Occasional changes in bowel movements are normal, but consistently soft or mushy stools can be concerning. While not always a sign of serious illness, soft and mushy poop may indicate dietary imbalances, digestive disturbances, or underlying health conditions. Understanding the root causes and knowing when to take action helps restore gut balance and overall well-being.
Understanding Stool Consistency: The Bristol Stool Scale
The Bristol Stool Scale is a medical tool used to classify the form of human feces into seven categories. Soft and mushy stools typically fall into Types 5 and 6:
| Type | Description | Interpretation |
|---|---|---|
| 1 | Separate hard lumps, like nuts | Severe constipation |
| 2 | Sausage-shaped but lumpy | Mild constipation |
| 3 | Like a sausage with cracks on surface | Near normal |
| 4 | Smooth, soft sausage or snake | Ideal stool |
| 5 | Soft blobs with clear cut edges | Beginning of loose stool |
| 6 | Mushy, ragged edges, fluffy pieces | Mild diarrhea |
| 7 | Watery, no solid pieces | Diarrhea |
If your stools regularly appear as Type 5 or 6, it suggests faster transit through the colon, preventing adequate water absorption. This often leads to mushiness and difficulty controlling bowel movements.
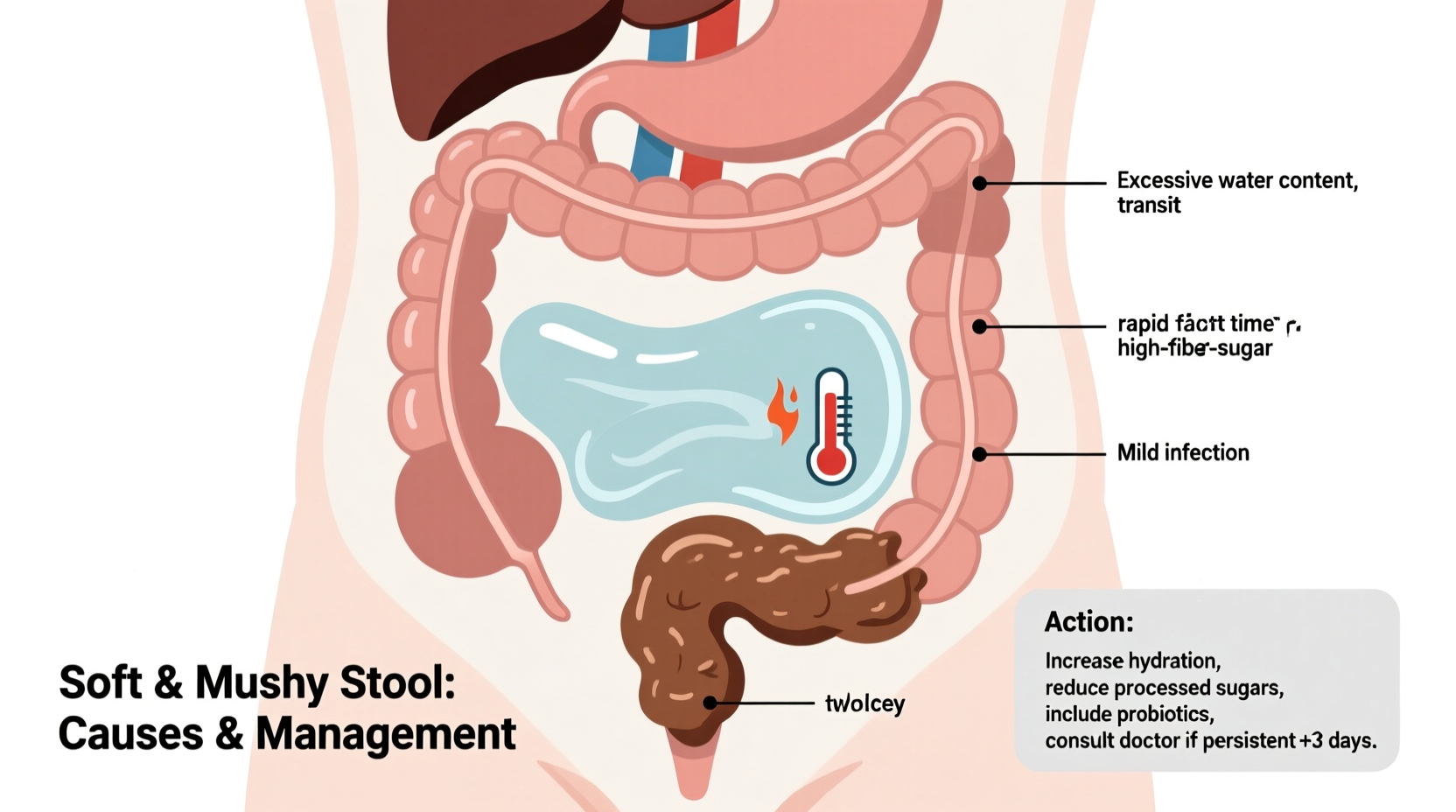
Common Causes of Soft and Mushy Stools
Several factors influence stool texture. Some are temporary; others may require long-term management.
Dietary Triggers
Foods high in fat, sugar, or artificial sweeteners (like sorbitol and xylitol) can speed up digestion and soften stools. Excessive caffeine, alcohol, and spicy foods also irritate the gut lining in sensitive individuals. A sudden increase in fiber—especially insoluble fiber from raw vegetables or bran—can cause loose stools until the gut adjusts.
Hydration Imbalance
Dehydration thickens stool, but overhydration alone doesn’t cause mushiness. However, consuming large volumes of fluids with meals, especially sugary drinks, can dilute digestive enzymes and contribute to poor digestion.
