Brown semen can be alarming the first time it’s noticed. While occasional changes in semen color are often harmless, a brown or reddish tint may indicate an underlying condition that requires attention. Semen typically appears milky white or gray, so any significant shift—especially toward brown—warrants understanding. This article explores the physiological reasons behind discolored semen, identifies potential causes, and outlines when medical evaluation is necessary.
Understanding Semen Composition and Color Variation
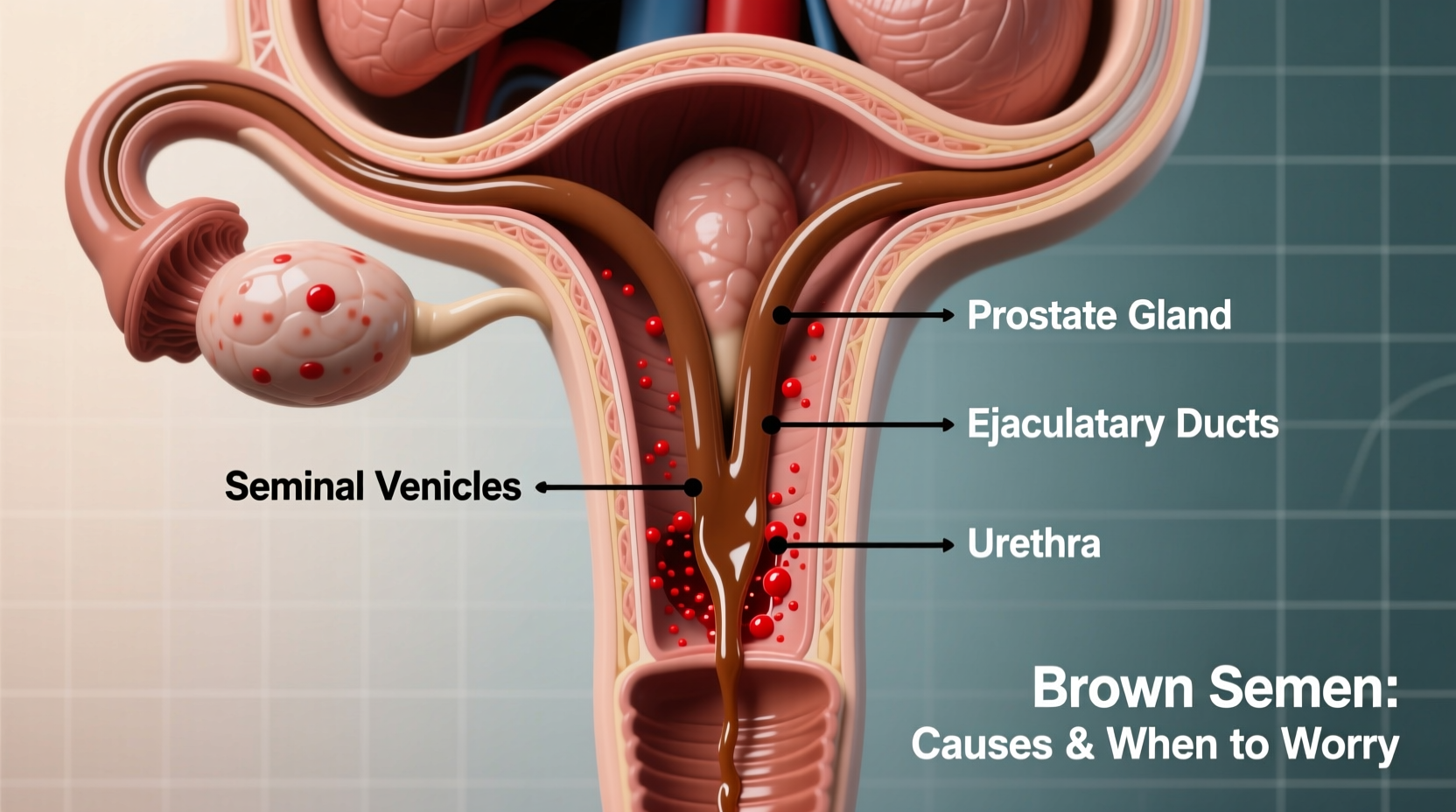
Semen is a complex fluid composed of sperm and secretions from the prostate gland, seminal vesicles, and bulbourethral glands. Its usual milky appearance comes from proteins, enzymes, and other compounds that support sperm viability. Minor variations in color due to diet, hydration, or frequency of ejaculation are normal. However, brown or pink semen suggests the presence of blood—a condition known as hematospermia.
Hematospermia occurs when blood mixes with semen during ejaculation. The blood may originate from the prostate, seminal vesicles, urethra, or epididymis. Fresh blood appears red, but older blood oxidizes and turns brown, which explains the darker hue. In most cases, especially among men under 40, hematospermia resolves on its own without treatment. Still, persistent or recurrent episodes should not be ignored.
Common Causes of Brown Semen
Several factors can lead to brown semen. Some are benign and temporary; others require prompt medical assessment. Below are the most frequent causes:
- Inflammation or infection: Prostatitis (prostate inflammation), urethritis (urethra infection), or epididymitis (epididymis swelling) can cause minor bleeding into the reproductive tract.
