Noticing a change in stool color can be alarming, especially when it turns black and sticky like tar. While occasional changes may result from diet or medication, black, tarry stools—medically known as melena—are often a warning sign of bleeding in the upper gastrointestinal (GI) tract. Understanding the underlying causes, recognizing associated symptoms, and knowing when to act can make a critical difference in your health outcome.
What Does Black and Tarry Stool Mean?
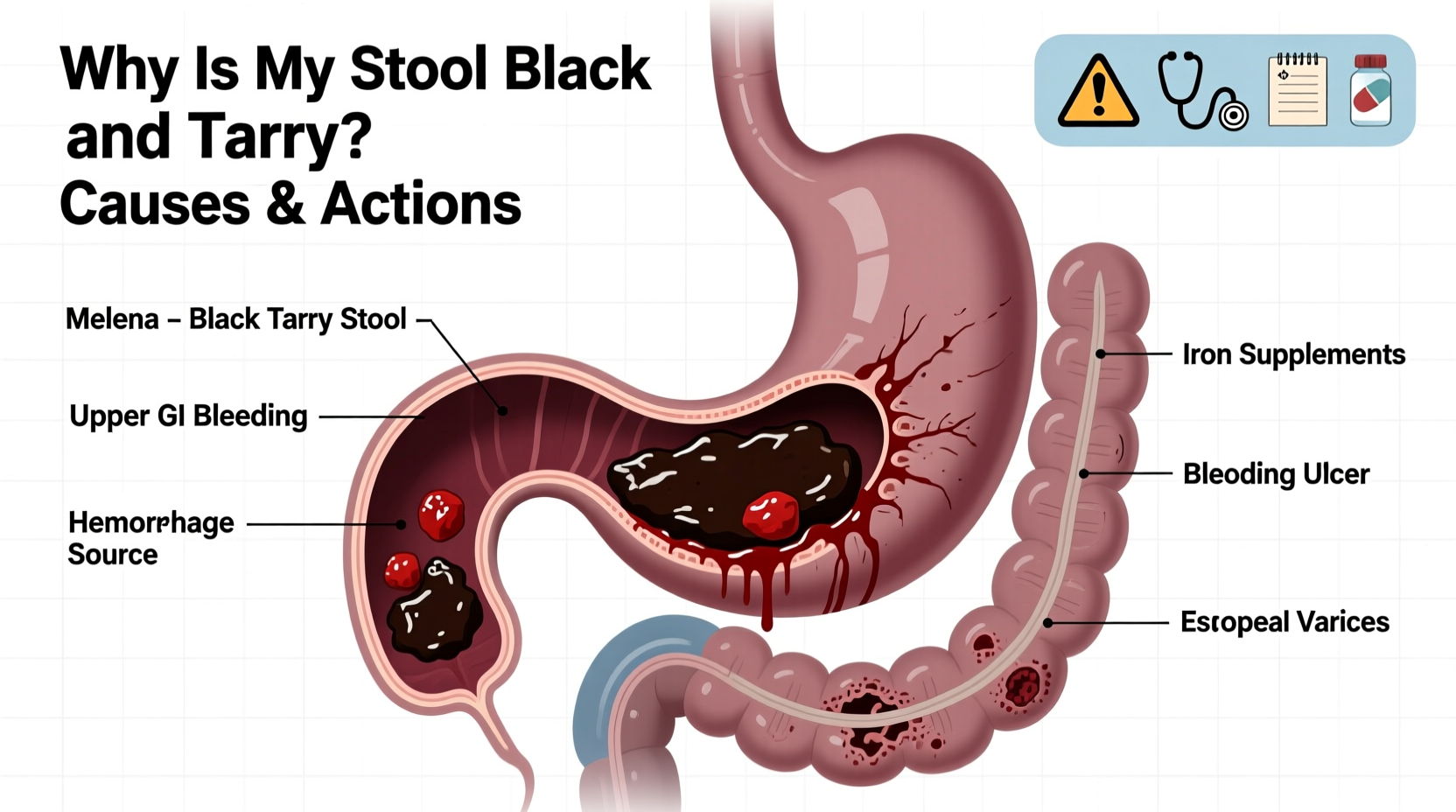
Melena refers to dark, glossy, foul-smelling stools that resemble tar. This appearance results from the digestion of blood in the stomach or small intestine. Unlike bright red blood in stool—which typically indicates lower GI bleeding—black, tarry stool suggests bleeding higher up in the digestive system, such as the esophagus, stomach, or duodenum.
The dark color occurs because hemoglobin, the protein in red blood cells, breaks down when exposed to digestive enzymes and acid. As blood travels through the intestines, it becomes altered, resulting in the characteristic black hue and sticky consistency.
“Melena is never normal. It’s a clinical red flag that requires prompt evaluation.” — Dr. Alan Reyes, Gastroenterologist, Cleveland Clinic
Common Causes of Black and Tarry Stools
Several conditions can lead to melena. Some are benign and temporary, while others are potentially life-threatening. The most frequent causes include:
- Peptic ulcers: Open sores in the lining of the stomach or duodenum, often caused by H. pylori infection or prolonged use of NSAIDs like ibuprofen or aspirin.
- Gastritis or esophagitis: Inflammation of the stomach or esophageal lining, which can erode blood vessels and cause bleeding.
- Esophageal varices: Enlarged veins in the esophagus, commonly seen in people with liver cirrhosis. These veins are fragile and prone to rupture.
