The reproductive system is one of the most vital biological systems in the human body, not only for individual health but for the continuation of the species. Unlike other organ systems that focus primarily on sustaining life—such as the circulatory or respiratory systems—the reproductive system serves a broader evolutionary purpose: enabling procreation. Its importance extends beyond fertility, influencing hormonal balance, emotional well-being, and long-term physical development. Understanding its key functions helps individuals make informed decisions about their health, relationships, and medical care.
Core Functions of the Reproductive System
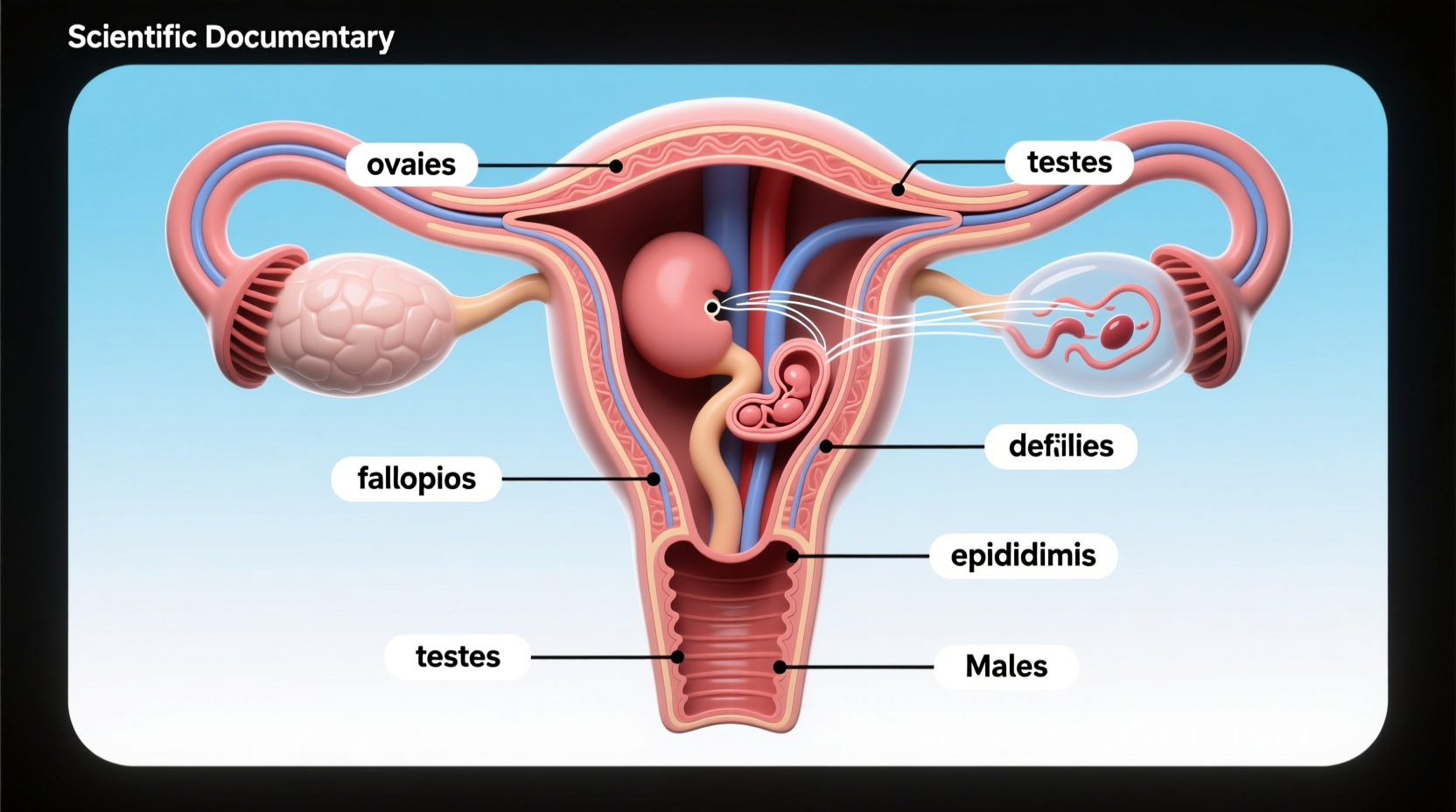
The reproductive system performs several essential roles that are critical from adolescence through adulthood. These functions differ slightly between males and females due to anatomical and physiological distinctions, but both systems work in harmony to ensure successful reproduction.
- Production of Gametes: The system produces sperm in males and ova (eggs) in females—specialized cells necessary for fertilization.
- Hormone Secretion: It regulates sex hormones such as testosterone, estrogen, and progesterone, which influence sexual development, mood, bone density, and metabolism.
- Fertilization Support: Female anatomy provides an environment conducive to sperm transport, egg release, and embryo implantation.
- Pregnancy and Childbirth: In females, the uterus supports fetal development, while hormonal shifts prepare the body for labor and lactation.
- Secondary Sexual Characteristics: During puberty, the reproductive system triggers changes like voice deepening, breast development, and body hair growth.
