If you've noticed small red bumps, pustules, or persistent irritation forming around your mouth—especially along the creases of your lips or on the chin—it can be both frustrating and confusing. Unlike typical acne, breakouts in this area often resist standard treatments and may worsen with harsh products. This specific pattern of inflammation has several potential causes, ranging from skincare habits to underlying skin conditions like perioral dermatitis. Understanding what’s really behind the flare-up is the first step toward clear, healthy skin.
Common Causes of Breakouts Around the Mouth
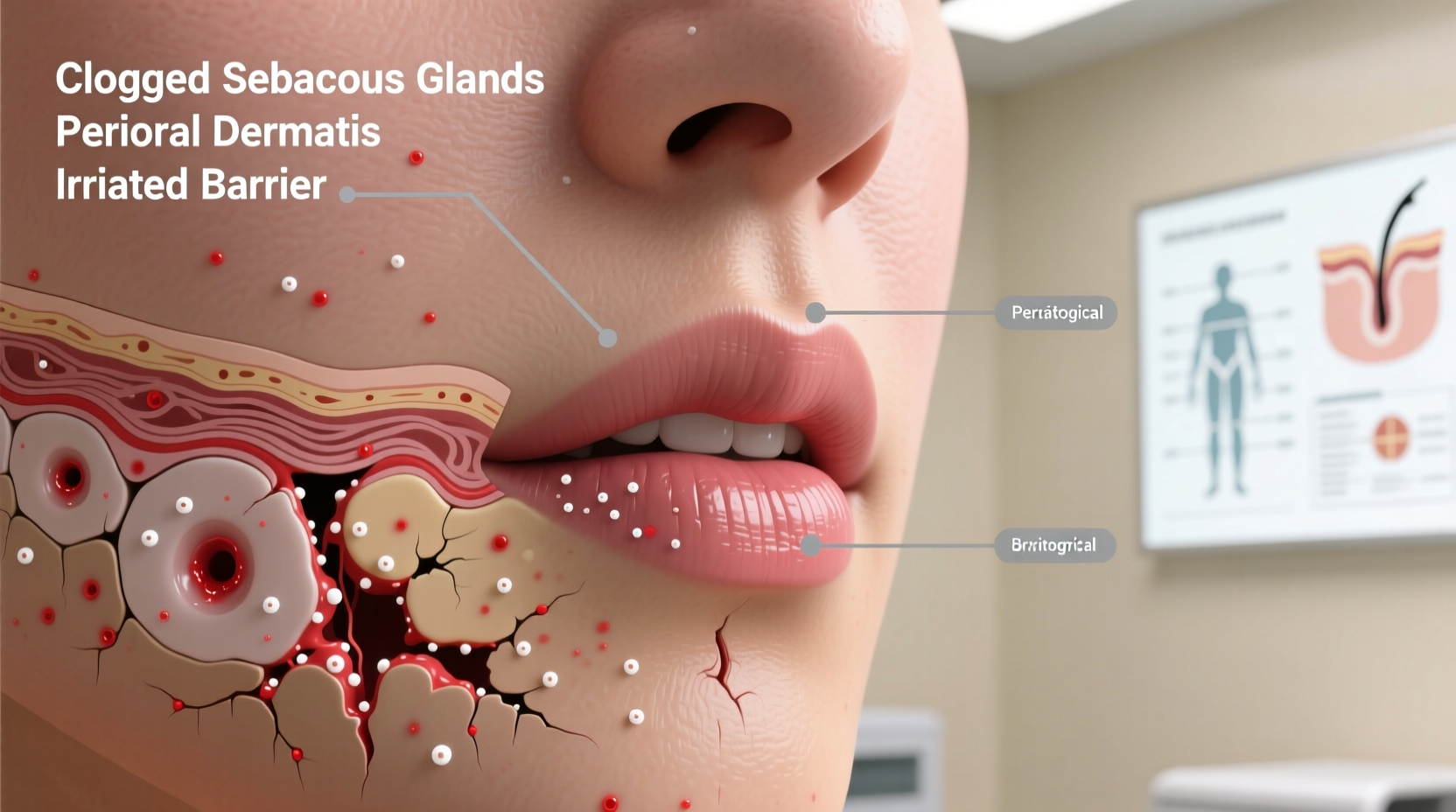
The skin around the mouth is delicate and highly reactive. It's exposed to food residues, lip products, toothpaste ingredients, and frequent touching—all of which can trigger irritation or inflammation. The most frequent culprits include:
- Perioral dermatitis: A rash-like condition causing red, bumpy eruptions around the mouth, sometimes spreading to the nose or eyes.
