Soft stool is a common digestive occurrence that many people experience from time to time. While occasional changes in bowel consistency are normal, consistently soft stool can be concerning—especially if it persists for weeks or is accompanied by other symptoms. Understanding the underlying causes, recognizing red flags, and knowing when to consult a healthcare provider are essential steps toward maintaining optimal gut health.
Bowel movements vary widely among individuals, but the Bristol Stool Scale—a clinical tool used to classify stool into seven types—identifies Types 5 and 6 as soft blobs or mushy, watery stools. If your stool regularly falls into these categories without progressing to diarrhea, it may indicate an ongoing digestive imbalance.
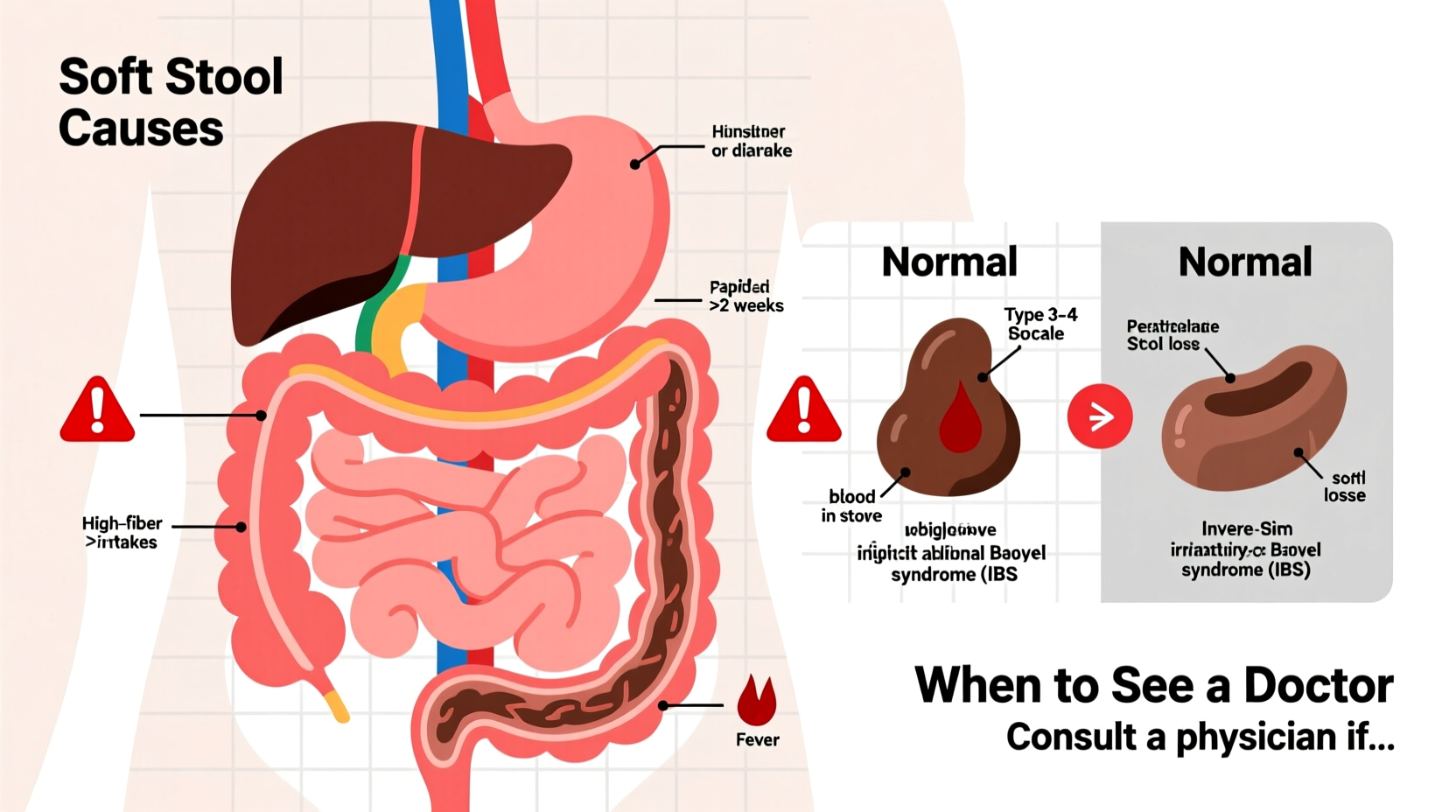
Common Causes of Consistently Soft Stool
Several factors influence stool consistency, including diet, hydration, gut microbiota, and overall digestive function. The most frequent non-medical reasons for soft stool include:
- Dietary habits: High intake of insoluble fiber (found in raw vegetables, whole grains), fatty foods, or artificial sweeteners like sorbitol and xylitol can loosen stool.
- Hydration levels: Drinking excessive fluids, particularly with meals, may reduce stool firmness.
- Caffeine and alcohol: Both act as mild laxatives and can increase intestinal motility, leading to softer stools.
- Stress and anxiety: The gut-brain axis means emotional stress can directly affect bowel movements, often resulting in looser stool.
- Recent dietary changes: Sudden increases in fruit, vegetable, or dairy consumption can temporarily alter stool texture.
In many cases, adjusting lifestyle habits can normalize bowel movements within a few days.