Role in Hormonal Regulation and Overall Health
Beyond reproduction, the endocrine activity of the reproductive organs significantly impacts general health. The ovaries and testes produce hormones that regulate more than just fertility—they influence cardiovascular function, cognitive performance, immune response, and mental health.
For example, estrogen contributes to maintaining healthy cholesterol levels and protecting bone density in women. Low estrogen during menopause increases the risk of osteoporosis and heart disease. Similarly, testosterone in men supports muscle mass, red blood cell production, and libido. Imbalances in these hormones can lead to fatigue, depression, weight gain, and metabolic issues.
“Reproductive health is not isolated—it's deeply interconnected with metabolic, psychological, and cardiovascular wellness.” — Dr. Lena Patel, Endocrinologist at Boston Women’s Health Center
Comparison of Male and Female Reproductive Functions
| Function | Male Reproductive System | Female Reproductive System |
|---|---|---|
| Gamete Production | Sperm produced continuously in testes after puberty | Ova formed before birth; released monthly after puberty |
| Hormones Produced | Testosterone, inhibin, small amounts of estrogen | Estrogen, progesterone, inhibin |
| Lifespan of Function | Can last into older age, though quality declines | Peak fertility until ~35; ends with menopause (~45–55) |
| Cyclic Activity | Minimal daily fluctuations | Regulated by 28-day menstrual cycle |
| Pregnancy Role | None | Supports gestation, childbirth, and breastfeeding |
Impact on Emotional and Social Well-being
The reproductive system also plays a subtle yet powerful role in emotional regulation and social behavior. Hormonal cycles affect mood, stress resilience, and interpersonal dynamics. For instance, premenstrual syndrome (PMS) and postpartum depression highlight how reproductive hormones directly influence brain chemistry.
Moreover, reproductive milestones—such as puberty, conception, infertility treatment, or menopause—often carry significant emotional weight. These transitions can shape identity, relationships, and personal goals. Recognizing this connection encourages a holistic approach to care, integrating medical, psychological, and lifestyle support.
Real-Life Example: Navigating Infertility Challenges
Sophia, a 34-year-old teacher, struggled with unexplained infertility for two years. Despite regular cycles and no known medical conditions, she and her partner couldn’t conceive. After consulting a reproductive endocrinologist, tests revealed mild hormonal imbalances affecting ovulation timing. With personalized medication and tracking methods, Sophia conceived within six months. Her experience underscores how understanding the reproductive system’s nuances—like subtle hormone shifts—can make a profound difference in achieving life goals.
Common Disorders and Prevention Strategies
Dysfunction in the reproductive system can arise from infections, genetic factors, lifestyle choices, or environmental exposures. Some prevalent conditions include polycystic ovary syndrome (PCOS), endometriosis, erectile dysfunction, and sexually transmitted infections (STIs).
Early detection and prevention are crucial. Consider the following checklist to maintain reproductive health:
- Get annual screenings (Pap smears, STI tests, prostate exams)
- Maintain a balanced diet rich in antioxidants and essential nutrients
- Avoid tobacco, excessive alcohol, and recreational drugs
- Exercise regularly to support circulation and hormone balance
- Manage stress through mindfulness or therapy
- Use protection during sexual activity to prevent STIs
Frequently Asked Questions
Why is the reproductive system important even if someone doesn’t want children?
The reproductive system regulates essential hormones that affect energy levels, skin health, bone strength, and emotional stability—even in individuals who do not plan to have children. Its proper function supports overall vitality throughout life.
Can lifestyle changes improve reproductive health?
Yes. Studies show that quitting smoking, reducing processed sugar intake, managing stress, and maintaining a healthy weight can improve fertility and hormonal balance in both men and women.
At what age should reproductive health monitoring begin?
Monitoring should start in adolescence. Girls should have their first gynecological visit between ages 13–15, while boys benefit from education about testicular self-exams and sexual health by age 14. Early awareness promotes lifelong wellness.
Step-by-Step Guide to Supporting Reproductive Wellness
- Assess Your Baseline: Schedule a check-up with a healthcare provider to evaluate hormone levels, organ health, and family history risks.
- Adopt a Fertility-Friendly Diet: Focus on whole grains, leafy greens, lean proteins, and healthy fats like omega-3s found in fish and flaxseeds.
- Track Biological Cycles: Use calendars or digital tools to monitor menstruation, cervical mucus, or basal body temperature if trying to conceive or avoid pregnancy naturally.
- Limit Toxin Exposure: Avoid plastics containing BPA, pesticides, and parabens in cosmetics, which may disrupt endocrine function.
- Seek Help When Needed: Don’t hesitate to consult specialists—reproductive endocrinologists, urologists, or therapists—if facing challenges related to fertility, pain, or sexual function.
Conclusion: Take Charge of Your Reproductive Health
The reproductive system is far more than a mechanism for producing offspring—it is central to hormonal equilibrium, emotional health, and long-term physical well-being. By understanding its key functions and respecting its complexity, individuals can take proactive steps toward better health at every stage of life. Whether you're entering puberty, planning a family, navigating midlife changes, or supporting a loved one, knowledge empowers action.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?