- Irritant contact dermatitis: Caused by exposure to irritating substances such as fluoride in toothpaste, cinnamon flavoring, or heavy moisturizers.
- Folliculitis: Inflammation of hair follicles due to bacteria, yeast, or friction.
- Hormonal acne: Often appears on the lower face and jawline, especially during menstrual cycles or stress periods.
- Lip balm or cosmetic overuse: Occlusive products like petroleum jelly or thick balms can clog pores when applied too close to the mouth.
Unlike acne vulgaris (common pimples), many of these conditions don’t respond well to traditional acne treatments—and some may even get worse with them. For example, topical steroids can initially calm symptoms but often lead to rebound flares if used long-term.
“Perioral dermatitis is frequently misdiagnosed as acne. Patients end up using harsh scrubs and benzoyl peroxide, which only aggravate the barrier and prolong healing.” — Dr. Lena Torres, Board-Certified Dermatologist
How to Identify What You're Dealing With
Accurate identification is crucial because treatment varies significantly based on the root cause. Here’s a breakdown of key differences:
| Condition | Symptoms | Triggers | Treatment Approach |
|---|---|---|---|
| Perioral Dermatitis | Small red bumps, mild burning or itching, no blackheads, spares the lip border | Steroid creams, heavy moisturizers, fluoridated toothpaste, humidity | Stop irritants, gentle skincare, prescription anti-inflammatories |
| Hormonal Acne | Painful cysts or pustules along jawline and chin, may flare monthly | Androgen fluctuations, stress, diet, dairy | Topical retinoids, hormonal therapy, oral antibiotics if severe |
| Irritant Contact Dermatitis | Redness, dryness, peeling, stinging after product use | Toothpaste, lip products, fragranced cleansers | Remove trigger, repair skin barrier, avoid further exposure |
| Folliculitis | Pimple-like bumps centered on hair follicles, may have pus | Shaving, tight clothing, bacterial or fungal overgrowth | Antimicrobial washes, antifungal creams, improved hygiene |
One telltale sign of perioral dermatitis is that the skin immediately surrounding the lips remains unaffected—a feature known as the \"perilabial sparing.\" If your breakout stops right at the edge of your vermilion border (the colored part of your lip), that’s a strong indicator.
Step-by-Step Guide to Healing Your Skin
Whether you're dealing with perioral dermatitis or another form of irritation, recovery requires consistency and patience. Most cases take 4–8 weeks to improve, especially once you eliminate contributing factors. Follow this timeline for best results:
- Week 1: Strip down your routine
Stop all non-essential skincare. Use only a fragrance-free, soap-free cleanser and lukewarm water. Avoid exfoliants, acids, retinoids, and heavy creams near the mouth. - Switch to fluoride-free toothpaste
Fluoride and sodium lauryl sulfate (SLS) are common irritants. Opt for a natural, SLS-free version without mint or cinnamon flavoring. - Stop using lip balms and ointments
Even “soothing” products like petroleum jelly can trap moisture and block pores. Let the area breathe unless medically advised otherwise. - Week 2–3: Introduce barrier support
Once initial redness begins to calm, apply a minimal, non-comedogenic moisturizer (e.g., ceramide-based). Avoid anything greasy or occlusive. - Consult a dermatologist if no improvement
If there’s little change after three weeks, seek professional diagnosis. Prescription options like low-dose doxycycline (anti-inflammatory dose) or topical metronidazole may be necessary. - Week 4+: Maintain and prevent relapse
Gradually reintroduce products one at a time. Prioritize simplicity. Protect against UV exposure with mineral sunscreen applied away from the mouth line.