Medical Conditions Linked to Chronic Soft Stool
When soft stool persists beyond a few weeks despite dietary adjustments, an underlying medical condition may be involved. Some common gastrointestinal disorders associated with ongoing soft stool include:
- Irritable Bowel Syndrome (IBS): Particularly IBS-D (diarrhea-predominant), where soft stool or loose bowel movements occur frequently, often with bloating or abdominal pain.
- Small Intestinal Bacterial Overgrowth (SIBO): An overgrowth of bacteria in the small intestine interferes with fat absorption, leading to greasy, soft stools.
- Lactose intolerance: Inability to digest lactose results in gas, bloating, and soft or loose stools after consuming dairy.
- Celiac disease: An autoimmune reaction to gluten damages the small intestine, causing malabsorption and chronic soft stool.
- Chronic pancreatitis: Reduced production of digestive enzymes impairs fat breakdown, resulting in pale, oily, foul-smelling soft stools (steatorrhea).
- Bile acid malabsorption: Excess bile acids reaching the colon stimulate water secretion, causing soft or watery stools.
These conditions often require diagnostic testing such as blood work, stool analysis, breath tests, or endoscopy for confirmation.
When to Worry: Red Flags Requiring Medical Attention
While soft stool alone isn’t necessarily dangerous, certain accompanying symptoms should prompt immediate evaluation by a healthcare provider. These warning signs suggest a more serious issue:
| Symptom | Possible Implication | Action Required |
|---|---|---|
| Unintentional weight loss | Malignancy, malabsorption, chronic inflammation | See doctor within 1–2 weeks |
| Blood in stool (bright red or dark) | Hemorrhoids, colitis, polyps, colorectal cancer | Seek urgent evaluation |
| Fever or chills | Infection or inflammatory bowel disease (IBD) | Contact provider immediately |
| Nighttime diarrhea | IBD, infection, or systemic illness | Requires diagnostic workup |
| Family history of colon cancer or IBD | Increased risk for hereditary conditions | Discuss screening options early |
“Persistent changes in bowel habits lasting more than four weeks warrant investigation—even in young, otherwise healthy individuals.” — Dr. Lena Torres, Gastroenterologist, Cleveland Clinic
Step-by-Step Guide to Managing Soft Stool at Home
If your soft stool isn't linked to alarming symptoms, you can take proactive steps to improve digestive stability. Follow this timeline to assess and address the issue:
- Week 1: Monitor and Record
- Keep a daily log of food, fluid intake, stress levels, and bowel movements.
- Note timing, consistency, color, and any discomfort.
- Week 2: Adjust Diet
- Reduce intake of high-FODMAP foods (onions, garlic, beans, apples) if bloating accompanies soft stool.
- Limit caffeine, alcohol, and artificial sweeteners.
- Increase soluble fiber (oats, bananas, psyllium) to add bulk.
- Week 3: Evaluate Response
- If improvement occurs, continue current habits.
- If no change, eliminate one suspected trigger (e.g., dairy) for five days to test tolerance.
- Week 4: Seek Professional Help
- If symptoms persist, schedule an appointment with a primary care physician or gastroenterologist.
- Be prepared to share your symptom diary and list of medications/supplements.
Real-Life Example: Sarah’s Experience with Persistent Soft Stool
Sarah, a 34-year-old teacher, noticed her stool had been soft for nearly two months. She didn’t have pain or weight loss, but felt frustrated by the lack of consistency. After tracking her diet, she realized she was drinking three large smoothies daily—packed with spinach, almond milk, and protein powder containing sugar alcohols.
She eliminated the smoothies and replaced them with balanced meals rich in complex carbohydrates and lean protein. Within ten days, her stool firmed up significantly. A follow-up visit with her doctor confirmed no underlying condition, and Sarah now maintains a moderate approach to fiber-rich beverages.
This case highlights how seemingly healthy habits can unintentionally disrupt digestion.
Checklist: When to See a Doctor About Soft Stool
Use this checklist to determine whether professional evaluation is needed:
- ✅ Soft stool has lasted longer than 4 weeks
- ✅ You’ve made dietary changes with no improvement
- ✅ There’s unexplained fatigue or weakness
- ✅ Abdominal pain worsens after eating
- ✅ You’re over age 50 or have a family history of colon cancer
- ✅ Stool floats consistently or has an oily film
- ✅ You experience nausea or vomiting alongside bowel changes
If two or more items apply, schedule a medical consultation.
Frequently Asked Questions
Can probiotics help with soft stool?
Yes, certain strains like Lactobacillus rhamnosus GG and Saccharomyces boulardii may help regulate bowel movements, especially if soft stool follows antibiotic use or travel. However, some people report increased gas or looser stools initially. Start with a low dose and monitor effects.
Is soft stool the same as diarrhea?
Not exactly. Diarrhea is defined as three or more loose or watery stools per day lasting less than two weeks (acute) or more than four weeks (chronic). Soft stool refers to form rather than frequency—many people pass soft but formed stool once daily without meeting criteria for diarrhea.
Can medications cause soft stool?
Absolutely. Common culprits include antibiotics, proton pump inhibitors (like omeprazole), metformin (for diabetes), and magnesium-containing supplements or antacids. Review all medications with your doctor if bowel changes began after starting a new prescription.
Take Control of Your Digestive Health
Consistently soft stool is more than just a minor inconvenience—it can be a signal from your body that something needs attention. While many cases resolve with simple dietary and lifestyle adjustments, ignoring persistent changes can delay diagnosis of treatable conditions. By paying attention to patterns, eliminating potential triggers, and knowing when to seek help, you empower yourself to maintain long-term digestive wellness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?