Rectal itching—also known as pruritus ani—is a surprisingly common condition that affects millions of people each year. While often not serious, persistent or severe itching around the anus can be uncomfortable, disruptive, and sometimes embarrassing. The good news is that most cases can be managed effectively with simple lifestyle changes and proper hygiene. However, knowing when to seek medical advice is crucial, especially if symptoms persist or worsen.
This guide breaks down the most common causes of rectal itching, outlines practical relief methods, and helps you recognize warning signs that warrant a visit to your healthcare provider.
Common Causes of Rectal Itching
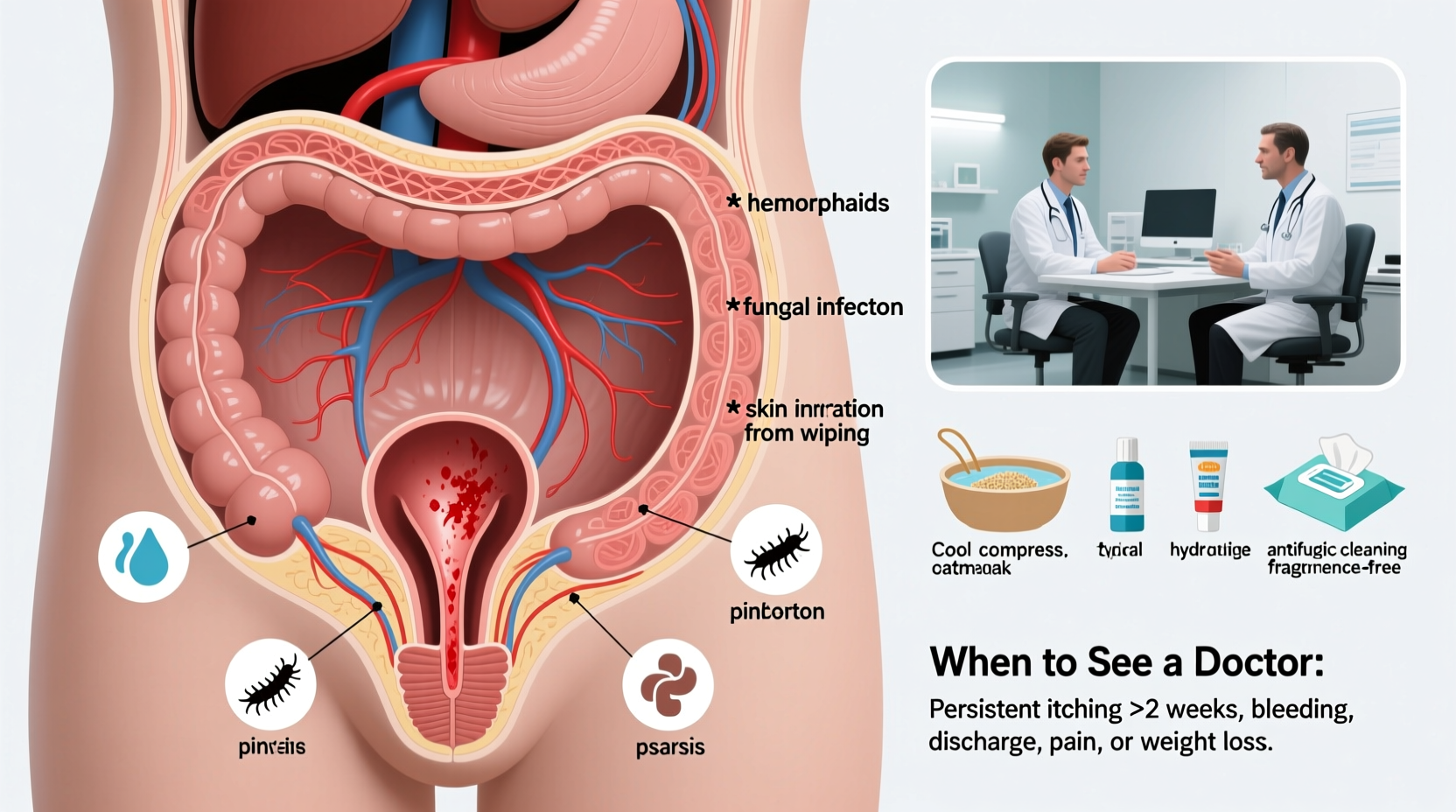
Anal itching rarely occurs without an underlying cause. Some triggers are temporary and easily addressed, while others may point to chronic conditions requiring professional care.
- Poor hygiene: Inadequate cleaning after bowel movements leaves behind stool residue, which can irritate sensitive skin.
- Excessive cleaning: Over-washing or scrubbing too hard can strip natural oils and damage the skin barrier, leading to irritation.
- Dietary factors: Spicy foods, caffeine, alcohol, citrus fruits, tomatoes, and dairy products can increase anal moisture or acidity, triggering itchiness.
- Hemorrhoids: Swollen veins in the rectum or anus can secrete mucus that irritates the surrounding skin.
