For many couples struggling with infertility, in vitro fertilization (IVF) offers a beacon of hope. Yet, despite advances in reproductive medicine, IVF does not guarantee success. In fact, a significant number of cycles end without a live birth. Understanding why IVF fails is crucial—not to assign blame, but to empower patients with knowledge, improve outcomes, and guide future decisions. While some factors are beyond control, others can be addressed through medical intervention or lifestyle adjustments.
Embryo Quality: The Foundation of Success
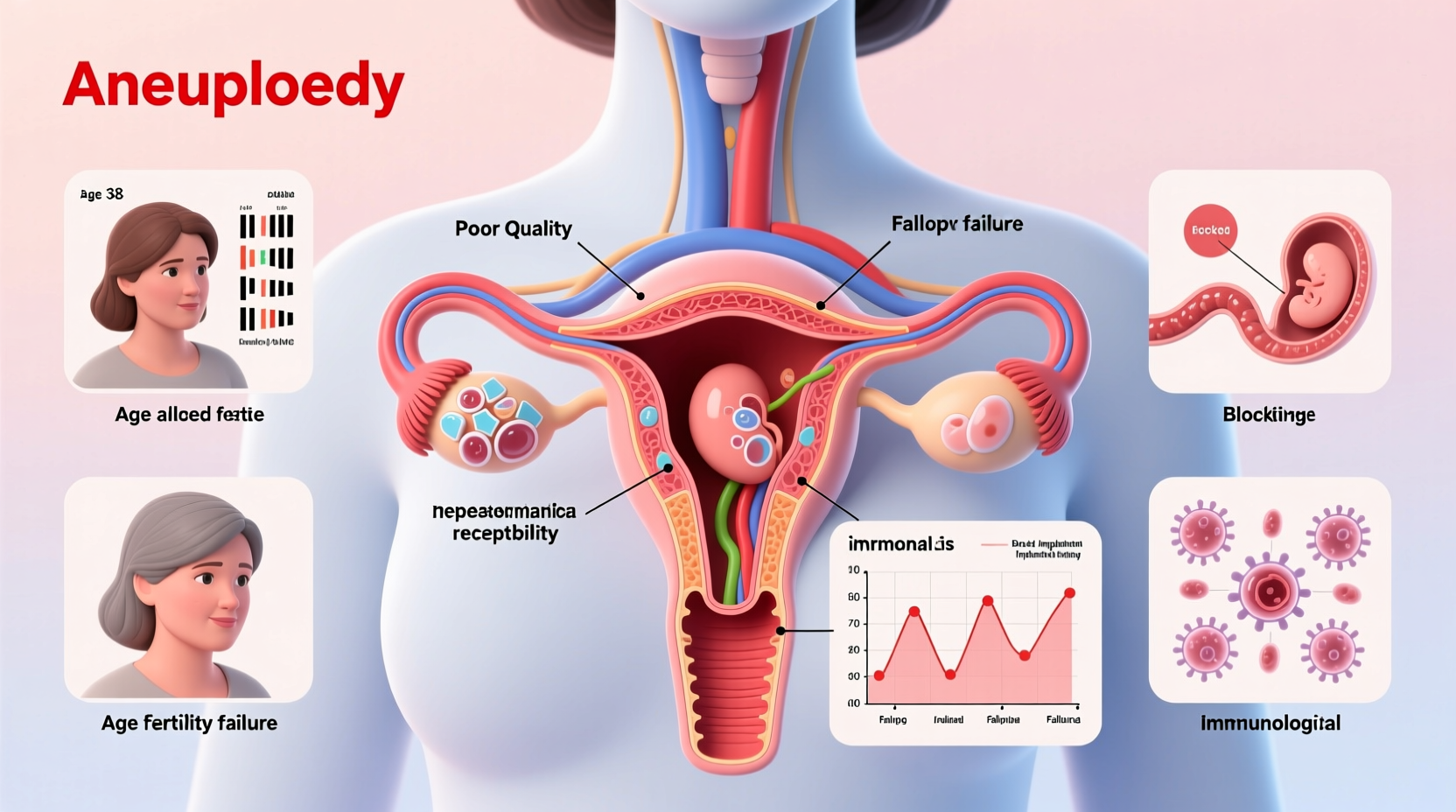
The quality of embryos plays the most decisive role in IVF success. Even when fertilization occurs, not all embryos develop into viable blastocysts capable of implanting in the uterine lining. Chromosomal abnormalities—often due to errors in egg or sperm cell division—are a leading cause of poor embryo development. These abnormalities increase with maternal age, particularly after 35, due to declining egg quality.
Many embryos with chromosomal issues (aneuploidy) either fail to implant, result in early miscarriage, or do not progress beyond early developmental stages. Preimplantation genetic testing for aneuploidy (PGT-A) can help identify chromosomally normal embryos, improving selection accuracy. However, PGT-A is not foolproof and may not be recommended for all patients.
Uterine and Endometrial Factors
An embryo may be genetically perfect, yet still fail to implant due to issues within the uterus. The endometrial lining must be receptive during a specific window known as the \"window of implantation.\" If the lining is too thin (typically less than 7mm), scarred, or inflamed, it may not support embryo attachment.
Conditions such as endometriosis, fibroids, polyps, or adenomyosis can distort the uterine cavity or create a hostile environment for implantation. Chronic endometritis—an often silent infection of the endometrium—can also impair receptivity and is frequently undiagnosed until repeated IVF failures occur.
