Feeling full long after eating, experiencing bloating, or noticing undigested food in your stool can be unsettling. When food seems to sit heavily in your stomach for hours without moving through the digestive tract, it’s more than discomfort—it may signal an underlying issue. Digestion is a complex process involving muscles, nerves, enzymes, and hormones. When any part falters, the result can be delayed gastric emptying, malabsorption, or functional gastrointestinal disorders. Understanding why your food isn’t digesting properly—and knowing what to do—can help you regain comfort and confidence in your digestive health.
Common Causes of Poor Digestion
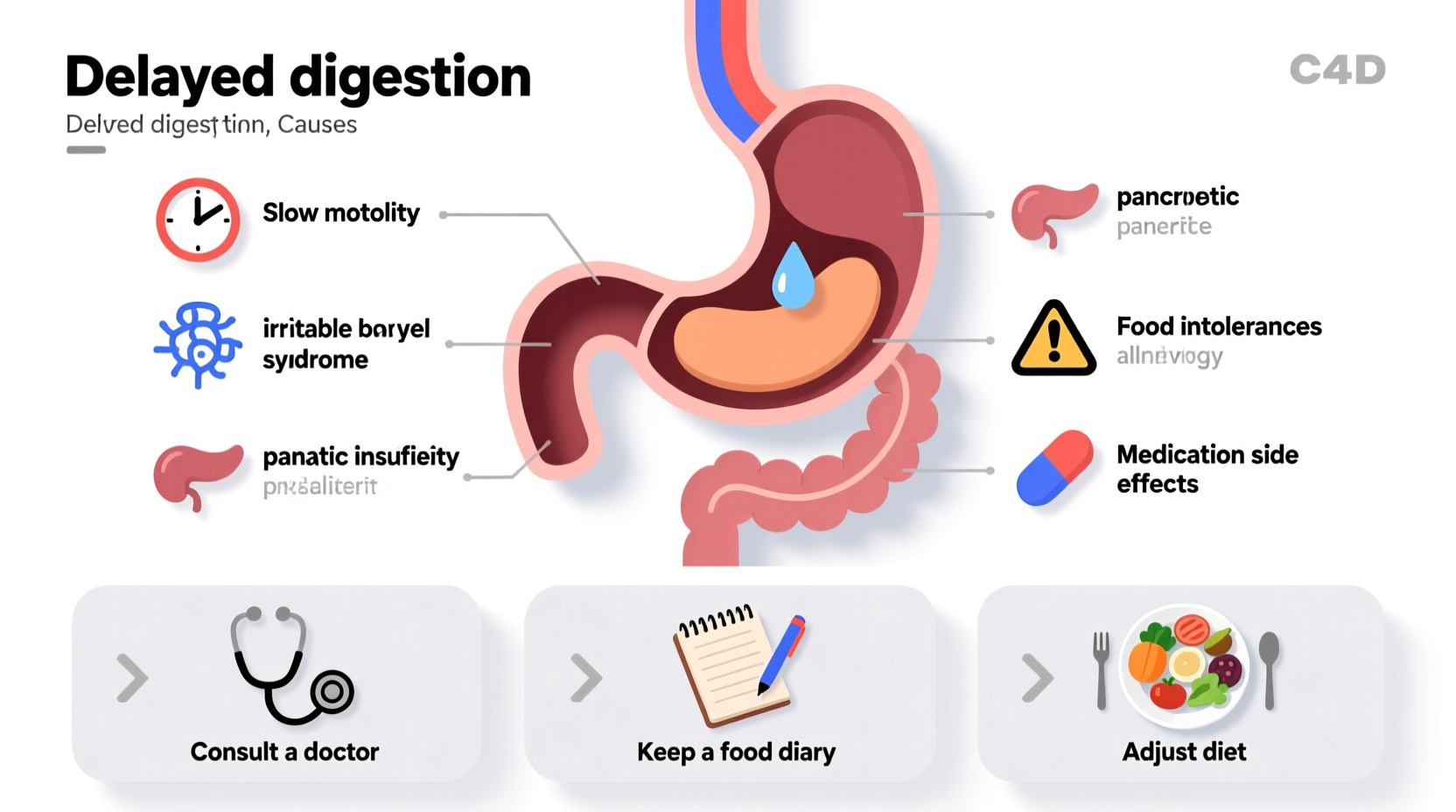
Digestive inefficiency rarely stems from a single factor. Instead, it often results from a combination of lifestyle habits, medical conditions, and physiological changes. Below are some of the most frequent contributors:
- Gastroparesis: A condition where the stomach empties too slowly due to nerve damage, often linked to diabetes or post-viral syndromes.
- Irritable Bowel Syndrome (IBS): Functional disorder affecting bowel motility and sensitivity, commonly causing bloating and irregular transit.
- Low stomach acid (hypochlorhydria): Insufficient hydrochloric acid impairs protein breakdown and enzyme activation.
- Enzyme deficiencies: Lactase deficiency (lactose intolerance), pancreatic insufficiency, or bile salt issues hinder nutrient breakdown.
