A pacemaker is a small, implanted medical device designed to help regulate abnormal heart rhythms—specifically those that are too slow (bradycardia) or irregular. While the idea of having a device inside your body may sound daunting, pacemakers are among the most common and effective treatments for certain cardiac conditions. Millions of people live active, healthy lives with pacemakers, often experiencing dramatic improvements in energy, stamina, and overall well-being. Understanding why someone might need a pacemaker, recognizing the symptoms of underlying heart rhythm disorders, and knowing when to seek care can make all the difference in long-term outcomes.
How the Heart’s Electrical System Works
The heart relies on a precise electrical system to maintain a steady, effective rhythm. With each heartbeat, an electrical impulse begins in the sinoatrial (SA) node—the heart’s natural pacemaker—located in the right atrium. This signal spreads through the atria, causing them to contract and push blood into the ventricles. The impulse then passes through the atrioventricular (AV) node and down specialized pathways, triggering ventricular contraction and pumping blood to the lungs and body.
When this system malfunctions—due to aging, disease, or injury—the heart may beat too slowly, too quickly, or irregularly. In cases where the rhythm is dangerously slow or pauses occur, a pacemaker becomes essential to restore proper function.
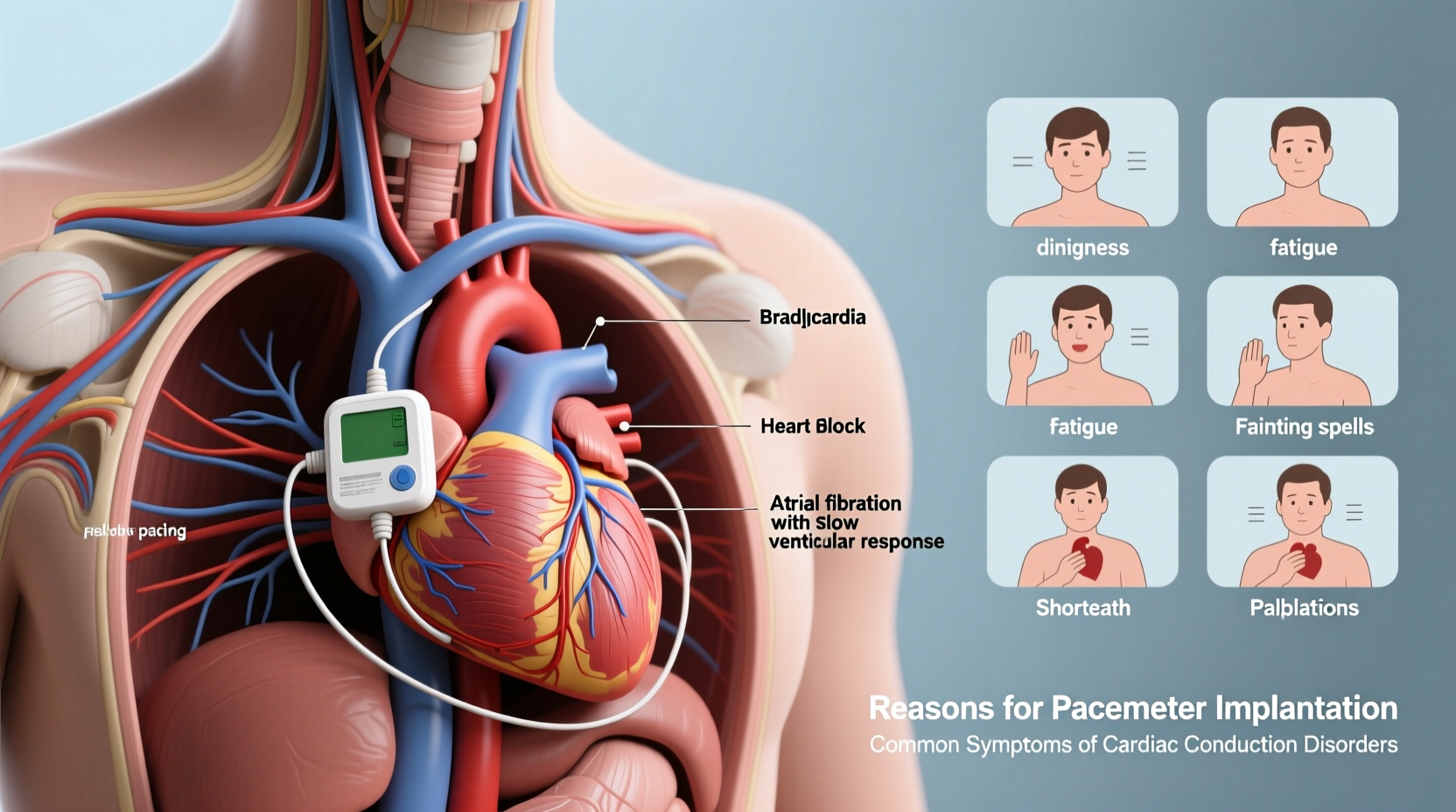
Common Reasons You Might Need a Pacemaker
Pacemakers are primarily used to treat bradycardia, but they also support treatment for several other heart-related conditions. Below are the most frequent medical reasons a doctor may recommend implantation:
- Sick Sinus Syndrome: A condition where the SA node fails to generate impulses properly, leading to alternating slow and fast heart rates.
- Heart Block: A disruption in the electrical signal between the atria and ventricles. This can be first-degree (mild), second-degree (intermittent), or third-degree (complete), with the latter almost always requiring a pacemaker.
