitamin A | Check dosage against recommended daily allowance | Avoid doubling up on supplements |
| Recently started a new medication | Review side effects and speak with your pharmacist | Don’t discontinue prescribed meds without consulting your doctor |
| Experiencing pain, fatigue, or yellow skin | Schedule a medical appointment promptly | Ignore warning signs or self-diagnose serious conditions |
Step-by-Step Guide: What to Do When You Notice Orange Poop
Follow this practical timeline to determine whether orange stool is a passing event or requires further action:
- Day 1: Observe and record. Note the exact color, consistency, and any associated symptoms (cramping, bloating, urgency).
- Day 2: Review recent intake. Consider meals, supplements, and medications from the past 48 hours.
- Day 3: Adjust diet. Reduce foods high in beta-carotene and eliminate artificially colored products.
- Day 4–5: Reassess. If stool returns to brown, the cause was likely dietary. If still orange, continue monitoring.
- Day 6–7: Seek evaluation. If orange stool persists beyond a week—or if symptoms like pain, fever, or jaundice develop—consult a healthcare provider.
Real-Life Example: A Case of Carrot Overload
Mark, a 34-year-old software developer, noticed his stool had turned bright orange after two weeks of starting a “healthy detox” regimen. His daily routine included 16 oz of fresh carrot-ginger juice each morning, along with sweet potato lunches and mango smoothies. Concerned, he visited his primary care physician.
After reviewing Mark’s diet and running basic liver function tests—which came back normal—the doctor concluded the orange stool was due to excessive beta-carotene intake. Mark was advised to moderate his juice consumption and diversify his vegetable choices. Within four days of reducing carrot intake, his stool returned to a normal brown color.
This case illustrates how even well-intentioned health trends can lead to surprising bodily changes—most of which are reversible with simple adjustments.
FAQ: Common Questions About Orange Poop
Can dehydration cause orange stool?
Dehydration primarily affects stool consistency (leading to harder, darker stools), but it doesn’t directly cause an orange color. However, concentrated bile in dehydrated individuals might slightly intensify stool pigmentation. Staying hydrated supports overall digestive health, but it’s unlikely to reverse orange stool unless combined with dietary changes.
Is orange poop dangerous in babies or toddlers?
In infants and young children, orange stool is usually harmless, especially if they’re consuming pureed carrots, sweet potatoes, or formula with added vitamins. However, if it's accompanied by diarrhea, vomiting, lethargy, or poor feeding, consult a pediatrician. Rarely, bile duct issues like biliary atresia can present with light or oddly colored stools in newborns.
Does orange poop mean I have a liver problem?
Not necessarily. Liver-related issues typically cause pale, clay-colored, or gray stools due to lack of bile, rather than orange. However, early-stage disruptions in bile flow might temporarily result in orange or yellow-brown variations. If orange stool persists and is paired with fatigue, dark urine, or abdominal discomfort, liver function should be evaluated through blood tests.
Conclusion: Know Your Body, Trust Your Instincts
Occasional orange poop is usually nothing to worry about—especially if you can trace it to carrots, supplements, or brightly colored foods. The digestive system is sensitive and responsive, and stool color is one of its most visible indicators. By paying attention to patterns and accompanying symptoms, you gain valuable insight into your internal health.
Most cases resolve with minor dietary tweaks. But when in doubt, or when changes persist beyond a few days, don’t hesitate to reach out to a medical professional. Early detection of liver or gallbladder conditions can prevent complications down the line.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?