- Mallory-Weiss tears: Small tears in the esophagus from violent vomiting, which may bleed enough to cause melena.
- Gastrointestinal tumors: Stomach or small intestine cancers can ulcerate and bleed over time.
- Medications: Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, or anticoagulants increases the risk of GI bleeding.
Dietary and Medicinal Mimics: Not Always Blood
Not all black stools indicate internal bleeding. Certain foods and supplements can discolor stool without posing a health threat. It's important to differentiate harmless causes from dangerous ones.
| Cause | Appearance | Clues It’s Not Melena |
|---|---|---|
| Iron supplements | Dark gray or black | No stickiness; stops after discontinuing iron |
| Bismuth-containing meds (e.g., Pepto-Bismol) | Jet black | Often accompanied by blackened tongue; resolves in 1–2 days |
| Blueberries, black licorice, or dark beets | Dark but not tarry | Stool remains soft and non-sticky; recent dietary intake |
| Activated charcoal | Charcoal black | Used intentionally for detox or gas; no other symptoms |
If you've recently taken Pepto-Bismol or started an iron regimen, the discoloration may be harmless. However, if the stool is sticky, foul-smelling, and persists beyond a day or two after stopping these substances, medical evaluation is essential.
When to Seek Immediate Medical Attention
Black, tarry stool combined with certain symptoms can indicate significant internal bleeding. Delaying care may lead to complications such as anemia, hypotension, or shock.
Seek emergency medical help if you experience:
- Dizziness or lightheadedness
- Rapid heart rate (tachycardia)
- Low blood pressure
- Vomiting blood (which may look like coffee grounds)
- Abdominal pain or bloating
- Fatigue or shortness of breath
- Pale skin or cold extremities
“I once treated a 58-year-old patient who dismissed his black stools as ‘something I ate.’ He was later diagnosed with a bleeding gastric ulcer and required hospitalization and endoscopic intervention.” — Dr. Lena Torres, Internal Medicine Specialist
Diagnosis and What to Expect at the Doctor
If melena is suspected, your healthcare provider will likely begin with a thorough history and physical exam. They’ll ask about medication use, alcohol consumption, previous ulcers, and any family history of GI disorders.
Diagnostic tests may include:
- Fecal occult blood test (FOBT): Detects hidden blood in stool samples.
- Complete blood count (CBC): Checks for anemia, which may develop from chronic blood loss.
- Endoscopy (EGD): A camera-equipped tube examines the esophagus, stomach, and duodenum to locate the source of bleeding and potentially treat it during the procedure.
- Imaging studies: CT scans or capsule endoscopy may be used if the source isn’t found via standard endoscopy.
In some cases, patients are admitted to the hospital for observation, IV fluids, and blood transfusions if significant blood loss has occurred.
Step-by-Step: What You Should Do Now
If you’ve noticed black, tarry stools, follow this practical timeline to ensure your safety:
- Stop taking NSAIDs, aspirin, or other blood-thinning medications unless prescribed otherwise. Consult your doctor before discontinuing any prescription drug.
- Review your recent diet and supplements. Did you consume iron, bismuth, or large amounts of dark foods? Eliminate these and monitor stool changes.
- Check for other symptoms. Note any dizziness, weakness, abdominal pain, or vomiting.
- Contact your primary care physician within 24 hours. Even if you feel fine, melena warrants evaluation.
- Prepare for your appointment: Bring a list of medications, recent dietary habits, and a description of the stool (color, consistency, frequency).
- Follow through with recommended tests. Early detection improves outcomes significantly.
Prevention and Long-Term Management
Once the cause is identified and treated, preventing recurrence is key. Consider these strategies:
- Avoid excessive alcohol and tobacco, both of which irritate the stomach lining.
- Limits NSAID use. Opt for acetaminophen for pain relief when possible.
- Treat H. pylori infections completely with prescribed antibiotics.
- Manage stress, which can exacerbate acid production and ulcer formation.
- Eat a balanced diet rich in fiber and low in spicy or acidic foods if prone to gastritis.
Checklist: Actions to Take If You Have Black, Tarry Stool
- ✅ Assess recent food and supplement intake
- ✅ Stop unnecessary NSAIDs or blood thinners (with doctor approval)
- ✅ Monitor for dizziness, weakness, or vomiting
- ✅ Contact your doctor within 24 hours
- ✅ Prepare medication and symptom history
- ✅ Schedule or undergo recommended testing
Frequently Asked Questions
Can dehydration cause black stool?
No, dehydration does not directly cause black, tarry stool. However, it can concentrate waste and alter stool color slightly. True melena is due to digested blood and should not be attributed to hydration status alone.
Is black stool always a sign of cancer?
No. While gastrointestinal cancers can cause melena, they are less common than ulcers or gastritis. However, unexplained black stool—especially in individuals over 50—should be evaluated to rule out malignancy.
How long does it take for melena to resolve after treatment?
After successful treatment of the underlying cause, melena typically resolves within 3 to 7 days as the blood clears from the digestive tract. Persistent discoloration requires re-evaluation.
Conclusion: Don’t Ignore the Warning Sign
Black and tarry stool is more than a curious bathroom observation—it’s a potential indicator of internal bleeding that demands attention. While some causes are benign, others are urgent and even life-threatening. Recognizing the difference between harmless discoloration and true melena can save time, prevent complications, and protect your long-term health.
If you’re ever in doubt, err on the side of caution. Speak to a healthcare provider promptly, get the necessary tests, and take control of your digestive health. Your body is sending a message—listen to it.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?