Avoid picking or scrubbing the area. Physical trauma delays healing and increases the risk of post-inflammatory hyperpigmentation, especially in darker skin tones.
Real-Life Example: Sarah’s Recovery Journey
Sarah, a 29-year-old graphic designer, began noticing tiny red bumps forming around her mouth after switching to a new nighttime moisturizer. She assumed it was acne and started using salicylic acid wipes twice daily. Within two weeks, the rash had spread, with intense stinging after every application.
After visiting a dermatologist, she was diagnosed with perioral dermatitis triggered by both the rich night cream and her mint-flavored toothpaste. Her treatment plan included:
- Discontinuing all facial products except a gentle cleanser
- Using a fluoride-free, flavorless toothpaste
- Taking a low-dose course of doxycycline for six weeks
- Applying a non-steroidal topical (ivermectin 1%) to reduce inflammation
By week five, her skin showed significant improvement. Today, she maintains a minimalist routine and avoids scented lip products entirely. “I learned that more isn’t always better,” she says. “Sometimes healing means doing less.”
Daily Care Checklist for Clearer Skin
Use this checklist to stay on track during recovery and beyond:
- ✅ Wash face with lukewarm water and gentle, fragrance-free cleanser
- ✅ Rinse thoroughly after brushing teeth to remove residue
- ✅ Use a clean towel—don’t rub, pat dry gently
- ✅ Apply medication or moisturizer with clean fingertips
- ✅ Avoid touching face throughout the day
- ✅ Replace pillowcases every 3–4 days
- ✅ Monitor for signs of recurrence: redness, tingling, new bumps
- ✅ Reintroduce products slowly—one every 7–10 days
Prevention: Long-Term Habits That Work
Once your skin clears, maintaining results depends on consistent habits. The goal is to protect the skin barrier while avoiding known irritants. Consider these preventive strategies:
- Choose non-comedogenic lip products: Look for labels like “non-acnegenic” or “oil-free.” Avoid lanolin, paraffin, and beeswax-heavy formulas.
- Limit facial mists and sprays: Many contain alcohol or fragrance that can drip into the mouth area and cause flare-ups.
- Be mindful of phone and mask hygiene: Phones collect oils and bacteria. Clean regularly with alcohol wipes. Change cloth masks frequently.
- Stay hydrated and manage stress: Internal health impacts skin resilience. Chronic stress can elevate cortisol, triggering inflammation.
- Evaluate your diet: Some studies suggest high-sugar diets and dairy intake may exacerbate facial rashes in sensitive individuals.
It’s also wise to reevaluate any steroid-containing creams used on the face—even hydrocortisone from the drugstore should not be used around the mouth for more than a few days without medical supervision.
Frequently Asked Questions
Can I wear makeup while treating breakouts around my mouth?
You can, but choose carefully. Use non-comedogenic, mineral-based foundations and avoid liquid concealers that may seep into pores. Always remove makeup gently with a micellar water or oil-free wipe. Never sleep with makeup on during active flare-ups.
Is perioral dermatitis contagious?
No, it is not an infection and cannot be spread through contact. However, sharing items like lip balm, towels, or makeup brushes is still unwise, as they can harbor bacteria that worsen skin imbalance.
How long does it take to heal?
With proper care, most people see improvement within 4–6 weeks. Full resolution may take up to 12 weeks, especially if steroids were previously used. Patience and adherence to a simplified routine are essential.
Take Control of Your Skin Health
Breakouts around the mouth are more than just a cosmetic concern—they signal that your skin barrier is under stress. While the urge to aggressively treat them is strong, the real solution often lies in restraint: removing irritants, simplifying routines, and allowing time for healing. Armed with the right knowledge, you can identify the root cause and respond effectively, rather than cycling through products that make things worse.
True skin transformation starts with understanding. Whether it’s switching toothpaste, ditching heavy balms, or seeking expert guidance, each small action builds toward lasting clarity. Don’t underestimate the power of gentle care—sometimes, the kindest thing you can do for your skin is simply leave it alone.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?