“Even with excellent embryos, implantation cannot occur without a receptive endometrium. We now recognize that uterine factors contribute to up to 10–15% of unexplained IVF failures.” — Dr. Lena Patel, Reproductive Endocrinologist
Common Uterine Issues Affecting Implantation
- Thin endometrial lining
- Intrauterine adhesions (Asherman’s syndrome)
- Submucosal fibroids distorting the cavity
- Endometrial polyps
- Chronic inflammation or infection
Age and Ovarian Reserve
Female age remains the strongest predictor of IVF success. As women age, both the quantity and quality of eggs decline. By age 40, only about 10–20% of a woman’s remaining eggs are chromosomally normal. This directly impacts fertilization rates, embryo development, and pregnancy sustainability.
Ovarian reserve—the number of viable eggs remaining—is assessed through blood tests (AMH, FSH) and ultrasound (antral follicle count). Low ovarian reserve means fewer eggs retrieved per cycle, reducing the chances of obtaining at least one high-quality embryo.
While men’s fertility declines more gradually, advanced paternal age (over 45) has been linked to increased DNA fragmentation in sperm, which can affect embryo quality and raise miscarriage risk.
Impact of Age on IVF Success Rates (Live Birth per Cycle)
| Age Group | Success Rate |
|---|---|
| Under 35 | ~40–50% |
| 35–37 | ~30–35% |
| 38–40 | ~20–25% |
| 41–42 | ~10–15% |
| Above 42 | <5% |
Lifestyle and Environmental Influences
While medical factors dominate IVF discussions, lifestyle choices exert measurable influence. Smoking, excessive alcohol consumption, obesity, and high stress levels have all been associated with reduced IVF success.
Smoking damages egg and sperm DNA, reduces ovarian response, and impairs blood flow to the uterus. Obesity alters hormone balance, affects ovulation, and increases inflammation—negatively impacting both embryo quality and implantation. Conversely, being underweight can disrupt menstrual cycles and reduce fertility.
Certain environmental toxins—including BPA (found in plastics), pesticides, and heavy metals—may interfere with hormonal signaling and reproductive function. Though research is ongoing, minimizing exposure is a prudent step.
Steps to Optimize Lifestyle Before IVF
- Quit smoking and avoid secondhand smoke
- Maintain a healthy BMI (18.5–24.9)
- Limit alcohol and caffeine intake
- Adopt a Mediterranean-style diet rich in antioxidants
- Engage in moderate exercise (e.g., walking, yoga)
- Practice stress-reduction techniques like mindfulness or acupuncture
Unexplained IVF Failure and Immune Factors
Sometimes, despite optimal embryo quality, a receptive uterus, and no identifiable medical issues, IVF still fails. This is termed “unexplained IVF failure.” Emerging research suggests immune system dysregulation may play a role. In rare cases, the body may mount an abnormal immune response against the embryo, treating it as a foreign invader.
Some clinics offer immune testing and treatments such as intravenous immunoglobulin (IVIG) or corticosteroids, though evidence supporting these interventions remains limited and controversial. These should only be considered in clinical trials or under strict specialist supervision.
Mini Case Study: Repeated Implantation Failure
Sarah, 37, underwent three IVF cycles using her own eggs. Each time, high-quality blastocysts were transferred, yet none resulted in pregnancy. Testing revealed chronic endometritis, likely stemming from a prior asymptomatic pelvic infection. After a course of antibiotics and a hysteroscopic removal of minor adhesions, her fourth cycle led to a successful pregnancy and the birth of a healthy baby girl. This case underscores the importance of investigating subtle uterine conditions after repeated failures.
FAQ: Common Questions About IVF Failure
Why did my IVF fail even with good-quality embryos?
Even morphologically excellent embryos may carry undetected chromosomal abnormalities. Additionally, timing of transfer, endometrial receptivity, and subtle immune or metabolic factors can prevent implantation. Sometimes, the reason remains unknown despite thorough evaluation.
How many IVF cycles should I try before considering other options?
Most specialists recommend evaluating results after 3–4 fresh or frozen embryo transfers, especially if no pregnancies occur. At that point, a comprehensive review of protocols, potential underlying causes, and alternative paths—such as donor gametes or surrogacy—should be discussed.
Can stress cause IVF to fail?
While acute stress alone is unlikely to directly cause IVF failure, chronic stress may influence hormonal balance and behaviors (like poor sleep or diet) that indirectly affect outcomes. Managing emotional well-being through counseling or support groups is encouraged for overall resilience.
Action Plan After IVF Failure
Experiencing IVF failure can be emotionally devastating, but it doesn’t mean future success is impossible. A structured approach can help clarify next steps:
- Request a full cycle review with your doctor
- Review embryo grading, stimulation protocol, and lab reports
- Assess uterine health via sonohysterogram or hysteroscopy
- Test for immune or thrombophilia markers if indicated
- Reevaluate lifestyle habits and make necessary changes
- Consider a second opinion from another fertility specialist
- Allow time for emotional recovery before starting again
Conclusion
IVF failure is a complex outcome influenced by biological, medical, and sometimes emotional factors. While not every reason can be controlled, understanding the common causes—embryo quality, uterine health, age, lifestyle, and unexplained elements—empowers patients to make informed decisions. With each cycle, valuable data is gathered that can refine future attempts. Persistence, paired with expert guidance and self-care, often leads to eventual success. If you’ve faced IVF failure, know you’re not alone—and there is still hope.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?