Stress and Gut-Brain Axis Disruption
The gut and brain communicate closely. Acute stress activates the “fight-or-flight” response, increasing intestinal motility and leading to softer or urgent bowel movements. Chronic stress may alter gut microbiota composition, weakening digestion over time.
Medications and Supplements
Common culprits include:
- Antibiotics (disrupt gut flora)
- Magnesium supplements
- Laxatives
- Proton pump inhibitors (PPIs)
- Metformin (for diabetes)
Underlying Digestive Conditions
Persistent soft stools may signal conditions such as:
- Irritable Bowel Syndrome (IBS): Often presents with alternating diarrhea and constipation, bloating, and cramping.
- Inflammatory Bowel Disease (IBD): Includes Crohn’s disease and ulcerative colitis, typically involving inflammation, blood in stool, and weight loss.
- Malabsorption disorders: Such as celiac disease (gluten intolerance) or lactose intolerance, where undigested food draws water into the colon.
- Bile acid malabsorption: Excess bile in the colon increases secretion of water, leading to chronic diarrhea or mushy stools.
“Frequent mushy stools should not be ignored—especially if they last more than two weeks. It’s a signal from your digestive system that something needs attention.” — Dr. Lena Patel, Gastroenterologist
What You Can Do: Practical Steps to Improve Stool Quality
Most cases of soft, mushy poop resolve with lifestyle adjustments. Here’s a structured approach:
Step 1: Evaluate Your Diet
Keep a 7-day food and symptom journal. Look for patterns linking certain foods to stool changes. Common offenders include dairy, gluten, fried foods, artificial sweeteners, and carbonated beverages.
Step 2: Balance Fiber Intake
Too much or too little fiber affects consistency. Aim for 25–30 grams daily from whole grains, fruits, vegetables, and legumes. Increase intake gradually to avoid gas and bloating. Focus on soluble fiber (oats, bananas, apples) which firms stool by absorbing water.
Step 3: Stay Hydrated—But Strategically
Drink water throughout the day, but avoid large amounts during meals to prevent diluting stomach acid. Herbal teas like chamomile or ginger may soothe digestion.
Step 4: Manage Stress
Practice mindfulness, deep breathing, or yoga. Even 10 minutes of daily meditation can reduce gut sensitivity over time.
Step 5: Replenish Gut Bacteria
After antibiotic use or prolonged digestive issues, consider probiotics. Strains like *Lactobacillus rhamnosus* and *Bifidobacterium infantis* have shown benefits in IBS-related diarrhea.
Action Checklist: Improving Stool Consistency
Use this checklist to systematically address soft, mushy stools:
- ✅ Keep a 7-day bowel and diet diary
- ✅ Reduce intake of processed sugars and artificial sweeteners
- ✅ Limit caffeine and alcohol
- ✅ Increase soluble fiber gradually
- ✅ Drink 6–8 glasses of water daily, spaced between meals
- ✅ Practice stress-reduction techniques daily
- ✅ Consider a high-quality probiotic for 4–6 weeks
- ✅ Avoid unnecessary antibiotics or antacids
- ✅ Consult a doctor if symptoms persist beyond 14 days
When to See a Doctor
While occasional soft stools are normal, seek medical evaluation if you experience:
- Persistent mushy or watery stools lasting more than two weeks
- Unintentional weight loss
- Blood or mucus in stool
- Severe abdominal pain or cramping
- Nighttime diarrhea disrupting sleep
- Fever or signs of infection
A healthcare provider may recommend tests such as stool cultures, blood work (for celiac disease), breath tests (for SIBO or lactose intolerance), or a colonoscopy if structural issues are suspected.
Mini Case Study: Recovering Digestive Balance
Mark, a 34-year-old software developer, noticed his stools had become increasingly soft and urgent over three months. He often skipped breakfast, ate fast food for lunch, and drank three energy drinks daily. After tracking his habits, he realized his symptoms flared after meals containing dairy or artificial sweeteners.
With guidance from a nutritionist, Mark eliminated processed foods, reduced caffeine, added oatmeal and bananas for soluble fiber, and began taking a daily probiotic. Within four weeks, his stool consistency improved to Type 4 on the Bristol scale. His energy levels rose, and bloating disappeared.
His case highlights how modern diets and lifestyle stressors can silently disrupt digestion—and how targeted changes yield measurable results.
Frequently Asked Questions
Is mushy poop a sign of infection?
It can be, especially if accompanied by fever, nausea, vomiting, or recent travel. Bacterial or parasitic infections (like giardia) often cause acute diarrhea. However, isolated soft stools without other symptoms are more likely due to diet or stress.
Can dehydration cause mushy stools?
No—dehydration typically causes hard, dry stools. Mushy stools result from excess water in the colon, often due to rapid transit or poor nutrient absorption. However, rehydrating with electrolyte-rich fluids (not just water) can help regulate bowel function during episodes of loose stools.
Are bananas good for soft stools?
Ripe bananas are beneficial. They contain pectin, a soluble fiber that absorbs excess fluid in the intestines and helps firm stool. Avoid unripe bananas if you’re prone to constipation, but for mushy stools, ripe ones are supportive.
Final Thoughts: Listen to Your Gut
Your bowel movements are one of the most direct indicators of digestive health. Soft and mushy poop isn’t inherently dangerous, but it shouldn’t be dismissed as “normal” if it persists. Small, consistent changes—improving diet, managing stress, staying hydrated—often make a significant difference.
If lifestyle adjustments don’t bring improvement within a few weeks, don’t hesitate to consult a healthcare professional. Early insight can prevent minor issues from becoming chronic conditions.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?