- Slow motility: Caused by medications (opioids, antidepressants), hypothyroidism, or autonomic nervous system dysfunction.
- Dietary factors: High-fat meals, excessive fiber, or large portions overwhelm the digestive system.
- Stress and anxiety: Activate the sympathetic nervous system, reducing blood flow and motility in the gut.
Recognizing the Symptoms
Delayed digestion presents with a cluster of symptoms that go beyond occasional indigestion. Persistent signs include:
- Prolonged fullness after meals
- Nausea or vomiting undigested food hours after eating
- Bloating and abdominal distension
- Belching, gas, or heartburn
- Visible undigested food in stool (especially fibrous vegetables)
- Fluctuating blood sugar levels (in diabetics with gastroparesis)
While seeing corn or leafy greens intact in stool is normal due to their cellulose structure, widespread undigested food—especially proteins or starches—warrants attention.
“Persistent digestive stalling isn’t just inconvenient—it can lead to malnutrition, bacterial overgrowth, and worsening gut-brain communication.” — Dr. Lena Patel, Gastroenterologist
What You Can Do: A Step-by-Step Guide
Improving digestion requires both immediate adjustments and long-term strategies. Follow this timeline to address root causes and promote healthy motility.
- Day 1–3: Modify Eating Habits
- Reduce meal size to 1–2 cups per sitting.
- Chew each bite thoroughly (20–30 times).
- Avoid drinking large fluids during meals to prevent stomach dilution.
- Week 1: Track and Adjust Diet
- Keep a food and symptom journal.
- Limit high-fat, fried, and processed foods.
- Temporarily reduce insoluble fiber (raw veggies, bran) if bloating is severe.
- Week 2–4: Support Digestion Naturally
- Take apple cider vinegar (1 tbsp in water) before meals to boost stomach acid.
- Try digestive enzyme supplements with meals, especially if eating protein or dairy.
- Incorporate ginger tea or peppermint after eating to stimulate motility.
- Month 2: Address Underlying Conditions
- Consult a healthcare provider for blood tests (thyroid, glucose, inflammation markers).
- Consider breath testing for SIBO (Small Intestinal Bacterial Overgrowth).
- Discuss gastric emptying studies if symptoms persist.
Do’s and Don’ts: Quick Reference Table
| Do | Don’t |
|---|---|
| Eat slowly and chew food well | Wolf down meals under stress |
| Choose cooked over raw vegetables when symptomatic | Consume large salads with tough greens |
| Stay hydrated between meals | Drink large amounts of liquid during meals |
| Move gently after eating (short walk) | Lie down immediately after meals |
| Use probiotics if tolerated | Overuse antacids without medical advice |
Real-Life Example: Maria’s Journey with Gastroparesis
Maria, a 45-year-old teacher with type 2 diabetes, began feeling full within minutes of eating, even small meals. She’d often vomit dinner hours later and lost weight unintentionally. Her primary care doctor suspected gastroparesis. After a gastric emptying study confirmed delayed motility, Maria worked with a dietitian to adopt a low-residue, soft-food diet. She started taking prescribed prokinetic medication and used digestive enzymes with meals. Within six weeks, her symptoms improved significantly. By managing her blood sugar consistently and prioritizing meal timing, she regained nutritional stability and daily comfort.
When to See a Doctor
While mild digestive discomfort is common, certain red flags require prompt medical evaluation:
- Unintentional weight loss
- Frequent vomiting, especially of undigested food
- Severe abdominal pain not relieved by passing gas or bowel movements
- Anemia or fatigue suggesting malabsorption
- Symptoms lasting more than two weeks despite dietary changes
A gastroenterologist may recommend endoscopy, imaging, or motility testing to rule out structural issues, ulcers, or chronic conditions like Crohn’s disease or celiac disease.
FAQ
Can stress really affect digestion?
Yes. The gut and brain are closely connected via the vagus nerve. Chronic stress suppresses digestive secretions and slows motility, leading to bloating, constipation, or reflux. Mind-body practices like deep breathing or meditation before meals can activate the parasympathetic nervous system and improve digestion.
Is it normal to see undigested food in stool?
Sometimes. Certain foods like corn, seeds, and raw vegetables have outer layers made of cellulose, which humans lack the enzymes to break down. As long as this is occasional and not accompanied by diarrhea, pain, or weight loss, it’s typically harmless.
Are digestive enzymes safe to take daily?
For most people, over-the-counter digestive enzymes are safe when taken with meals. However, they’re not a substitute for diagnosing underlying issues. Long-term use should be discussed with a healthcare provider, especially if you have pancreatic conditions or are on other medications.
Final Steps Toward Better Digestion
Your digestive system thrives on consistency, quality input, and mindful habits. Start by simplifying meals, chewing thoroughly, and observing how your body responds. Small shifts—like avoiding late-night eating or reducing processed fats—can yield significant improvements. If symptoms persist, don’t dismiss them as “just indigestion.” Early intervention prevents complications and supports long-term gut health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?