- Fungal infections: Candida overgrowth thrives in warm, moist environments and commonly affects the anal region.
- Pinworms: A parasitic infection particularly common in children, causing intense nighttime itching.
- Skin conditions: Eczema, psoriasis, or contact dermatitis from soaps, wipes, or laundry detergents can affect the perianal area.
- Infections: Bacterial infections or sexually transmitted infections (STIs) like herpes or HPV may present with anal itching.
- Chronic diarrhea or constipation: Both can lead to skin irritation due to repeated wiping or straining.
Effective Relief Strategies at Home
For mild or occasional itching, self-care measures often provide quick relief. The goal is to reduce irritation, keep the area dry, and restore skin health.
- Practice gentle hygiene: After bowel movements, clean with water using a peri-bottle or bidet. Pat dry gently with a soft towel—never rub.
- Avoid scratching: Scratching damages the skin, increases inflammation, and can introduce bacteria, leading to infection.
- Use plain, unscented toilet paper: Or better yet, switch to fragrance-free, alcohol-free moist wipes designed for sensitive skin.
- Wear loose, breathable clothing: Cotton underwear and loose-fitting pants help reduce moisture buildup.
- Apply a protective barrier cream: Zinc oxide or petroleum jelly can shield irritated skin from further exposure to moisture and fecal matter.
- Modify your diet: Eliminate potential irritants like spicy foods, coffee, beer, and acidic fruits for a few days to see if symptoms improve.
- Take sitz baths: Soak the area in warm (not hot) water for 15–20 minutes daily to soothe irritation and promote healing.
Step-by-Step Daily Routine for Relief
| Time | Action | Purpose |
|---|---|---|
| Morning & Night | Gentle cleansing with water, pat dry | Prevent residue buildup without irritating skin |
| After Bowel Movement | Rinse with peri-bottle, use soft wipe if needed | Minimize friction and chemical exposure |
| Once Daily | 15-minute sitz bath | Reduce inflammation and cleanse gently |
| As Needed | Apply zinc oxide ointment | Create protective moisture barrier |
When to See a Doctor
Most cases of anal itching resolve within a few days with home care. However, persistent or worsening symptoms should not be ignored. Seek medical evaluation if:
- The itching lasts longer than 2–3 weeks despite self-care.
- You notice bleeding, discharge, lumps, or pain in the anal area.
- There are signs of infection—increased redness, warmth, swelling, or pus.
- You suspect pinworms, especially in children with nighttime itching.
- You have a history of inflammatory bowel disease (IBD), HIV, or STIs.
“Persistent pruritus ani should never be dismissed as just ‘bad hygiene.’ It can be a sign of underlying gastrointestinal, infectious, or dermatological conditions.” — Dr. Lena Torres, Gastroenterologist
Mini Case Study: Resolving Chronic Itching
James, a 42-year-old office worker, experienced recurring anal itching for over two months. He initially tried medicated wipes and anti-itch creams, but symptoms worsened. After avoiding spicy foods and switching to cotton underwear, he saw slight improvement. However, when he developed small painful fissures, he consulted a proctologist. Testing revealed a fungal infection and early-stage hemorrhoids. With antifungal treatment, dietary adjustments, and sitz baths, his symptoms resolved within three weeks. This case highlights how overlapping causes require accurate diagnosis and targeted therapy.
Do’s and Don’ts: Quick Reference Table
| Do’s | Don’ts |
|---|---|
| Use water to clean the area | Scratch the itchy area |
| Wear cotton underwear | Use scented soaps or wipes |
| Apply barrier ointments | Wear tight synthetic clothing |
| Stay hydrated and eat fiber-rich foods | Ignore bleeding or pain |
| See a doctor if symptoms persist | Self-treat with steroid creams long-term |
Frequently Asked Questions
Can hemorrhoids cause rectal itching?
Yes. Internal or external hemorrhoids often secrete mucus that irritates the delicate skin around the anus. Treating the hemorrhoids—through diet, hydration, or medical procedures—usually reduces the associated itching.
Are over-the-counter creams safe for long-term use?
Some OTC creams containing hydrocortisone can provide short-term relief, but prolonged use (beyond one to two weeks) can thin the skin and worsen symptoms. Always consult a doctor before using steroid-based treatments near the anus.
Can stress make rectal itching worse?
Indirectly, yes. Stress can exacerbate digestive issues like irritable bowel syndrome (IBS), which may lead to diarrhea or constipation—both contributing to anal irritation. Additionally, stress can heighten sensitivity to discomfort.
Conclusion: Take Control of Your Comfort
Rectal itching is more than just a minor annoyance—it can significantly impact your quality of life. The key to managing it lies in identifying the cause, adopting gentle hygiene practices, and making smart lifestyle adjustments. Most cases respond well to simple changes, but don’t hesitate to seek medical advice if symptoms persist or escalate. Early intervention prevents complications and ensures you get the right treatment.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?