- Recent medical procedures: Biopsies, cystoscopies, or vasectomies may result in temporary blood in semen.
- Sexual activity: Vigorous intercourse or prolonged abstinence followed by ejaculation can irritate tissues and lead to trace bleeding.
- Stones or obstructions: Calcifications in the prostate or seminal vesicles may erode tissue and cause bleeding.
- Trauma: Injury to the pelvic region or genitals can introduce blood into the ejaculate.
“While hematospermia is often self-limiting, persistent discoloration beyond a few weeks should prompt urological evaluation.” — Dr. Alan Pierce, Urologist and Men's Health Specialist
When to Be Concerned: Red Flags and Risk Factors
Most cases of brown semen in younger men are isolated and resolve within a few weeks. However, certain signs suggest a more serious underlying issue. These include:
| Symptom | Low Concern | High Concern |
|---|---|---|
| Duration | 1–3 occurrences, resolves quickly | Persists beyond 4 weeks |
| Pain | None or mild discomfort | Severe pelvic, testicular, or urinary pain |
| Urinary Symptoms | Absent | Frequent urination, urgency, burning |
| Age | Under 40 | Over 45, especially with family history of prostate issues |
| Fever or Chills | No | Yes – suggests infection |
Men over 45 or those with a history of genitourinary conditions should take brown semen more seriously. Persistent hematospermia in this group may be linked to chronic prostatitis, benign prostatic hyperplasia (BPH), or, rarely, prostate or seminal vesicle tumors.
Diagnostic Process and Medical Evaluation
If brown semen persists beyond a few weeks or is accompanied by other symptoms, a visit to a urologist is recommended. The diagnostic process typically includes:
- Medical history review: The doctor will ask about sexual activity, recent procedures, trauma, and associated symptoms.
- Physical examination: A digital rectal exam (DRE) may be performed to assess the prostate.
- Urine and semen analysis: Tests can detect infection, white blood cells, or abnormal cells.
- Imaging: Transrectal ultrasound (TRUS) may be used to visualize the prostate and seminal vesicles.
- Blood tests: PSA (prostate-specific antigen) levels may be checked, particularly in older patients.
In many cases, no specific cause is found, and the condition resolves spontaneously. When an infection is identified, antibiotics are prescribed. For inflammatory conditions, anti-inflammatory medications or alpha-blockers may help relieve symptoms.
Mini Case Study: Recurrent Hematospermia in a 38-Year-Old Man
A 38-year-old male presented with brown semen recurring over six weeks. He reported no pain, fever, or urinary symptoms. Initial urine cultures were negative. A transrectal ultrasound revealed small calcifications in the seminal vesicles. After a course of antibiotics targeting chronic prostatitis and lifestyle adjustments—including reduced alcohol intake and stress management—the symptom resolved completely within two months. Follow-up showed no recurrence after one year.
This case illustrates that even without acute infection, low-grade inflammation can contribute to hematospermia and respond well to targeted treatment.
Action Plan: What You Should Do Now
If you’ve noticed brown semen, follow this checklist to determine your next steps:
- Monitor how many times it occurs over the next 2–3 weeks.
- Check for additional symptoms: pain, fever, urinary changes.
- Recall any recent procedures, infections, or injuries.
- Avoid excessive sexual activity or masturbation temporarily.
- Schedule a urology appointment if it persists beyond a month.
Do’s and Don’ts When Dealing with Brown Semen
| Do’s | Don’ts |
|---|---|
| Stay hydrated and maintain good hygiene | Ignore persistent symptoms beyond 4 weeks |
| Keep a symptom journal (frequency, color, pain) | Self-medicate with antibiotics or supplements without advice |
| Seek evaluation if over 45 or have risk factors | Assume it’s always cancer or a severe disease |
| Practice safe sex to prevent STIs | Delay seeing a doctor due to embarrassment |
Frequently Asked Questions
Can sexually transmitted infections (STIs) cause brown semen?
Yes. STIs like gonorrhea or chlamydia can cause urethritis, leading to inflammation and bleeding into the semen. If you’re sexually active and notice discolored semen along with discharge or painful urination, get tested for STIs promptly.
Is brown semen a sign of cancer?
In rare cases, yes—but it’s uncommon, especially in younger men. Persistent hematospermia in men over 45 may prompt further investigation for prostate, bladder, or seminal vesicle cancers. However, most cases are due to benign causes. Elevated PSA levels or abnormal imaging would raise suspicion.
Will brown semen affect fertility?
Occasional hematospermia does not typically impact fertility. However, if the underlying cause is chronic infection or obstruction, it could interfere with sperm transport or function. Treating the root condition usually restores normal semen parameters.
Final Thoughts and Next Steps
Brown semen is more common than many realize and often resolves without intervention. The key is awareness and timely action. While it’s natural to feel anxious, remember that most causes are treatable and not life-threatening. Ignoring persistent symptoms, however, can delay diagnosis of conditions that benefit from early management.
Your reproductive and urinary health matters. If brown semen continues beyond a few weeks or is accompanied by discomfort, don’t hesitate to consult a healthcare provider. Open conversations with your doctor lead to better outcomes and peace of mind.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?