- Post-Heart Attack Complications: Damage from a heart attack can impair the heart’s electrical pathways, especially if the conduction system is affected.
- Heart Failure with Conduction Delays: Some patients with weakened hearts benefit from biventricular pacemakers (also called cardiac resynchronization therapy) that help both sides of the heart pump in sync.
- Long QT Syndrome or Other Arrhythmias: Though less common, some inherited rhythm disorders may require pacing as part of a broader treatment plan.
- Side Effects from Medications: Certain drugs, such as beta-blockers or calcium channel blockers, can excessively slow the heart rate in sensitive individuals.
“Pacemakers don’t cure heart disease, but they do correct life-limiting rhythm problems. For many patients, it means going from being housebound to walking their dog again.” — Dr. Lena Patel, Electrophysiologist, Cleveland Clinic
Symptoms That May Indicate a Need for a Pacemaker
Not everyone with a heart rhythm disorder experiences obvious symptoms, but when they do appear, they often reflect inadequate blood flow due to a slow or erratic heartbeat. Key warning signs include:
- Fatigue, even after adequate rest
- Dizziness or lightheadedness
- Fainting (syncope) or near-fainting episodes
- Shortness of breath during routine activities
- Chest pain or discomfort
- Irregular or unusually slow pulse
- Difficulty exercising or reduced stamina
These symptoms may come and go, making them easy to overlook. However, unexplained fainting spells or recurrent dizziness should prompt immediate evaluation by a cardiologist. Diagnostic tools like electrocardiograms (ECGs), Holter monitors, and event recorders help capture intermittent rhythm disturbances over time.
What to Expect: Diagnosis and Implantation Process
If a doctor suspects a rhythm disorder, the diagnostic process typically begins with a physical exam and ECG. If results are inconclusive, a 24- to 48-hour Holter monitor may be prescribed. For infrequent symptoms, an event recorder worn for weeks can detect abnormalities when symptoms occur.
Once a significant bradyarrhythmia is confirmed, and symptoms correlate with the rhythm issue, a pacemaker may be recommended. The implantation procedure is minimally invasive and usually performed under local anesthesia:
- You’ll receive a sedative to help you relax.
- The area below the collarbone is numbed, and a small incision is made.
- One or more insulated wires (leads) are threaded through a vein into the heart chambers.
- The leads are connected to the pacemaker generator, which is placed under the skin.
- The device is tested to ensure proper function before closing the incision.
Most patients go home within 24 hours and resume light activity within a few days. Full recovery takes about 4–6 weeks, during which arm movement on the implant side is limited to prevent lead displacement.
Types of Pacemakers and Their Uses
Not all pacemakers are the same. The type recommended depends on the nature of the heart rhythm problem and the patient’s overall health.
| Type | Chambers Paced | Best For |
|---|---|---|
| Single-Chamber | One (usually right ventricle) | Patients with AV block and normal atrial function |
| Dual-Chamber | Two (right atrium and right ventricle) | Mimics natural rhythm; ideal for sick sinus syndrome |
| Biventricular (CRT-P) | Three (both ventricles + atrium) | Heart failure patients with electrical delays |
| Leadless Pacemaker | One (right ventricle only) | Minimally invasive option for select bradycardia cases |
Advances in technology have led to smaller devices, longer battery life (typically 8–15 years), and remote monitoring capabilities that allow doctors to track device performance without office visits.
Mini Case Study: Recovering Quality of Life
James, a 72-year-old retired teacher, began experiencing frequent dizziness and fatigue while gardening. Initially, he attributed it to age and dehydration. After fainting while standing in line at the grocery store, he visited his primary care physician. An ECG showed third-degree heart block with a heart rate dipping to 38 bpm. He was referred to a cardiologist and fitted with a dual-chamber pacemaker within two weeks. Within days, James reported feeling “like himself again.” Six months later, he resumed hiking with his grandchildren—something he hadn’t done in over a year.
Lifestyle After Pacemaker Implantation
Most patients return to normal activities within a few weeks. Modern pacemakers are designed to adapt to physical exertion, increasing heart rate during exercise. However, certain precautions apply:
- Avoid strong magnetic fields (e.g., MRI machines unless device is MRI-compatible).
- Inform airport security about your device; handheld wands should not linger over the implant site.
- Keep cell phones at least 6 inches away from the pacemaker (use the ear opposite the implant).
- Notify all healthcare providers about your device before any procedure.
FAQ
Can a pacemaker cure my heart condition?
No, a pacemaker does not cure heart disease. Instead, it manages symptoms by ensuring your heart maintains an adequate rhythm. Underlying conditions still require ongoing medical management.
Will I feel the pacemaker once it's implanted?
Initially, you may feel a lump under the skin, and there might be mild soreness for a few weeks. Most people stop noticing the device over time. You won’t feel the electrical impulses it delivers.
How often will my pacemaker need checking?
Follow-up visits are typically scheduled every 3–6 months. Many systems now offer wireless monitoring, allowing your doctor to review data remotely every few weeks.
Conclusion
Recognizing the symptoms of a slow or irregular heartbeat—and understanding the reasons you might need a pacemaker—can be life-saving. From unexplained fatigue to fainting spells, these signs should never be ignored. Thanks to modern medicine, pacemakers offer a safe, effective solution that restores rhythm, energy, and independence. If you or a loved one are experiencing symptoms of a heart rhythm disorder, consult a cardiologist promptly. Early diagnosis and treatment can transform your quality of life.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?